Incidental finding of an appendiceal mucocele [August 2025]
November 21, 2025
The Double Aorta Artifact: A Benign Trap in Abdominal Sonography [October 2025]
December 8, 2025SUBMIT YOUR CASE
EFSUMB invites submission of interesting cases for the website section 'Case of the Month'. All CoM submissions are eligible for selection for free registration at the next Euroson congress. Two cases that receive the most 'likes' in a year will receive free registration for the next EUROSON congress and the third most liked liked case will receive a cash prize of 100 EUR.
Rare Multinodular Epithelioid Malignant Mesothelioma of the Tunica Vaginalis
Authors:
Chidi Uchenna Ollawa (Sonographer/Researcher), Ernest Ruto Upeh (Advanced Practice Sonographer), Eyo Akpan (Advanced Practice Sonographer), Yannick Yangue (Consultant Radiologist), Ruchi Nasa (Consultant Histopathologist)Affiliation:
Cumberland Infirmary, North Cumbria Integrated Care NHS Foundation Trust1Clinical History
Chronic hydrocele, painless swelling x 12/52. 69 years old male with no history of asbestos exposure.
2Image Findings
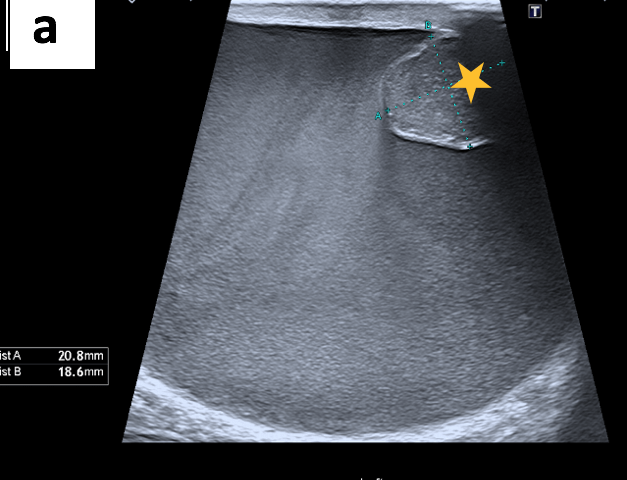
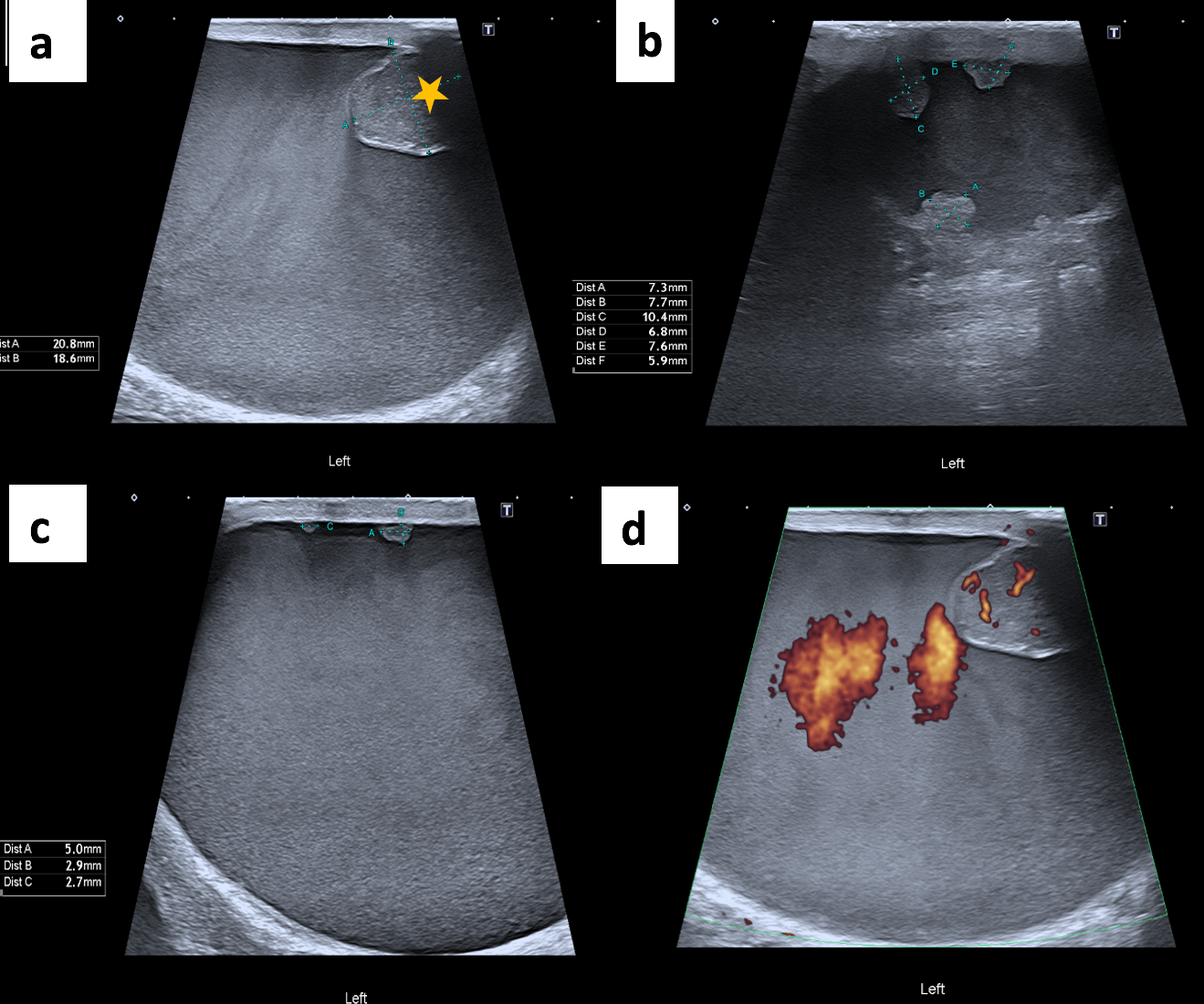
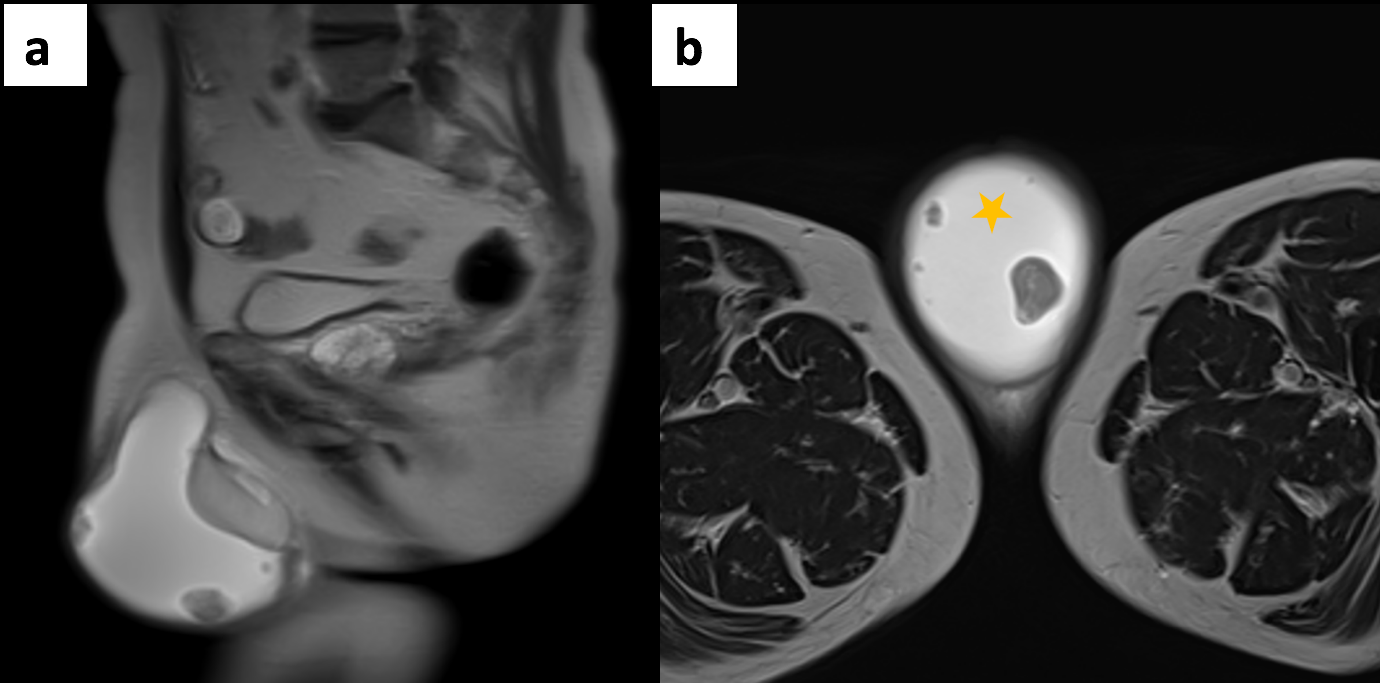
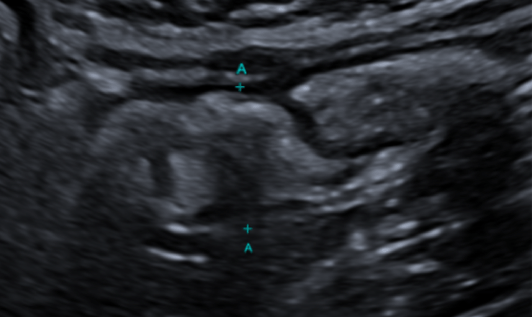
The ultrasound scan revealed turbid fluid with internal echoes and multiple hypoechoic, nodular, excrescences/adherent lesions on the tunica vaginalis. MRI scan was unremarkable.
3Diagnosis
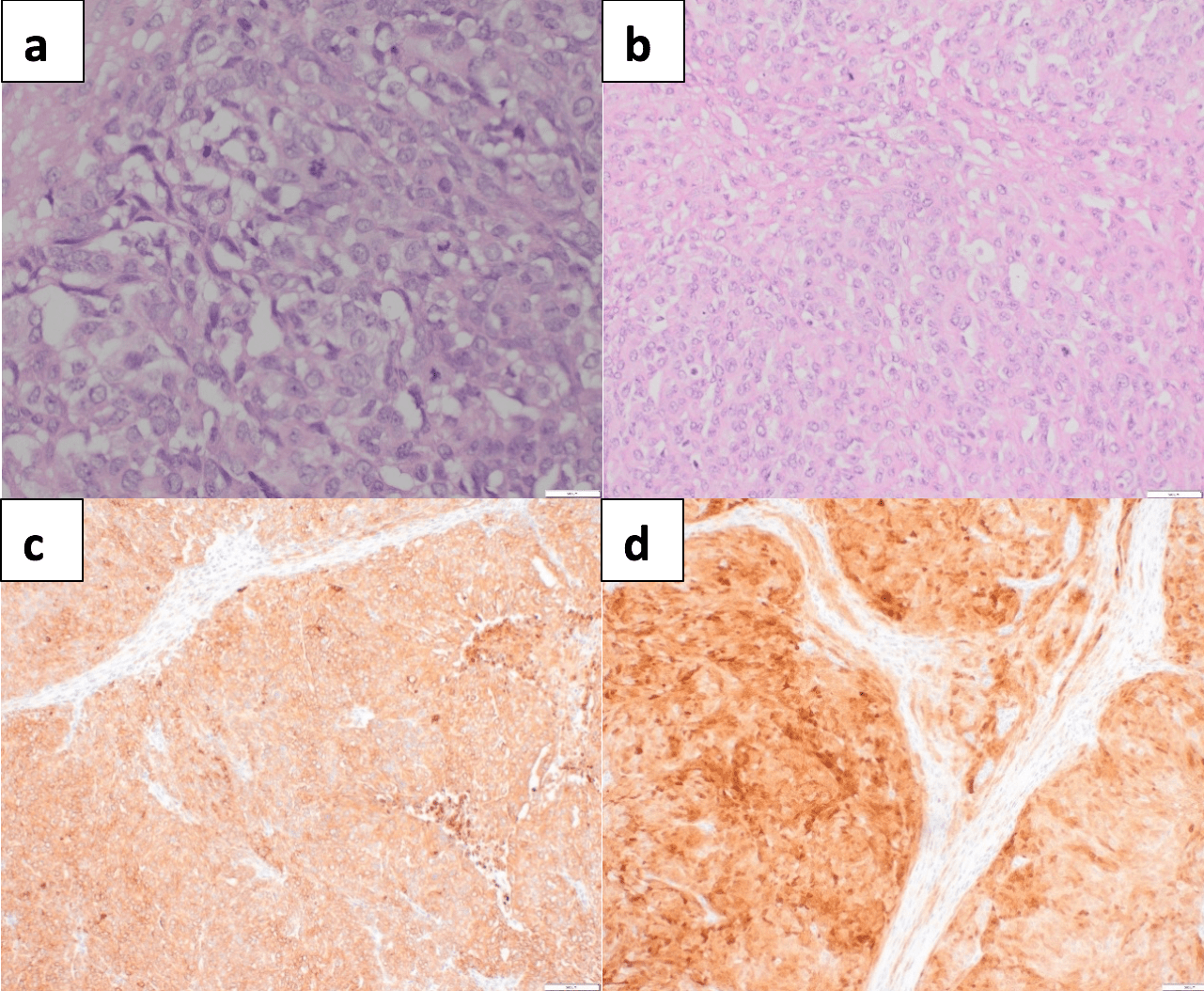
Histopathology and immunohistochemistry confirmed a malignant epithelioid neoplasm that was positive for Pan-CK (AE1/3, calretinin, WT1, vimentin, CK5/6, CK7 and BerEP4).
4Discussion
● Background
Malignant mesothelioma is a rare, aggressive cancer that affects the mesothelial cells lining the pleural, peritoneal, and pericardial cavities and the tunica vaginalis. Mesotheliomas of the tunica vaginalis (MMTVs) account for 1–3% of all mesotheliomas and originate from mesothelial cells in this area. Within the scrotum, the visceral layer of the tunica vaginalis serves as the outer covering of the tunica albuginea, which encases the testes. The parietal layer of the tunica vaginalis is proximal to the scrotal wall muscles, fascia and skin. This leaves potential space between the tunica layers to accommodate fluid build-up. Hydrocele is characterised by fluid accumulation between the visceral and parietal layers of the tunica vaginalis, leading to scrotal swelling. This condition can arise from various aetiologies, including trauma, infection or idiopathic causes.
● Clinical perspective
Globally, fewer than 100 cases of MMTV have been reported in the available literature, emphasising its rarity. In the UK, according to Cancer Research, mesothelioma incidence rates in females have increased by nearly 90% since the early 1990s, whereas rates in males rose by more than 40% from 2017 to 2019. Most mesothelioma cases are linked to asbestos exposure, although some patients have no known history of exposure. The connection between asbestos and tunica vaginalis mesothelioma is particularly unclear, indicating that other factors may contribute to its development in this location.
Diagnoses of tunica vaginalis mesothelioma often occur incidentally during surgeries for other scrotal conditions. The uncommon nature of the condition further complicates the collection of comprehensive epidemiological data and contributes to the lack of standardised diagnostic and treatment protocols. The diagnosis of MMTV presents challenges due to nonspecific clinical manifestations, such as hydrocele or a painless scrotal mass. These symptoms are also common in several benign conditions, which may lead to delays in diagnosis and further investigation. Despite its rarity, MMTV shares similar clinical, histological, and molecular characteristics with mesotheliomas found at other sites, including epithelioid and biphasic morphologies, as well as gene mutations, such as NF2 and TP532. A vague clinical picture often necessitates a thorough diagnostic approach.
Ultrasound is the primary imaging modality used to assess scrotal swelling or potential tumours. This is due to its easy availability, use of non-ionising radiation, cost-effectiveness and real-time features. However, ultrasound is highly operator-dependent and, therefore, requires adequate training. Other modalities, such as magnetic resonance imaging (MRI) or computed tomography (CT), can be considered when ultrasound findings are equivocal. Histology analysis of surgically removed (or biopsied) scrotal tumours is the gold standard for diagnosis. Although rare, tumours of the tunica vaginalis include fibrous pseudotumours and malignant mesotheliomas. They both primarily affect middle-aged men and are characterised by painless nodules and scrotal enlargement. The common sonographic appearance suggestive of MMTV includes the presence of singular or multiple painless nodules/excrescences in the tunica vaginalis with hydrocele. The diagnosis in this case was confirmed through orchiectomy followed by histopathology and immunochemistry.
In cases of pleural mesothelioma, ultrasound-guided percutaneous needle biopsy has shown high sensitivity (83.39%) and specificity (100%) for diagnosing malignant mesothelioma. Based on the findings from pleural mesothelioma and general imaging principles, ultrasound is highly sensitive but has limited specificity. Therefore, the authors recommend that sonographers could receive adequate training to enhance or advance their practice in fine needle aspiration cytology and ultrasound-guided biopsy of nodules of the tunica vaginalis within a one-stop rapid-access clinic to expedite the diagnosis of MMTV. This will ensure the collection of comprehensive epidemiological data and contribute to the standardisation of diagnostic and treatment protocols for MMTV. Conversely, the sensitivity and specificity of CT and MRI in diagnosing malignant mesothelioma of the tunica vaginalis have not been well established. However, CT and MRI offer complementary advantages in staging and assessing local invasion. Further research is needed to determine the diagnostic accuracy of these modalities, specifically for MMTV.
● Therapy planning
The primary treatment for MMTV is radical orchiectomy, which is often supplemented by adjuvant therapy in aggressive or metastatic cases.
● Outcome
Final diagnosis made was epithelioid malignant mesothelioma of the tunica vaginalis. Patient has had a follow up CT scan of the thorax, abdomen and pelvis which were unremarkable.
● Prognosis
The prognosis is poor and varies significantly, with five-year survival rates ranging between 30% and 50%, further emphasising the need for ongoing research into more effective treatment options. Therefore, increasing the degree of clinical suspicion in high-risk patients and achieving the right result during an initial scrotal ultrasound examination may improve the MMTV prognosis.
Malignant mesothelioma is a rare, aggressive cancer that affects the mesothelial cells lining the pleural, peritoneal, and pericardial cavities and the tunica vaginalis. Mesotheliomas of the tunica vaginalis (MMTVs) account for 1–3% of all mesotheliomas and originate from mesothelial cells in this area. Within the scrotum, the visceral layer of the tunica vaginalis serves as the outer covering of the tunica albuginea, which encases the testes. The parietal layer of the tunica vaginalis is proximal to the scrotal wall muscles, fascia and skin. This leaves potential space between the tunica layers to accommodate fluid build-up. Hydrocele is characterised by fluid accumulation between the visceral and parietal layers of the tunica vaginalis, leading to scrotal swelling. This condition can arise from various aetiologies, including trauma, infection or idiopathic causes.
● Clinical perspective
Globally, fewer than 100 cases of MMTV have been reported in the available literature, emphasising its rarity. In the UK, according to Cancer Research, mesothelioma incidence rates in females have increased by nearly 90% since the early 1990s, whereas rates in males rose by more than 40% from 2017 to 2019. Most mesothelioma cases are linked to asbestos exposure, although some patients have no known history of exposure. The connection between asbestos and tunica vaginalis mesothelioma is particularly unclear, indicating that other factors may contribute to its development in this location.
Diagnoses of tunica vaginalis mesothelioma often occur incidentally during surgeries for other scrotal conditions. The uncommon nature of the condition further complicates the collection of comprehensive epidemiological data and contributes to the lack of standardised diagnostic and treatment protocols. The diagnosis of MMTV presents challenges due to nonspecific clinical manifestations, such as hydrocele or a painless scrotal mass. These symptoms are also common in several benign conditions, which may lead to delays in diagnosis and further investigation. Despite its rarity, MMTV shares similar clinical, histological, and molecular characteristics with mesotheliomas found at other sites, including epithelioid and biphasic morphologies, as well as gene mutations, such as NF2 and TP532. A vague clinical picture often necessitates a thorough diagnostic approach.
Ultrasound is the primary imaging modality used to assess scrotal swelling or potential tumours. This is due to its easy availability, use of non-ionising radiation, cost-effectiveness and real-time features. However, ultrasound is highly operator-dependent and, therefore, requires adequate training. Other modalities, such as magnetic resonance imaging (MRI) or computed tomography (CT), can be considered when ultrasound findings are equivocal. Histology analysis of surgically removed (or biopsied) scrotal tumours is the gold standard for diagnosis. Although rare, tumours of the tunica vaginalis include fibrous pseudotumours and malignant mesotheliomas. They both primarily affect middle-aged men and are characterised by painless nodules and scrotal enlargement. The common sonographic appearance suggestive of MMTV includes the presence of singular or multiple painless nodules/excrescences in the tunica vaginalis with hydrocele. The diagnosis in this case was confirmed through orchiectomy followed by histopathology and immunochemistry.
In cases of pleural mesothelioma, ultrasound-guided percutaneous needle biopsy has shown high sensitivity (83.39%) and specificity (100%) for diagnosing malignant mesothelioma. Based on the findings from pleural mesothelioma and general imaging principles, ultrasound is highly sensitive but has limited specificity. Therefore, the authors recommend that sonographers could receive adequate training to enhance or advance their practice in fine needle aspiration cytology and ultrasound-guided biopsy of nodules of the tunica vaginalis within a one-stop rapid-access clinic to expedite the diagnosis of MMTV. This will ensure the collection of comprehensive epidemiological data and contribute to the standardisation of diagnostic and treatment protocols for MMTV. Conversely, the sensitivity and specificity of CT and MRI in diagnosing malignant mesothelioma of the tunica vaginalis have not been well established. However, CT and MRI offer complementary advantages in staging and assessing local invasion. Further research is needed to determine the diagnostic accuracy of these modalities, specifically for MMTV.
● Therapy planning
The primary treatment for MMTV is radical orchiectomy, which is often supplemented by adjuvant therapy in aggressive or metastatic cases.
● Outcome
Final diagnosis made was epithelioid malignant mesothelioma of the tunica vaginalis. Patient has had a follow up CT scan of the thorax, abdomen and pelvis which were unremarkable.
● Prognosis
The prognosis is poor and varies significantly, with five-year survival rates ranging between 30% and 50%, further emphasising the need for ongoing research into more effective treatment options. Therefore, increasing the degree of clinical suspicion in high-risk patients and achieving the right result during an initial scrotal ultrasound examination may improve the MMTV prognosis.
5Teaching Points
1. Multinodular malignant mesothelioma of the tunica vaginalis (MMTV) is a rare morphological subtype scarcely described in the literature.
2. Absence of asbestos exposure does not rule out MMTV.
3. Chronic complex hydrocele may mask aggressive malignancy and should not be assumed benign.
4. Detailed ultrasound evaluation of the tunica vaginalis for all cases of chronic hydrocele and early MDT involvement is critical for ruling out MMTV and for favourable outcomes.
2. Absence of asbestos exposure does not rule out MMTV.
3. Chronic complex hydrocele may mask aggressive malignancy and should not be assumed benign.
4. Detailed ultrasound evaluation of the tunica vaginalis for all cases of chronic hydrocele and early MDT involvement is critical for ruling out MMTV and for favourable outcomes.
6References
1. Brevet, M. (2016). Comparative Genetics of Diffuse Malignant Mesothelioma Tumors of the Peritoneumand Pleura, With Focus on BAP1 Expression. 1(2), 91–97. https://doi.org/10.1515/PP-2016-0007
2. Drevinskaite, M., Smailyte, G., Kevlicius, L., Patasius, A., & Mickys, U. (2020). Malignant mesothelioma of the tunica vaginalis testis: a rare case and review of literature. BMC Cancer, 20(1). https://doi.org/10.1186/s12885-020-6648-3
3. Tiwana, M. S., & Leslie, S. W. (2020). Anatomy, Abdomen and Pelvis, Testicle. https://www.ncbi.nlm.nih.gov/books/NBK470201/
4. Yang, J., Chen, H., Yan, H., Zhang, Y., & Liu, J. (2024). Clinical and ultrasound features of fibrous pseudotumor of tunica vaginalis of the testis: eight cases and literature review. Frontiers in Oncology, 14. https://doi.org/10.3389/fonc.2024.1485723.
5. Bri, L. & Kern, I. (2020). Clinical significance of histologic subtyping of malignant pleural mesothelioma. AME Publishing Company. https://doi.org/10.21037/tlcr.2020.03.38
6. Liu, H., Dong, L., Xiang, L.-H., Xu, G., Wan, J., Fang, Y., Ding, S.-S., Jin, Y.-Q., Sun, L.-P., & Xu, H. (2022). Multiparametric ultrasound for the assessment of testicular lesions with negative tumoral markers. Asian Journal of Andrology, 25(1), 50–57. https://doi.org/10.4103/aja202235
7. Emile, S. H., Balata, M., Elfallal, A. H., & Abdelnaby, M. (2019). Malignant Mesothelioma of the Tunica Vaginalis: Incidental Diagnosis of a Rare Condition. Indian Journal of Surgery, 81(1), 80–82. https://doi.org/10.1007/S12262-018-1778-4
8. Mishra, K., Siddiquee, S., & Mislang, A. R. (2023). A rare presentation of malignant mesothelioma of the tunica vaginalis managed with immunotherapy and review of the literature. Clinical Case Reports, 11(6). https://doi.org/10.1002/ccr3.7610
9. Zhang, N., Fu, N., Peng, S., & Luo, X. (2017). Malignant mesothelioma of the tunica vaginalis testis: a case report and literature review.. Molecular and clinical oncology. https://doi.org/10.3892/mco.2017.1450
10. Sahu, R. K., Ruhi, S., Al-Goshae, H. A., Bhattacharjee, B., Bhattacharya, S., Khan, J., Goyal, M., Syed, A., Jangde, R. K., Ekasari, W., Nagdev, S., Widyowati, R., & Jeppu, A. K. (2023). Malignant mesothelioma tumours: molecular pathogenesis, diagnosis, and therapies accompanying clinical studies. Frontiers in Oncology, 13. https://doi.org/10.3389/fonc.2023.1204722
11. Nazar, T., Gopalakrishnabhaktan, A., et al. (2024). Testicular mesothelioma disguised as hydrocele: A case report. Journal of Medical Case Reports.
12. Chekol, S. S., & Sun, C.-C. (2012). Malignant mesothelioma of the tunica vaginalis testis: diagnostic studies and differential diagnosis. Archives of Pathology & Laboratory Medicine, 136(1), 113–117. https://doi.org/10.5858/ARPA.2010-0550-RS
13. Ladevaia, C., D’Agnano, V., Pagliaro, R., Nappi, F., Lucci, R., Massa, S., Bianco, A., & Perrotta, F. (2024). Diagnostic accuracy of ultrasound-guided percutaneous pleural needle biopsy for malignant pleural mesothelioma. Journal of Clinical Medicine, 13. https://doi.org/10.3390/jcm13092600
2. Drevinskaite, M., Smailyte, G., Kevlicius, L., Patasius, A., & Mickys, U. (2020). Malignant mesothelioma of the tunica vaginalis testis: a rare case and review of literature. BMC Cancer, 20(1). https://doi.org/10.1186/s12885-020-6648-3
3. Tiwana, M. S., & Leslie, S. W. (2020). Anatomy, Abdomen and Pelvis, Testicle. https://www.ncbi.nlm.nih.gov/books/NBK470201/
4. Yang, J., Chen, H., Yan, H., Zhang, Y., & Liu, J. (2024). Clinical and ultrasound features of fibrous pseudotumor of tunica vaginalis of the testis: eight cases and literature review. Frontiers in Oncology, 14. https://doi.org/10.3389/fonc.2024.1485723.
5. Bri, L. & Kern, I. (2020). Clinical significance of histologic subtyping of malignant pleural mesothelioma. AME Publishing Company. https://doi.org/10.21037/tlcr.2020.03.38
6. Liu, H., Dong, L., Xiang, L.-H., Xu, G., Wan, J., Fang, Y., Ding, S.-S., Jin, Y.-Q., Sun, L.-P., & Xu, H. (2022). Multiparametric ultrasound for the assessment of testicular lesions with negative tumoral markers. Asian Journal of Andrology, 25(1), 50–57. https://doi.org/10.4103/aja202235
7. Emile, S. H., Balata, M., Elfallal, A. H., & Abdelnaby, M. (2019). Malignant Mesothelioma of the Tunica Vaginalis: Incidental Diagnosis of a Rare Condition. Indian Journal of Surgery, 81(1), 80–82. https://doi.org/10.1007/S12262-018-1778-4
8. Mishra, K., Siddiquee, S., & Mislang, A. R. (2023). A rare presentation of malignant mesothelioma of the tunica vaginalis managed with immunotherapy and review of the literature. Clinical Case Reports, 11(6). https://doi.org/10.1002/ccr3.7610
9. Zhang, N., Fu, N., Peng, S., & Luo, X. (2017). Malignant mesothelioma of the tunica vaginalis testis: a case report and literature review.. Molecular and clinical oncology. https://doi.org/10.3892/mco.2017.1450
10. Sahu, R. K., Ruhi, S., Al-Goshae, H. A., Bhattacharjee, B., Bhattacharya, S., Khan, J., Goyal, M., Syed, A., Jangde, R. K., Ekasari, W., Nagdev, S., Widyowati, R., & Jeppu, A. K. (2023). Malignant mesothelioma tumours: molecular pathogenesis, diagnosis, and therapies accompanying clinical studies. Frontiers in Oncology, 13. https://doi.org/10.3389/fonc.2023.1204722
11. Nazar, T., Gopalakrishnabhaktan, A., et al. (2024). Testicular mesothelioma disguised as hydrocele: A case report. Journal of Medical Case Reports.
12. Chekol, S. S., & Sun, C.-C. (2012). Malignant mesothelioma of the tunica vaginalis testis: diagnostic studies and differential diagnosis. Archives of Pathology & Laboratory Medicine, 136(1), 113–117. https://doi.org/10.5858/ARPA.2010-0550-RS
13. Ladevaia, C., D’Agnano, V., Pagliaro, R., Nappi, F., Lucci, R., Massa, S., Bianco, A., & Perrotta, F. (2024). Diagnostic accuracy of ultrasound-guided percutaneous pleural needle biopsy for malignant pleural mesothelioma. Journal of Clinical Medicine, 13. https://doi.org/10.3390/jcm13092600