- European Federation of Societies for Ultrasound in Medicine and Biology ~ Educating all for competence to practice ultrasound safely
CEUS for guidance and monitoring of interventions
March 17, 2019Elasto Small Parts (1)
March 25, 2019Large pedunculated lipoma of the esophagus: a case report
Elena-Codruța Constantinescu1,2, Adrian Săftoiu1,2
1. Research Center of Gastroenterology and Hepatology Craiova, University of Medicine and Pharmacy Craiova, Romania 2. GastroCenter Craiova, Romania
Elena Codruța Constantinescu
constantinescu.codruta@yahoo.com
1. Research Center of Gastroenterology and Hepatology Craiova, University of Medicine and Pharmacy Craiova, Romania 2. GastroCenter Craiova, Romania
Elena Codruța Constantinescu
constantinescu.codruta@yahoo.com
1Abstract
Esophageal lipomas are rare tumors, accounting for only 0.4% of all benign neoplasms of the gastrointestinal system. The majority of these tumors are located in the cervical part and just a few are located in the lower third of the esophagus (1). We present a case of a large pedunculated esophageal lipoma in a 46-year-old male who presented with dysphagia, regurgitation and a sensation of a lump in the throat. Upper gastrointestinal (GI) endoscopy revealed a pedunculated tumor mass within the esophageal lumen with its peduncle arising from the cervical esophagus. Endoscopic ultrasound (EUS) confirmed that the esophageal lumen was entirely occupied by a giant mobile lesion and computer tomography (CT) revealed the intraluminal pedunculated tumor mass.
2Case Report
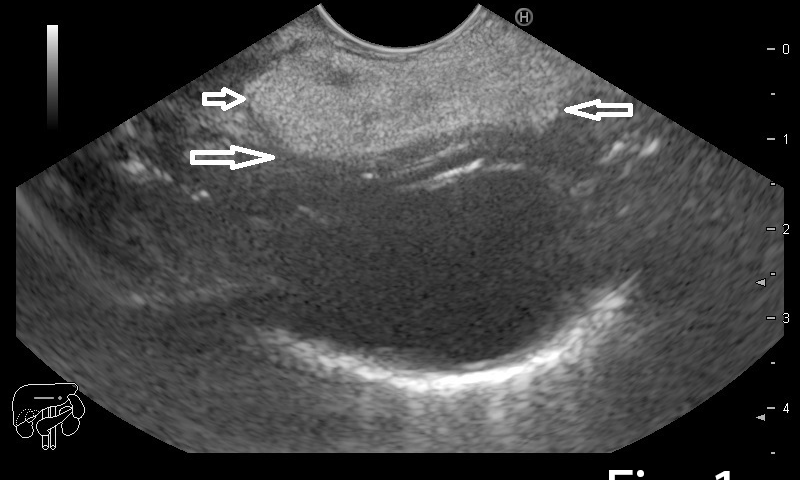
A 46-year old man presented to the gastrointestinal clinic complaining of dysphagia, regurgitation and a sensation of a lump in the throat, symptoms which had progressively worsened over the previous year. Upper GI endoscopy revealed a giant soft mass within the esophageal lumen, with a smooth surface covering, originating from the cervical esophagus, with a positive ”squeeze sign” (Video 1). EUS was performed and showed a giant mobile lesion occupying the esophageal lumen, with hyperechogenic structure, suggestive of a lipoma (Figure 1ab). Contrast-enhanced EUS did not depict any signals inside the subepithelial mass in the early arterial or late venous phases(Figure 1c). In order to define the surgical approach, a CT of the neck, thorax and abdomen was performed and it revealed the submucosal pedunculated tumor mass, confirming the diagnosis of lipoma (Figure 2).
3Discussion
Gastrointestinal lipomas can be found anywhere along the entire length of the gastrointestinal tract; the esophagus is the least common site and accounts for only 0.4% of all benign neoplasms of the digestive tract [1,2]. Esophageal lipomas arise close to the upper esophageal sphincter, are usually slowly-growing, are solitary pedunculated tumors and they occur in adults, predominantly men [1,3.4]. The tumors are usually discovered incidentally, are small in size and the symptoms are correlated to the size of the tumor: dysphagia to solids is the most common when they are large enough (4,5).
In case of symptomatic patients and suspicion of an endoluminal mass, a correct diagnosis can be made using upper GI endoscopy, EUS and CT scan, although magnetic resonance imaging(MRI) sometimes provides superior results (6,7).
During endoscopy, one key finding is to observe a smooth and intact mucosa of the esophageal lumen. In addition, a pathognomonic sign for lipomas is the ”squeeze” sign - changes in the contour and configuration of the lesion as a result of peristalsis (8).
Biopsy is not advocated for esophageal lipomas (1,9) and thus EUS is used to determine the layer of origin of the tumor. It can clearly identify benign lesions, such as lipomas as they appear hyperechogenic (10).
For our case, upper GI endoscopy and EUS as well as CE-EUS supported the diagnosis of lipoma: the endoluminal mass was covered by a smooth mucosa, with a positive ”squeeze” sign, whilst EUS identified a submucosal hyperechogenic tumor without any vascularity.
As treatment options, small lipomas can be resected endoscopically with a polypectomy loop even if the site of origin can make the procedure technically challenging. Lipomas greater than 5 cm and pedunculated lipomas require surgical excision as they are usually symptomatic and have the potential of causing severe complications (11,12). In our case, the patient was referred to surgery due to the size and origin of the tumor, with a high potential of hemorrhage and/or perforation.
In case of symptomatic patients and suspicion of an endoluminal mass, a correct diagnosis can be made using upper GI endoscopy, EUS and CT scan, although magnetic resonance imaging(MRI) sometimes provides superior results (6,7).
During endoscopy, one key finding is to observe a smooth and intact mucosa of the esophageal lumen. In addition, a pathognomonic sign for lipomas is the ”squeeze” sign - changes in the contour and configuration of the lesion as a result of peristalsis (8).
Biopsy is not advocated for esophageal lipomas (1,9) and thus EUS is used to determine the layer of origin of the tumor. It can clearly identify benign lesions, such as lipomas as they appear hyperechogenic (10).
For our case, upper GI endoscopy and EUS as well as CE-EUS supported the diagnosis of lipoma: the endoluminal mass was covered by a smooth mucosa, with a positive ”squeeze” sign, whilst EUS identified a submucosal hyperechogenic tumor without any vascularity.
As treatment options, small lipomas can be resected endoscopically with a polypectomy loop even if the site of origin can make the procedure technically challenging. Lipomas greater than 5 cm and pedunculated lipomas require surgical excision as they are usually symptomatic and have the potential of causing severe complications (11,12). In our case, the patient was referred to surgery due to the size and origin of the tumor, with a high potential of hemorrhage and/or perforation.
4References
1. Mayo CW, Pagutalunan PJG, Brown DJ. Lipoma of the alimentary tract. Surgery 1963;53:598-603.
2. Algin C, Hacioglu A, Aydin T, İhtiyar E. Esophagectomy in esophageal lipoma: report of a case. Turk J Gastroenterol 2006;17:110-112.
3. Taylor AJ, Stewart ET, Dodds WJ. Gastrointestinal lipomas: a radiologic and pathologic review. AJR Am J Roentgenol 1990;155(6):1205-10
4. Wang CY, Hsu HS, Wu YC, Huang MH, Hsu WH. Intramural lipoma of the esophagus. J Chin Med Assoc 2005;68:240-3.
5. Tsalis K, Antoniou N, Kalfadis S, Dimoulas A, Dagdilelis AKL, Lazaridis C. Laparoscopic enucleation of a giant submucosal esophageal lipoma. Case report and literature review. Am J Case Rep 2013;14:179-183.
6. Murata Y, Yoshida M, Akimto S, Ide H, Suzuki S, Hanyu F. Evaluation of endoscopic ultrasonography for the diagnosis of submucosal tumors of the esophagus. SurgEndosc 1988;2(2):51-8.
7. Kang JY, Chan-Wilde C, Wee A, Chew R, Ti TK. Role of computed tomography and endoscopy in the management of alimentary tract lipomas. Gut 1990;31(5:):550-3.
8. P. Katsinelos, G. Chatzimavroudis, C. Zavos, I. Pilpilidis, G. Lazarki, B. Papaziogas, et all. Cecal lipoma with pseudomalignant features: a case report and review of the literature. World J Gastroenterol., 13 (May 7(17)), 2007, pp. 2510-2513
9. Hurwitz MM, Redleaf PD, Williams HJ, Edwards JE. Lipomas of the gastrointestinal tract. An analysis of seventy-two tumors. Am J Roentgenol Radium TherNucl Med 1967;99(1):84-9.
10. Eckardt AJ, Jenssen C. Current endoscopic ultrasound-guided approach to incidental subepithelial lesions: optimal or optional? Ann Gastroenterol 2015;28(2):160-172.
11. Fumagalli U, Bona S, Battafarano F, Bonifacio C, Narne S, Peracchia A, Rosati R. Transoral surgical removal of a giant fibrolipoma of the esophagus: Case report.Gastroentérologie Clinique et Biologique2008;32(10):866-869.
12. Wang Q, Lin W, Zhou S. Large pedunculated lipoma of the esophagus: Report of a case and review of literature. JCRT 2015;11:(4), 1031-1031.
2. Algin C, Hacioglu A, Aydin T, İhtiyar E. Esophagectomy in esophageal lipoma: report of a case. Turk J Gastroenterol 2006;17:110-112.
3. Taylor AJ, Stewart ET, Dodds WJ. Gastrointestinal lipomas: a radiologic and pathologic review. AJR Am J Roentgenol 1990;155(6):1205-10
4. Wang CY, Hsu HS, Wu YC, Huang MH, Hsu WH. Intramural lipoma of the esophagus. J Chin Med Assoc 2005;68:240-3.
5. Tsalis K, Antoniou N, Kalfadis S, Dimoulas A, Dagdilelis AKL, Lazaridis C. Laparoscopic enucleation of a giant submucosal esophageal lipoma. Case report and literature review. Am J Case Rep 2013;14:179-183.
6. Murata Y, Yoshida M, Akimto S, Ide H, Suzuki S, Hanyu F. Evaluation of endoscopic ultrasonography for the diagnosis of submucosal tumors of the esophagus. SurgEndosc 1988;2(2):51-8.
7. Kang JY, Chan-Wilde C, Wee A, Chew R, Ti TK. Role of computed tomography and endoscopy in the management of alimentary tract lipomas. Gut 1990;31(5:):550-3.
8. P. Katsinelos, G. Chatzimavroudis, C. Zavos, I. Pilpilidis, G. Lazarki, B. Papaziogas, et all. Cecal lipoma with pseudomalignant features: a case report and review of the literature. World J Gastroenterol., 13 (May 7(17)), 2007, pp. 2510-2513
9. Hurwitz MM, Redleaf PD, Williams HJ, Edwards JE. Lipomas of the gastrointestinal tract. An analysis of seventy-two tumors. Am J Roentgenol Radium TherNucl Med 1967;99(1):84-9.
10. Eckardt AJ, Jenssen C. Current endoscopic ultrasound-guided approach to incidental subepithelial lesions: optimal or optional? Ann Gastroenterol 2015;28(2):160-172.
11. Fumagalli U, Bona S, Battafarano F, Bonifacio C, Narne S, Peracchia A, Rosati R. Transoral surgical removal of a giant fibrolipoma of the esophagus: Case report.Gastroentérologie Clinique et Biologique2008;32(10):866-869.
12. Wang Q, Lin W, Zhou S. Large pedunculated lipoma of the esophagus: Report of a case and review of literature. JCRT 2015;11:(4), 1031-1031.
5Figure and video legend
Figure 1a-b. EUS showing a hyperechogenic lesion with a smooth margin arising from the submucosal layer of the esophagus. 1c. Contrast-enhanced EUS indicated completely absent signals, for both the early arterial and late venous phases.
Figure 2. Contrast-enhanced CT showing the characteristic pedunculated lesion suggestive of lipoma (arrow).
Video 1. Videoendoscopy showing the pedunculated submucosal tumor with a large pedicle covered with normal mucosa originating in the cervical esophagus, with a positive "squeeze sign". The examination starts with withdrawal of the endoscope from the stomach, with visualisation of a soft mass in the left of the screen with normal overlying mucosa (00:50), with a long pedicle originated in the upper esophagus (1:30-2:00). The "squeeze sign" consists of shortening and thickening of the pedicle (3:10, 3:20)
Figure 2. Contrast-enhanced CT showing the characteristic pedunculated lesion suggestive of lipoma (arrow).
Video 1. Videoendoscopy showing the pedunculated submucosal tumor with a large pedicle covered with normal mucosa originating in the cervical esophagus, with a positive "squeeze sign". The examination starts with withdrawal of the endoscope from the stomach, with visualisation of a soft mass in the left of the screen with normal overlying mucosa (00:50), with a long pedicle originated in the upper esophagus (1:30-2:00). The "squeeze sign" consists of shortening and thickening of the pedicle (3:10, 3:20)


![Large pedunculated lipoma of the esophagus: a case report </br> [Mar 2019]](https://efsumb.org/wp-content/uploads/2020/11/COTM_march2019_Figure1a.png)
![Large pedunculated lipoma of the esophagus: a case report </br> [Mar 2019]](https://efsumb.org/wp-content/uploads/2020/11/COTM_march2019_Figure1b.png)
![Large pedunculated lipoma of the esophagus: a case report </br> [Mar 2019]](https://efsumb.org/wp-content/uploads/2020/11/COTM_march2019_Figure1c.png)
![Large pedunculated lipoma of the esophagus: a case report </br> [Mar 2019]](https://efsumb.org/wp-content/uploads/2020/11/COTM_march2019_Figure2.png)
