Student Image Challenge 107
June 13, 2024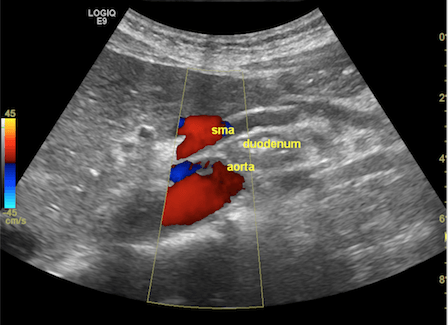
The eyes cannot see what the mind does not know. Ultrasound-based diagnosis of aorto-mesenteric clamp syndrome in the emergency department [February 2024]
July 3, 2024SUBMIT YOUR CASE
EFSUMB invites submission of interesting cases for the website section 'Case of the Month'. All CoM submissions are eligible for selection for free registration at the next Euroson congress. Two cases that receive the most 'likes' in a year will receive free registration for the next EUROSON congress and the third most liked liked case will receive a cash prize of 100 EUR.
A case of gastric duplication cyst diagnosed by double contrast enhanced ultrasound
Authors: Yi Dong[1], Ying Wang[1], Christoph F Dietrich[1],[2]
[1] Department of Ultrasound, Xinhua Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, China.
[2] Department Allgemeine Innere Medizin (DAIM), Kliniken Hirslanden Beau Site, Salem und Permancence, Bern, Switzerland.
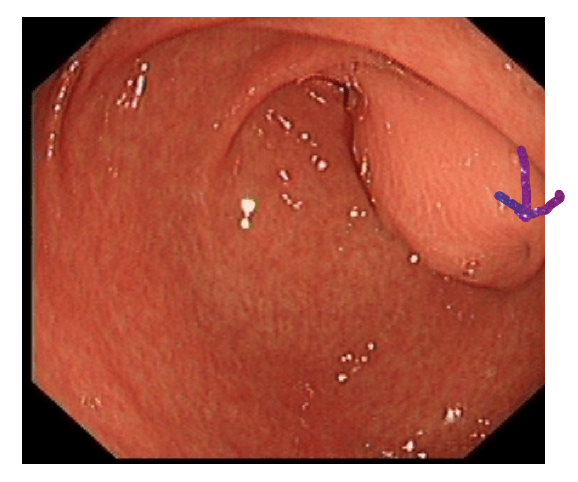
Figure 1 Gastroscopy shows subepithelial bulging of the gastric antrum. A small orifice (excavation) is suspected. The differential diagnosis is broad including cystic (e.g., duplication cyst as 20% of duplicate cysts have a connection to the GIT) and solid masses of different origin (e.g., ectopic pancreas or gastrointestinal stromal tumors [Gist]) (2, 3).
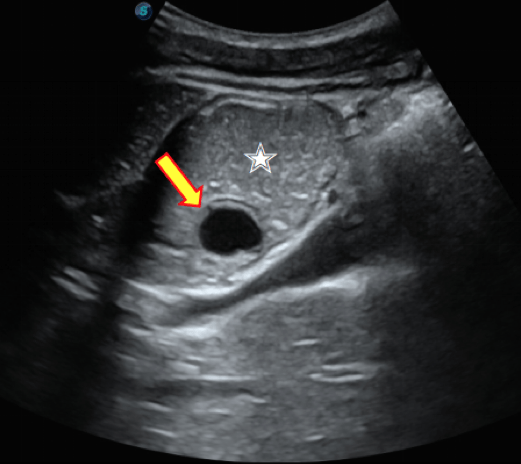
Figure 2. Gastric ultrasound shows a cystic mass (yellow arrow, 19 × 12 mm) with a layered wall (2.3 mm) in the gastric antrum cavity being covered towards the gastric lumen by the hyperechoic entry echo (layer 1), the hypoechoic mucosa/ muscularis mucosae (2) and the hyperechoic submucosa (3) that moved with the peristalsis of the stomach (white star).
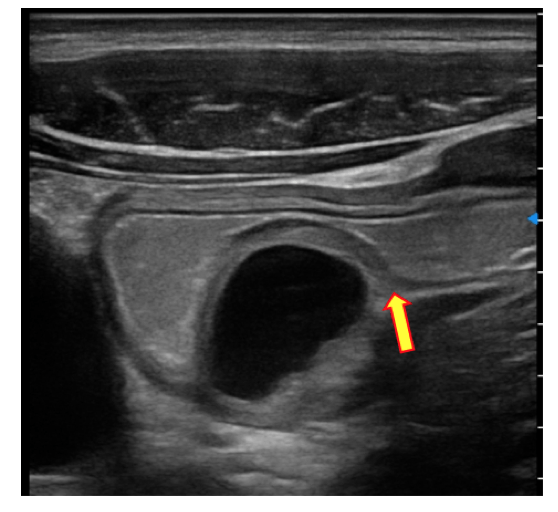
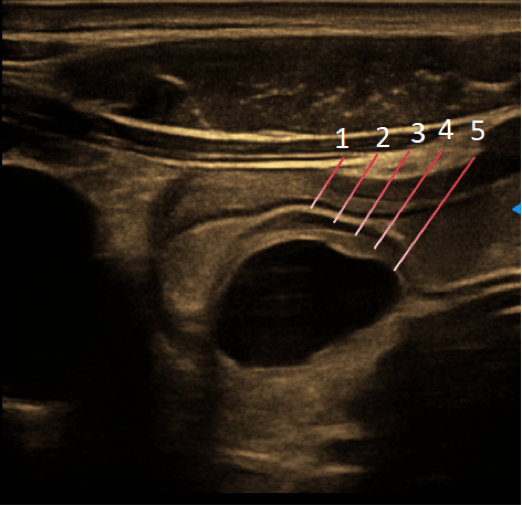
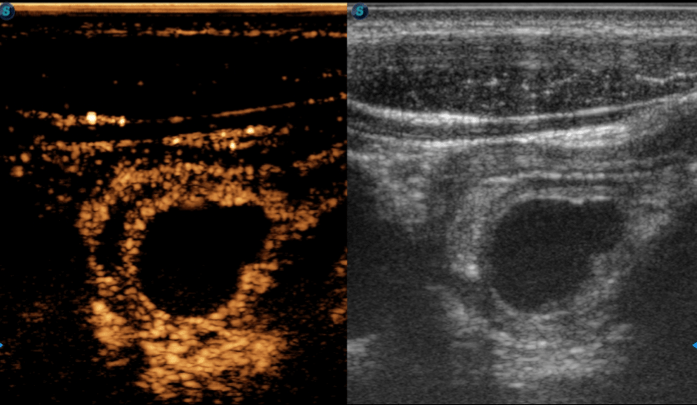
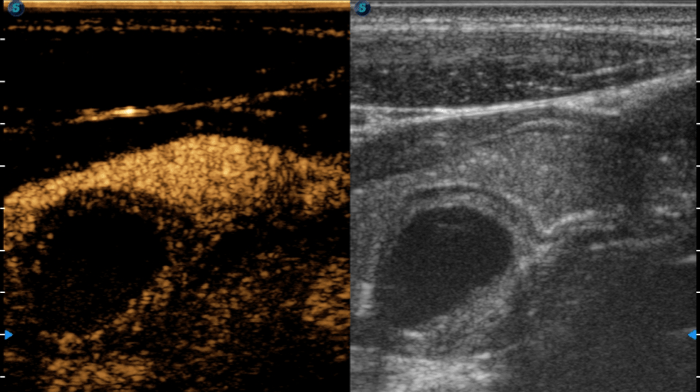
Figure 3a. Ultrasound scan performed by high-frequency linear transducer shows a double-wall sign of the cyst wall with hyperechoic submucosal layer and hypoechoic muscular layer. The interference of the submucosa and muscular layer of the cyst was connected with the respective layer of the gastric wall (yellow arrow) (a). A very thin hypoechoic band can be assumed in front of the inner face echo of the cyst, but this is hardly recognizable and can only be guessed at if one is familiar with the wall structure of duplication cysts or gastric foregut cystic developmental malformations. B mode ultrasound scan shows the five-layered structure of the cyst similar to the gastric wall (b). (1) Hyperechoic entrance reflex/ internal interface echo of the gastric wall. (2) Hypoechoic mucosa/ muscularis mucosae of the gastric wall. (3+4) Submucosa of the gastric wall. (5) Internal interface echo of the cyst and submucosa of the stomach wall. At the edge of the cyst, this hyperechoic echo merges into the submucosa of the stomach wall.
Figure 3b. Ultrasound scan performed by high-frequency linear transducer shows a double-wall sign of the cyst wall with hyperechoic submucosal layer and hypoechoic muscular layer. The interference of the submucosa and muscular layer of the cyst was connected with the respective layer of the gastric wall (yellow arrow) (a). A very thin hypoechoic band can be assumed in front of the inner face echo of the cyst, but this is hardly recognizable and can only be guessed at if one is familiar with the wall structure of duplication cysts or gastric foregut cystic developmental malformations. B mode ultrasound scan shows the five-layered structure of the cyst similar to the gastric wall (b). (1) Hyperechoic entrance reflex/ internal interface echo of the gastric wall. (2) Hypoechoic mucosa/ muscularis mucosae of the gastric wall. (3+4) Submucosa of the gastric wall. (5) Internal interface echo of the cyst and submucosa of the stomach wall. At the edge of the cyst, this hyperechoic echo merges into the submucosa of the stomach wall.
Transcutaneous ultrasound was performed with a S60 equipment (SonoScape, Shenzhen, China; C1-6A convex array probe, 12L-A linear array probe). Examination of the stomach reveals an anechoic cystic mass of about 19 × 12 mm in the gastric antrum cavity with regular margins and morphology. The wall thickness was about 2.3 mm. Real time ultrasound scanning revealed that the mass moved with the peristalsis of the stomach [Figure 2].
High-frequency ultrasound scan was performed using a linear transducer to observe the relationship of the mass to the gastric wall. The layer of the cyst was connected with the muscular layer of the gastric wall showing a double-wall sign with hyperechoic submucosal and hypoechoic muscular layer. The use of sepia tint map of B mode ultrasound might even show more clearly the defined layers of the cyst [Figure 3].
Then, double contrast enhanced ultrasound (CEUS) was performed. CEUS via intravenous injection of SonoVue 2.4 mL (Bracco SpA, Milan, Italy) as contrast agent. The degree of the cystic wall enhancement was similar to that of the gastric wall. The patient was instructed to take 100 ml of tap water with 5 drops of SonoVue contrast agent orally to observe if the cystic part of the mass was connected to the gastric cavity. It was found that the contrast agents did not enter the mass demonstrating that the mass was not connected to the gastric cavity [Figure 4].
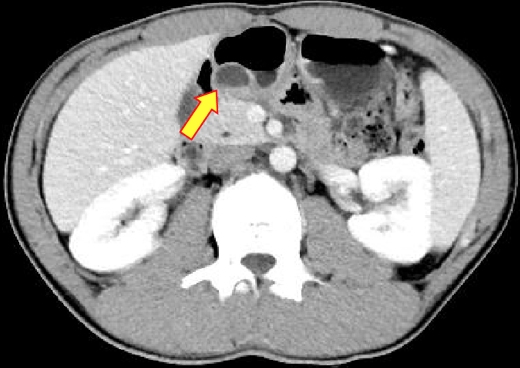
Contrast enhanced computed tomography (CECT) of the abdomen was performed, which revealed a non-enhanced cystic lesion of size 11 x 18 mm in curvature of the gastric antrum. The cyst showed no internal septations and calcifications. The enhancement degree of cystic wall was similar to that of the gastric wall [Figure 5].
Based on the clinical symptoms and the former two cross-sectional imaging methods, the clinical diagnosis was a gastric duplication cyst non-communicating with the gastrointestinal tract. Surgical resection is considered to be a curative treatment in symptomatic patients.
Double contrast enhanced ultrasound (CEUS) revealed a cystic mass in the antrum of the stomach. In this case, the initial clinical symptoms were non-specific, patient admitted for subepithelial bulge suggested by EGD. Although both CECT and CEUS suggest GDC, CEUS provides more imaging information for clinical including the layer of the cystic wall. Also, CEUS showed its relationship to the gastric wall and to the gastric lumen. Diagnostic and interventional endoscopic ultrasound is often used in suspected subepithelial lesions (7) but was not performed in this patient.
The essential features for GDC diagnosis include: 1) the cyst wall is continuous with the stomach; 2) the smooth muscle layer of the cyst is shared with the stomach; 3) the cyst is lined with gastrointestinal epithelium; 4) the cyst and the stomach share a common blood supply (8, 9).
Duplication cysts can be cystic or tubular and may be communicating or non-communicating with the gastrointestinal tract. The most common type (80 %) is the cystic and non-communicating form (10).
2. Jenssen C, Dietrich CF. Endoscopic ultrasound of gastrointestinal subepithelial lesions. Ultraschall Med. 2008;29:236-256.
3. Ignee A, Jenssen C, Hocke M, Dong Y, Wang WP, Cui XW, Woenckhaus M, et al. Contrast-enhanced (endoscopic) ultrasound and endoscopic ultrasound elastography in gastrointestinal stromal tumors. Endosc Ultrasound 2017;6:55-60.
4. Abdalkader M, Al Hassan S, Taha A, Nica I. Complicated Gastric Duplication Cyst in an Adult Patient: Uncommon presentation of an uncommon disease. Journal of Radiology Case Reports 2017;11:16-23.
5. Jayapal L, Kumar S, Baskaran A, Balachandar TG, Swain SK. Gastric Duplication Cyst: A Report of a Rare Case. Cureus 2023.
6. He H, Tang T, Wang X, Zhou L, Wang L. Comparing endoscopic ultrasonography and double contrast-enhanced ultrasonography in the preoperative diagnosis of gastric stromal tumor. Cancer Imaging 2023;23.
7. Dietrich CF, Braden B, Jenssen C. Interventional endoscopic ultrasound. Curr Opin Gastroenterol 2021;37:449-461.
8. Rowling JT. Some observations on gastric cysts. Br J Surg 1959;46:441-445.
9. Tang XB, Bai YZ, Wang WL. An intraluminal pyloric duplication cyst in an infant. Journal of Pediatric Surgery 2008;43:2305-2307.
10. Menon P, Rao KL, Saxena AK. Duplication cyst of the stomach presenting as hemoptysis. Eur J Pediatr Surg 2004;14:429-431.