CO-OPTED MEMBER – Marcin Czeczelewski
September 1, 2025
MEMBER – Madara Ratniece
October 1, 2025SUBMIT YOUR CASE
EFSUMB invites submission of interesting cases for the website section 'Case of the Month'. All CoM submissions are eligible for selection for free registration at the next Euroson congress. Two cases that receive the most 'likes' in a year will receive free registration for the next EUROSON congress and the third most liked liked case will receive a cash prize of 100 EUR.
Beyond the Gallbladder: Biliary cyst with infrequent biliary malformation identified by ultrasonography
Authors:
1. Maria Stefany Ascencio Leon, Second-year Radiodiagnostic Resident , Don Benito Villa Nueva de la Serena Hospital.
2. Isabel Quintana Rodríguez. Radiologist ,Don Benito Villanueva de la Serena Hospital.
1Clinical History
Two-year-old patient presenting with abdominal pain for one week, with worsening intensity in the last four days. Symptoms are associated with food-content emesis, occasional diarrhea without pathological products, and dark-colored urine.
Physical examination reveals mild conjunctival jaundice, no palpable organomegaly, and no signs of peritoneal irritation.
Lab data highlights:
• Amylase: 190 U/L
• CRP: 14 mg/L
• Total bilirubin: 1.21 mg/dL
• Conjugated bilirubin: 0.55 mg/dL
Physical examination reveals mild conjunctival jaundice, no palpable organomegaly, and no signs of peritoneal irritation.
Lab data highlights:
• Amylase: 190 U/L
• CRP: 14 mg/L
• Total bilirubin: 1.21 mg/dL
• Conjugated bilirubin: 0.55 mg/dL
2Imaging Findings
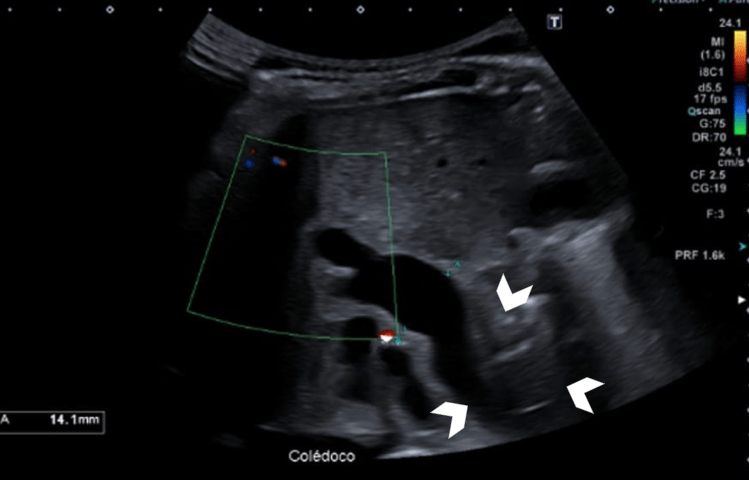
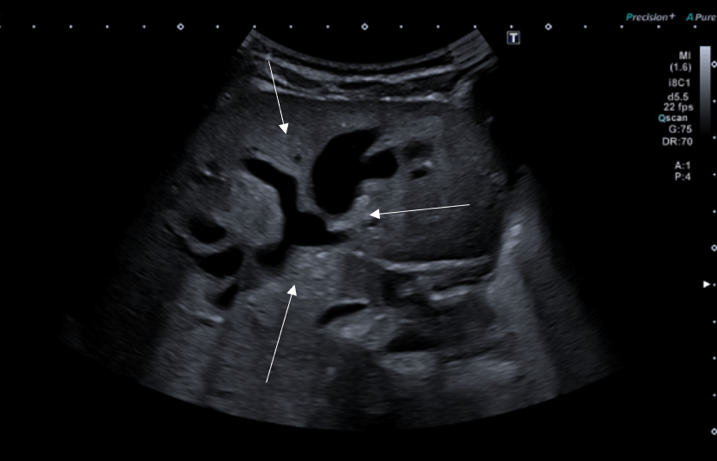
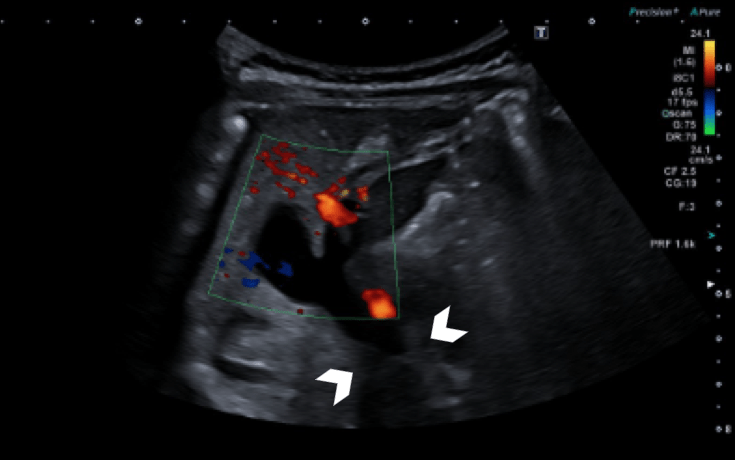
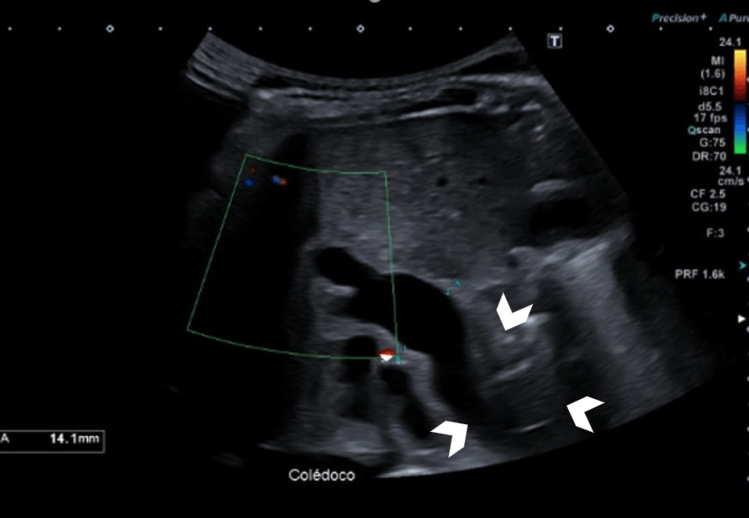
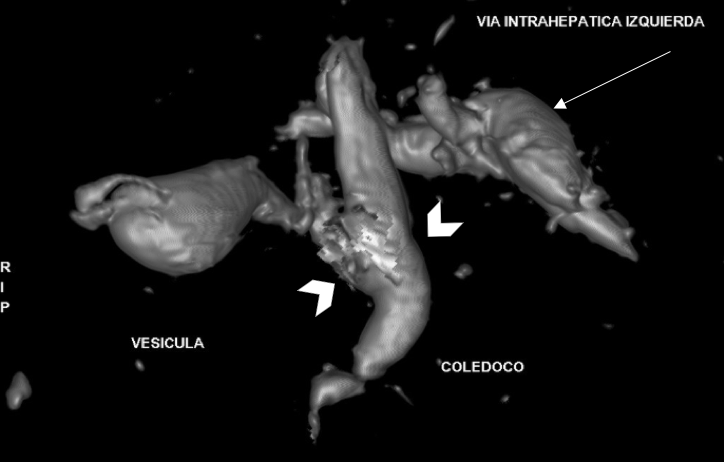
An ultrasound of the entire abdomen was performed using a Canon Aplio i800 ultrasound scanner with a 5 MHz convex probe and an abdominal protocol. The examination revealed fusiform dilatation of the intra- and extrahepatic bile ducts at the level of the choledochus, with saccular intrahepatic dilatation observed at the hepatic hilum and in the left hepatic lobe (Fig.1,2)
The choledochus measures up to 14 mm in diameter in its proximal third (Fig. 3), with the distal portion not visualized due to overlying duodenal gas. These findings are consistent with congenital dilatation of the common bile duct, suggestive of a Todani Type IVA choledochal cyst. It is therefore recommended to complement the study with MR cholangiography (MRCP).
MRCP confirms dilatation of both intrahepatic ducts, especially on the left (13 mm, saccular), and to a lesser extent on the right (7 mm). The hepatocoledochus measures 11 mm in diameter and shows a fusiform morphology (Fig. 4). The choledochus is visualized up to its intrahepatic segment and appears to join the pancreatic duct approximately 11 mm proximal to the duodenal papilla. These findings are compatible with a Todani Type IVA choledochal cyst and an anomalous pancreaticobiliary junction, Komi Type B.
No relevant family, personal, or surgical history.
The choledochus measures up to 14 mm in diameter in its proximal third (Fig. 3), with the distal portion not visualized due to overlying duodenal gas. These findings are consistent with congenital dilatation of the common bile duct, suggestive of a Todani Type IVA choledochal cyst. It is therefore recommended to complement the study with MR cholangiography (MRCP).
MRCP confirms dilatation of both intrahepatic ducts, especially on the left (13 mm, saccular), and to a lesser extent on the right (7 mm). The hepatocoledochus measures 11 mm in diameter and shows a fusiform morphology (Fig. 4). The choledochus is visualized up to its intrahepatic segment and appears to join the pancreatic duct approximately 11 mm proximal to the duodenal papilla. These findings are compatible with a Todani Type IVA choledochal cyst and an anomalous pancreaticobiliary junction, Komi Type B.
No relevant family, personal, or surgical history.
3Diagnosis
Todani Type IVA Choledochal Cyst
4Discussion
Choledochal cysts are rare congenital anomalies, occurring in approximately 1 per 150,000 live births. They are three times more common in females and more prevalent in the Asian population (1).
The most widely accepted theory of pathogenesis is Babbitt’s theory, present in 30–70% of cases, which postulates that an anomalous pancreaticobiliary junction leads to pancreatic reflux into the bile duct. This causes increased intraductal pressure, weakening of the bile duct wall, and subsequent cystic dilatation (1,2).
The Todani classification is currently the most accepted system for categorizing choledochal cysts, dividing them into five main types:
• Type I: Dilatation of the extrahepatic bile duct
o Ia: Cystic dilatation of the entire extrahepatic bile duct
o Ib: Segmental dilatation below the cystic duct junction
o Ic: Fusiform dilatation of the extrahepatic bile duct
• Type II: A true diverticulum of the common bile duct (~2% of cases)
• Type III: Choledochocoele (intraductal dilatation within the duodenal wall)
• Type IV: Dilatation of both intra- and extrahepatic bile ducts
o IVa: Involves the common bile duct, common hepatic duct, and intrahepatic ducts
o IVb: Involves multiple segments of the extrahepatic bile duct only
• Type V (Caroli’s disease): Segmental intrahepatic duct dilatation (3)
Type I is the most frequent (80% of cases), followed by type IVa (20%), as seen in our patient (1).
Most cases are diagnosed during childhood, with only 25% detected in adulthood. The classic triad of abdominal pain, palpable mass, and jaundice is described but occurs in only ~20% of cases (4).
CLINICAL PERSPECTIVE:
Laboratory findings are typically non-specific. Symptoms may include fever, vomiting, and abdominal pain (4). Ultrasonography is the most accessible and widely used diagnostic tool, with a sensitivity of 71–91%. It is also useful for postoperative monitoring (2).
However, MRCP or ERCP remains the gold standard, especially for surgical planning, as they allow for detailed anatomical delineation of the biliary and pancreatic ducts and identification of vascular or ductal anomalies (4).
A complete evaluation should include assessment for associated extra-biliary anomalies, as concomitant cardiac anomalies are reported in up to 31% of cases (2).
POTENTIAL COMPLICATIONS:
Complications include cholangitis, biliary strictures, lithiasis, and malignancy. The risk of neoplasia ranges from 10–30%, increasing with age (3).
The most common malignancy is cholangiocarcinoma (2), with the highest incidence in Todani Type I (68%) and Type IV (21%) cysts, the latter being the subtype present in this patient (3).
THERAPY PLANNING:
Surgical intervention included resection of the Type IVa choledochal cyst, intraoperative cholangiography, cholecystectomy, and Roux-en-Y hepaticojejunostomy.
PROGNOSIS AND OUTCOME:
Postoperatively, the patient remained under clinical observation in the intensive care unit and was discharged without complications.
The most widely accepted theory of pathogenesis is Babbitt’s theory, present in 30–70% of cases, which postulates that an anomalous pancreaticobiliary junction leads to pancreatic reflux into the bile duct. This causes increased intraductal pressure, weakening of the bile duct wall, and subsequent cystic dilatation (1,2).
The Todani classification is currently the most accepted system for categorizing choledochal cysts, dividing them into five main types:
• Type I: Dilatation of the extrahepatic bile duct
o Ia: Cystic dilatation of the entire extrahepatic bile duct
o Ib: Segmental dilatation below the cystic duct junction
o Ic: Fusiform dilatation of the extrahepatic bile duct
• Type II: A true diverticulum of the common bile duct (~2% of cases)
• Type III: Choledochocoele (intraductal dilatation within the duodenal wall)
• Type IV: Dilatation of both intra- and extrahepatic bile ducts
o IVa: Involves the common bile duct, common hepatic duct, and intrahepatic ducts
o IVb: Involves multiple segments of the extrahepatic bile duct only
• Type V (Caroli’s disease): Segmental intrahepatic duct dilatation (3)
Type I is the most frequent (80% of cases), followed by type IVa (20%), as seen in our patient (1).
Most cases are diagnosed during childhood, with only 25% detected in adulthood. The classic triad of abdominal pain, palpable mass, and jaundice is described but occurs in only ~20% of cases (4).
CLINICAL PERSPECTIVE:
Laboratory findings are typically non-specific. Symptoms may include fever, vomiting, and abdominal pain (4). Ultrasonography is the most accessible and widely used diagnostic tool, with a sensitivity of 71–91%. It is also useful for postoperative monitoring (2).
However, MRCP or ERCP remains the gold standard, especially for surgical planning, as they allow for detailed anatomical delineation of the biliary and pancreatic ducts and identification of vascular or ductal anomalies (4).
A complete evaluation should include assessment for associated extra-biliary anomalies, as concomitant cardiac anomalies are reported in up to 31% of cases (2).
POTENTIAL COMPLICATIONS:
Complications include cholangitis, biliary strictures, lithiasis, and malignancy. The risk of neoplasia ranges from 10–30%, increasing with age (3).
The most common malignancy is cholangiocarcinoma (2), with the highest incidence in Todani Type I (68%) and Type IV (21%) cysts, the latter being the subtype present in this patient (3).
THERAPY PLANNING:
Surgical intervention included resection of the Type IVa choledochal cyst, intraoperative cholangiography, cholecystectomy, and Roux-en-Y hepaticojejunostomy.
PROGNOSIS AND OUTCOME:
Postoperatively, the patient remained under clinical observation in the intensive care unit and was discharged without complications.
5Teaching Points
• Abdominal ultrasound remains the first-line imaging modality for evaluating the biliary tract.
• Familiarity with normal biliary anatomy is essential to accurately distinguish pathological changes in rare entities like choledochal cysts.
• Early detection and appropriate intervention can help prevent serious outcomes such as cholangiocarcinoma.
• Familiarity with normal biliary anatomy is essential to accurately distinguish pathological changes in rare entities like choledochal cysts.
• Early detection and appropriate intervention can help prevent serious outcomes such as cholangiocarcinoma.
6References
1. Carbajal-Castellanos Christian E., Ochoa Tebni, Sánchez-Sierra Luis Enrique, Alvarenga-Valladares Gerardo Enrique. Clinical-epidemiological characterization of choledochal cysts in the pediatric population treated at the Maternal and Child Hospital. Rev. Cir. 2023; 75(2): 91-97.
2. Mayorga-Garcés A, Mayorga-Garcés H-M-G. Update on the diagnosis and treatment of choledochal cysts. RAPD Online. 2018; 41(6): 280-284.
3. Rodríguez-Casanova M, Palma-Escobar O, Plácido-Méndez A, Waller-González L. Biliary cyst in a pediatric patient. Endosc Méx. 2016; 28(3): 123-127.
4. Climent Alcalá FJ, García Fernández de Villalta M, Escosa García L, Rodríguez Alonso A, Albajara Velasco LA. Care unit for children with complex chronic pathologies. A necessary model in our hospitals. An Pediatr (Barc). 2018; 88(1): 12-18.
5. Marquina Cintora S, Sánchez Suárez A, Herrero Álvarez M, Carabaño Aguado I, Aguirre Pascual E, Salcedo Lobato E, et al. Joubert syndrome. Rev Pediatr Aten Primaria. 2021; 23(90): 191-194.
2. Mayorga-Garcés A, Mayorga-Garcés H-M-G. Update on the diagnosis and treatment of choledochal cysts. RAPD Online. 2018; 41(6): 280-284.
3. Rodríguez-Casanova M, Palma-Escobar O, Plácido-Méndez A, Waller-González L. Biliary cyst in a pediatric patient. Endosc Méx. 2016; 28(3): 123-127.
4. Climent Alcalá FJ, García Fernández de Villalta M, Escosa García L, Rodríguez Alonso A, Albajara Velasco LA. Care unit for children with complex chronic pathologies. A necessary model in our hospitals. An Pediatr (Barc). 2018; 88(1): 12-18.
5. Marquina Cintora S, Sánchez Suárez A, Herrero Álvarez M, Carabaño Aguado I, Aguirre Pascual E, Salcedo Lobato E, et al. Joubert syndrome. Rev Pediatr Aten Primaria. 2021; 23(90): 191-194.