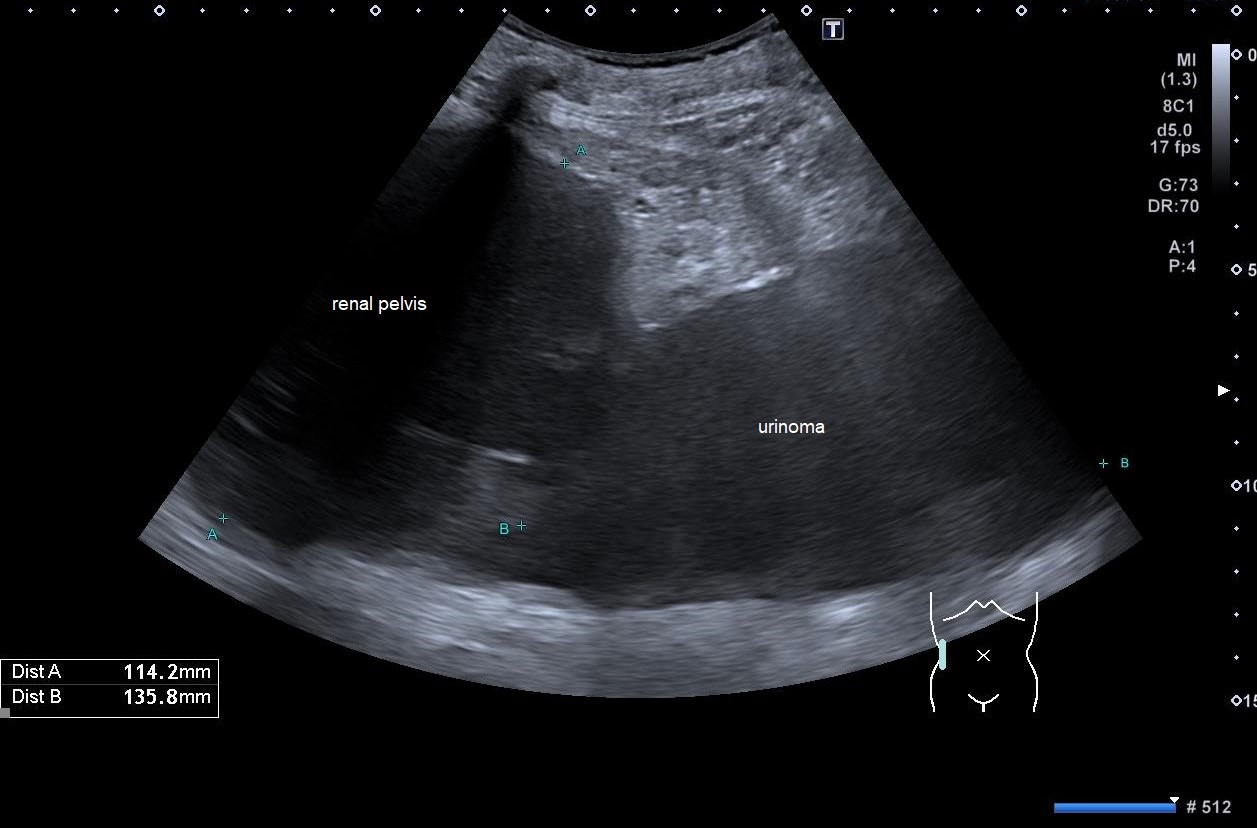
Spontaneous Rupture of the Renal Pelvis with Large Urinoma [May 2024]
July 22, 2024ECMUS TQA Survey
September 30, 2024SUBMIT YOUR CASE
EFSUMB invites submission of interesting cases for the website section 'Case of the Month'. All CoM submissions are eligible for selection for free registration at the next Euroson congress. Two cases that receive the most 'likes' in a year will receive free registration for the next EUROSON congress and the third most liked liked case will receive a cash prize of 100 EUR.
Primary or metastatic tumor? - A case report of mucinous adenocarcinoma of pancreas
Authors:Rui Cheng [1], Ying Wang [1], Li Wei [1], Jung Ernst Michael [2], Yi Dong [1]
[1] Department of Ultrasound, Xin Hua Hospital Affiliated to Shang Hai Jiaotong University School of Medicine, Shanghai, China
[2] Institute for Diagnostic Radiology and Interdisciplinary Ultrasound, University Hospital Regensburg, Regensburg, Germany
Figure 4a: The masses in the liver showed annular enhancement in the arterial phase of CEUS, with faster washout compared to the surrounding parenchyma. It appeared hypoechoic in the portal venous and delayed phases (a). The vascular structure and morphology of liver metastases were clearly displayed on SR CEUS (b).
Figure 4b: The masses in the liver showed annular enhancement in the arterial phase of CEUS, with faster washout compared to the surrounding parenchyma. It appeared hypoechoic in the portal venous and delayed phases (a). The vascular structure and morphology of liver metastases were clearly displayed on SR CEUS (b).
Pancreatic metastasis of lung adenocarcinoma is rare[1]. A retrospective study of 2872 patients with lung adenocarcinoma showed pancreatic metastases in only 17 patients (0.59%) [2]. Primary pulmonary mucinous adenocarcinoma is a special subtype of lung adenocarcinoma [3], accounting for about 0.24% of lung cancer [4]. Thus, this case is extremely unusual. We report a 47-year-old woman who was admitted to our hospital for the pancreatic and hepatic masses. Symptoms, such as abdominal distension and backache, were non-specific. Diagnostic imaging, especially CEUS, with intravenous microbubbles, plays a vital role in differentiating the masses.
CLINICAL PERSPECTIVE:
Based on the clinical symptoms and the former three cross-sectional imaging methods, the clinical diagnosis was primary pancreatic cancer together hepatic metastasis, with tumor cells originating from ductal epithelium. Histopathological results of masses from both pancreas and liver were mucinous adenocarcinomas. These findings were consistent with the ultrasound diagnosis —— pancreatic tumor originating from epithelial cells. However, immunohistochemistry showed that ALK (+), a specific manifestation of lung adenocarcinoma. Thus, we back to Positron Emission Tomography/Computed Tomography (PET/CT) reports, and found an abnormal FDG concentrations in the lung (Figure 6). Finally, after the discussion of multi-disciplinary team (MDT), pancreatic lesion was diagnosed as metastatic mucinous adenocarcinoma, originating from primary lung mucinous adenocarcinoma.
THERAPY PLANNING:
Surgical resection was excluded because of the multiple metastases. Since immunohistochemistry results showed ALK (+), the patient received targeted therapy, which has potential efficacy.
OUTCOME & PROGNOSIS:
Our final diagnosis was pancreatic metastasis of lung adenocarcinoma. Primary pulmonary mucinous adenocarcinoma is a special subtype of lung adenocarcinoma, with poor prognosis [3]. In this case, the patient presented with multi-organ metastases and progressed rapidly , therefore could not undergo surgery.
2. Niu FY, Zhou Q, Yang JJ, et al. Distribution and prognosis of uncommon metastases from non-small cell lung cancer. BMC Cancer, 2016, 16: 149.
3. Li W, Yang Y, Yang M, et al. Clinicopathologic Features and survival outcomes of primary lung mucinous adenocarcinoma based on different Rrdiologic Subtypes. Ann Surg Oncol, 2024, 31(1): 167-77.
4. Xue H, Zhou W, Zkang Z, et al. Femoral head metastases from primary mucinous lung adenocarcinoma with left hip pain: A case report and literature review. Front Surg, 2022, 9: 987627.










