Update on CEUS Non Liver Guidelines
December 8, 2017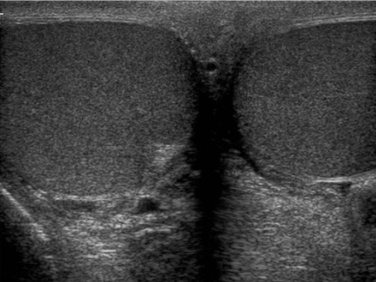
(Ch:36) Ultrasound of the Scrotum
January 3, 2018Fibromuscular dysplasia of the right renal artery
Correspondence: Prof. Dr. med. Christoph F. Dietrich, Medizinische Klinik 2, Caritas-Krankenhaus
Uhlandstr. 7, 97980 Bad Mergentheim, Tel:+49 7931 58 2201, Email: christoph.dietrich@ckbm.de
A 37 yo female patient suffered from chronic headaches. She was examined by a neurologist who diagnosed fibromyalgia. Her family practioner also diagnosed severe arterial hypertension (so-called “non dipper”) and excluded hyperaldosteronism, hyperthyroidism and sleep apnoea as secondary causes. Anti-hypertensive medication was initiated with amlodipine and ramipril. Although she is a smoker (> 20 py) there were no ultrasonic features of atherosclerosis. However, her estimated glomerular filtration rate was reduced (~68 ml/min/1,73m²). Auscultation also revealed a high frequent upper quadrant noise on the right side. The general practioners initial ultrasound showed a significant difference in the size and resistive index (RI) between the right and left kidney. For that reason, the patient was sent to our specialist hypertension center where the diagnosis of renal artery stenosis caused by fibromuscular dysplasia was confirmed.
The peak systolic velocity (PSV) in the renal artery is physiologically below < 1.5 m/s and typically around 1 m/s. In contrast, values > 1.8 m/s are indicative of significant stenosis. The normal RI values within the kidney are in the range of 0.55 - 0.65 and typically below 0.7. The normal values are increasing with age (up to 20 %) (1, 5, 6).
Figure 2: The retrocavally located right renal artery could be visualized posterior to the inferior vena cava (IVC) with a bruit in (a) and turbulent flow above 4 m/s in (b).
Figure 3: (a) The typical intrarenal interlobar poststenotic parvus-tardus spectrum is shown (RI 0.42 – 0.46) in comparison to the contralateral side (RI 0.62 - 65).
(b) The intrarenal interlobar spectrum one day after the successful percutaneous transluminal angioplasty showed normalisation of the resistive index (0.53, not shown).
Figure 4:(a) A normal and low-resistance Doppler spectrum was demonstrated one day after dilatation of the right renal artery (in between markers) without a bruit and turbulence.
(b) There was a PSV/EDV of 103/43 cm/s (RI = 0.59) (AO: aorta). .
Figure 5: 37 year old female with fibromuscular dysplasia of the right renal artery. Digital subtraction angiography (DSA) showing the classical "string of beads" appearance of the right renal artery with stenosis in the mid segment in (a). DSA after ballon angioplasty without relevant stenosis in (b).
2. Ignee A, Gebel M, Caspary WF, Dietrich CF. [Doppler imaging of hepatic vessels - review]. Z.Gastroenterol. 2002;40:21-32.
3.Jenssen C, Tuma J, Moller K, Cui XW, Kinkel H, Uebel S, Dietrich CF. [Ultrasound artifacts and their diagnostic significance in internal medicine and gastroenterology - part 2: color and spectral Doppler artifacts]. Z Gastroenterol 2016;54:569-578.
4. Dietrich CF, Siehr K: Arterielle Hypertonie. In: Dietrich CF, ed. Medizin im Vortrag. Balingen: Spitta Verlag, 2004; 1-19.
5. Brkljacic B, Castellani S, Deane C, Dietrich CF: Doppler ultrasound of renal vessels. In: Dietrich CF, ed. EFSUMB Course Book on Ultrasound. London, 2012; 716-736.
6. Brkljacic B, Castellani S, Deane C, Dietrich CF: Doppler ultrasound of the aorta, inferior vena cava and visceral arteries. In: Dietrich CF, ed. EFSUMB Course Book on Ultrasound. London, 2012; 693-714.



![Fibromuscular dysplasia of the right renal artery</br> [Dec 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_december2017-fig1b.jpg)
![Fibromuscular dysplasia of the right renal artery</br> [Dec 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_december2017-fig2a.jpg)
![Fibromuscular dysplasia of the right renal artery</br> [Dec 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_december2017-fig2b.jpg)
![Fibromuscular dysplasia of the right renal artery</br> [Dec 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_december2017-fig3a.jpg)
![Fibromuscular dysplasia of the right renal artery</br> [Dec 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_december2017-fig3b.jpg)
![Fibromuscular dysplasia of the right renal artery</br> [Dec 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_december2017-fig4a.jpg)
![Fibromuscular dysplasia of the right renal artery</br> [Dec 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_december2017-fig4b.jpg)
![Fibromuscular dysplasia of the right renal artery</br> [Dec 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_december2017-fig5a.jpg)
![Fibromuscular dysplasia of the right renal artery</br> [Dec 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_december2017-fig5b.jpg)
