- European Federation of Societies for Ultrasound in Medicine and Biology ~ Educating all for competence to practice ultrasound safely

(Ch:36) Ultrasound of the Scrotum
January 3, 2018
(Ch:35) Ultrasound of Peripheral Veins
January 15, 2018An Unexpected finding of an Early Pregnancy Scan
T Seaton, ME Roddie, AK Lim
Imperial College Healthcare Trust, Charing Cross Hospital Campus, London W6 8Rf, United Kingdom.
Imperial College Healthcare Trust, Charing Cross Hospital Campus, London W6 8Rf, United Kingdom.
1Clinical History
A 33 year old lady attended for an early pregnancy (8/40) ultrasound. She had a history of endometriosis and one previous failed IVF pregnancy. She was well with no pain or vaginal bleeding. Clinical examination was normal.
2Image Findings
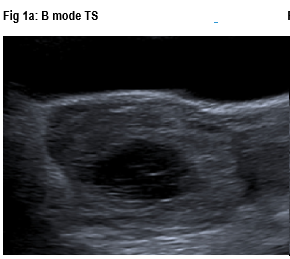
Trans-abdominal and trans-vaginal ultrasounds (Figure 1: a-c) demonstrated:
- An endometrial thickening of 19 mm with no intrauterine gestational sac.
- A right ovary containing a 26mm endometrioma.
- A left adnexal rounded mass measuring 7.3 x 5.8 x 7.3cm lying between the uterus and the left ovary. It had a cystic, irregular central portion and a markedly vascular periphery. The appearances were suggestive of a gestational sac and an ectopic pregnancy. However the appearances were somewhat unusual and the marked peripheral vascularity and grey-scale changes raised the possibility of a trophoblastic tumour.
MRI pelvis (T2 sagittal, T1 coronal, T2 coronal fat-sat, T2 transverse, T2 transverse-oblique, DWI and ADC sequences) study demonstrated:
- A large left adnexal mass measuring 6.6cm x 7.3cm x 7.1cm lying between the uterus and the left ovary, which demonstrated a heterogenous signal pattern with a haemorrhagic central. There are large serpiginous signal voids compatible with large angiogenic vessels typically seen with a gestational trophoblastic tumour.
3Diagnosis
The patients bhCG was also elevated beyond an 8 week pregnancy at just over 128,000 confirming the suspected diagnosis of a tubal molar pregnancy. She was initially treated with first line chemotherapy and had this molar pregnancy surgically removed once it had significantly reduced in size.
4Background
Gestational trophoblastic diseases (GTDs) constitute a spectrum of tumors characterized by abnormal proliferation of pregnancy-associated trophoblastic tissue with progressive malignant potential [1], usually involving the endometrial cavity.
The incidence of hydatidiform moles is1:1000–2000 pregnancies. Ectopic hydatidiform mole is extremely rare (1:1,000,000 pregnancies) [2]. Its malignant potential is similar to that of an intrauterine molar pregnancy.
5Clinical Perspective
Ectopic hydatidiform mole can present with abdominal pain with or without vaginal bleeding [3]. However, the patient may be asymptomatic.
Typically patients have an elevated serum bhCG levels (although a lower range than intra-uterine molar pregnancy because implantation in the fallopian tube precludes adequate vascularization) [4].
No single diagnostic method can confirm the presence of a mole with 100% accuracy. Diagnosis depends upon the correlation of clinical and pathological features.
Sonographically, a molar mass appears as a heterogenous, hypoechoic solid mass with cystic vascular spaces, increased vascularity and low resistance waveforms from the intra-uterine arteries [5].
MRI is not routinely required. However, it is useful in assessing the degree of myometrial invasion and locate disease outside the uterus as well as in recurrence or high risk patients [6,7]. A molar mass is heterogenous but predominantly low signal on T1WI and high on T2WI with avid contrast enhancement.
It is important to distinguish ectopic molar pregnancies from ectopic non-molar pregnancies as molar pregnancies can potentially be complicated by persistent trophoblastic disease and malignant transformation, which requires longer period of follow-up [6-9]. The high risk of extensive bleeding in molar pregnancy makes the option of surgical treatment less attractive.
6Therapy Outcomes
The dilemma in the management of these cases is whether to opt for neo-adjuvant chemotherapy or surgery as first line. The high risk of heavy bleeding makes surgery a less attractive option, however, this is offset by the risk of tubal rupture.
7Outcome
The gynaecology MDT team concluded that this patient should be managed conservatively as the risk of bleeding from surgery was too high. She was given a course of methotrexate and folic acid. Her bhCG reduced from to 57,189 following her first cycle. The mass was excised once the bhCG was normal.
8Prognosis
More than 80% of hydatidiform moles are benign. The prognosis of ectopic molar pregnancies is the same as for other forms of gestational trophoblastic disease [3, 8]. The outcome after treatment is usually excellent (nearly 100%).
9Teaching Points
- Tubal molar pregnancy is a rare event (1:1,000,000 pregnancies)
- Clinical diagnosis is difficult and the clinical features may be indistinguishable from non-molar ectopic pregnancy.
- Imaging aids diagnosis, therapy planning and is essential for follow up.
- Radiology cannot provide histological confirmation. However, correlation with bhCG indicates the diagnosis and post-surgical correlation is recommended.
10Figures
Figures 1a-c: B mode TS / B Mode LS showing mass and left ovary in callipers / Colour Doppler TS
Figure 2a-d: In view of the somewhat indeterminate findings, A MRI pelvic study was performed to further characterise this left adnexal mass (Figures 2: a-d)
Figure 3a-d: US images with power Doppler of a typical molar pregnancy within the endometrial cavity but with myometrial extension. These masses are commonly echogenic with small cystic spaces and the lesion and/or whole uterus is very vascular with significantly reduced pulsatility/resistive indices.
Figure 4 a-b: MRI images demonstrate the classic features of an intra-uterine molar pregnancy.
Figure 2a-d: In view of the somewhat indeterminate findings, A MRI pelvic study was performed to further characterise this left adnexal mass (Figures 2: a-d)
Figure 3a-d: US images with power Doppler of a typical molar pregnancy within the endometrial cavity but with myometrial extension. These masses are commonly echogenic with small cystic spaces and the lesion and/or whole uterus is very vascular with significantly reduced pulsatility/resistive indices.
Figure 4 a-b: MRI images demonstrate the classic features of an intra-uterine molar pregnancy.
11References
- Mickael JS, Edward SN. Gestational trophoblastic tumours. In: Shaw RW, editor. Gynaecology. 3rd ed. London (UK): Elsevier Science Limited; 2003. P. 653-64.
- Gillespie AM, Lidbury EA, Tidy JA, Honcock BW. The clinical presentation, treatment and outcome of patient diagnosed with possible ectopic molar gestation. Int J Gynaecol Cancer 2004; 14:366-9.
- Heidar Z, Sarfjoo FS, Zademodares S, Habibollahi M, Kheiri N. Molar ectopic pregnancy after tubectomy..Acta Med Iran. 2012; 50(8):565-7.
- Christopher PC. The female genital tract. In: Kumar V, Abdul K, Nelson F editors. Pathologic bases of disease. 7th ed. Philadelphia (US): Elsevier Inc; 2005, p.1059-119.
- Agarwal R, Harding V, Short D, Fisher RA, Sebire NJ, Harvey R, Patel D, Savage PM, Lim AK, Seckl MJ. Uterine artery pulsatility index: a predictor of methotrexate resistance in gestational trophoblastic neoplasia. Br J Cancer. 2012 Mar 13;106(6):1089-94
- Allen SD, Lim AK, Seckl MJ, Blunt DM, Mitchell AW. Radiology of gestational trophoblastic neoplasia. Clin Radiol. 2006 Apr;61(4):301-13.
- Lim AK, Patel D, Patel N, Hawtin K, Dayal L, Schmid P, Savage P, Seckl MJ. Pelvic imaging in gestational trophoblastic neoplasia. J Reprod Med. 2008 Aug;53(8):575-8.
- Yakasai IA, Adamu N, Galadanchi HS. Ruptured tubal molar pregnancy. Niger J Clin Pract. 2012 Oct-Dec; 15(4):491-3. Siozos A, Sriemevan A. A case of true tubal hydatidiform mole and literature review. BMJ Case Rep. 2010 Aug 9;2010


![An Unexpected finding of an Early Pregnancy Scan</br> [Jan 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_jan2018_fig1b.png)
![An Unexpected finding of an Early Pregnancy Scan</br> [Jan 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_jan2018_fig1c.png)
![An Unexpected finding of an Early Pregnancy Scan</br> [Jan 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_jan2018_fig2a.png)
![An Unexpected finding of an Early Pregnancy Scan</br> [Jan 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_jan2018_fig2b.png)
![An Unexpected finding of an Early Pregnancy Scan</br> [Jan 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_jan2018_fig2c.png)
![An Unexpected finding of an Early Pregnancy Scan</br> [Jan 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_jan2018_fig2d.png)
![An Unexpected finding of an Early Pregnancy Scan</br> [Jan 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_jan2018_fig3a.png)
![An Unexpected finding of an Early Pregnancy Scan</br> [Jan 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_jan2018_fig3b.png)
![An Unexpected finding of an Early Pregnancy Scan</br> [Jan 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_jan2018_fig3c.png)
![An Unexpected finding of an Early Pregnancy Scan</br> [Jan 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_jan2018_fig3d.png)
![An Unexpected finding of an Early Pregnancy Scan</br> [Jan 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_jan2018_fig4a.png)
![An Unexpected finding of an Early Pregnancy Scan</br> [Jan 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_jan2018_fig4b.png)
