Breaking the Barrier: Ultrasound Diagnosis of Infantile Hypertrophic Pyloric Stenosis [March 2024]
July 9, 2024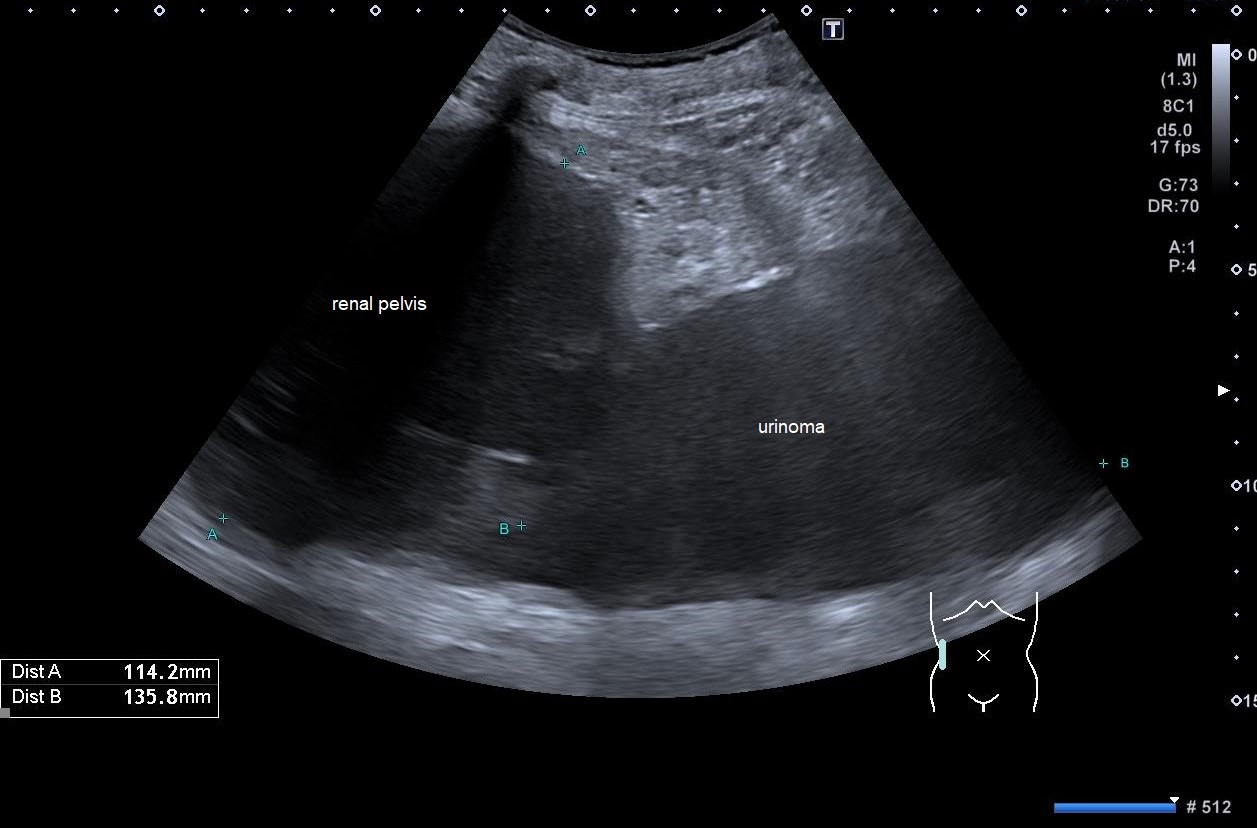
Spontaneous Rupture of the Renal Pelvis with Large Urinoma [May 2024]
July 22, 2024SUBMIT YOUR CASE
EFSUMB invites submission of interesting cases for the website section 'Case of the Month'. All CoM submissions are eligible for selection for free registration at the next Euroson congress. Two cases that receive the most 'likes' in a year will receive free registration for the next EUROSON congress and the third most liked liked case will receive a cash prize of 100 EUR.
Midgut malrotation and volvulus with bowel necrosis after HPS operation
Authors: Cvejic Sofija, Dasic Ivana, Radovic Tijana, Pavicevic Polina
Department of Radiology, University Children’s Hospital, Belgrade, Serbia
Movie 1. ’Whirlpool sign’ showing torsion of the small bowel mesentery.
1Clinical History
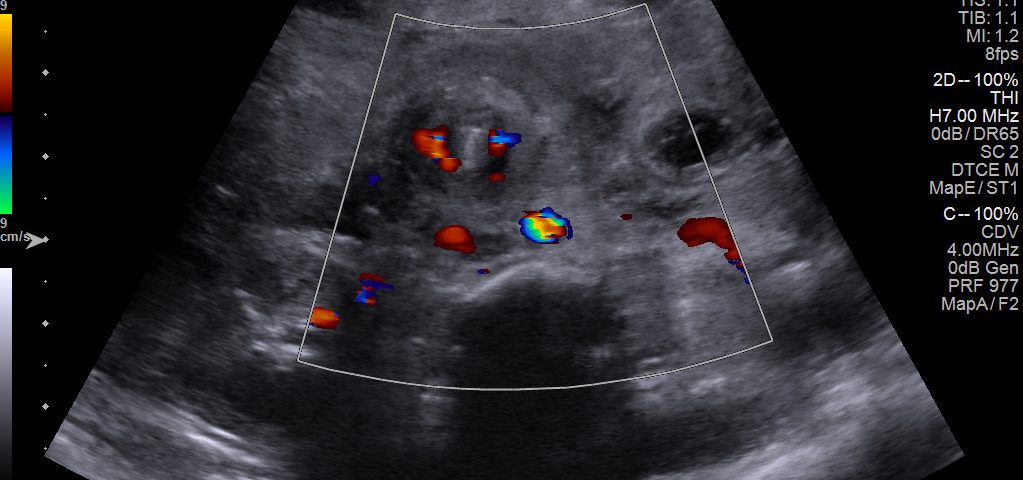
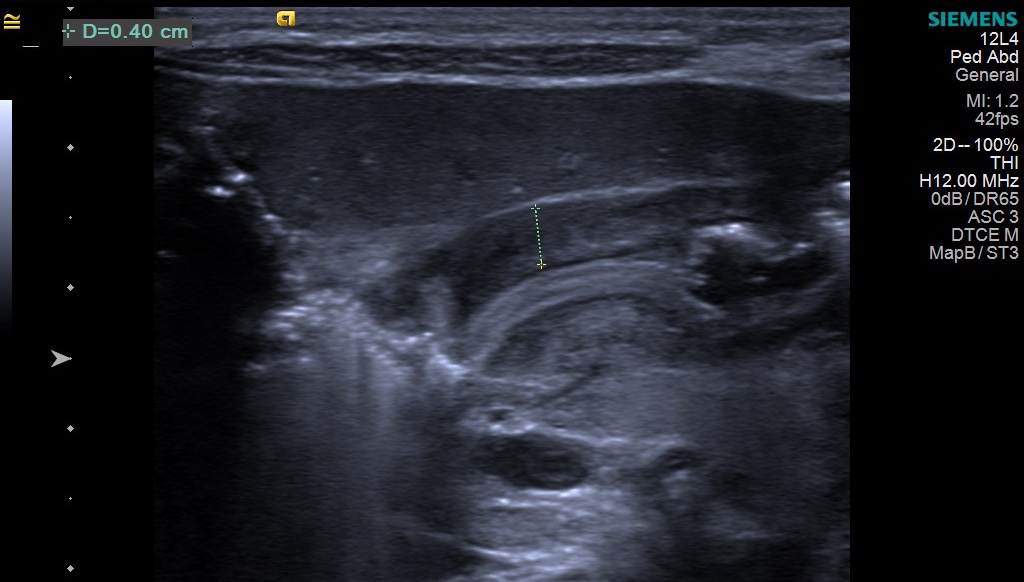
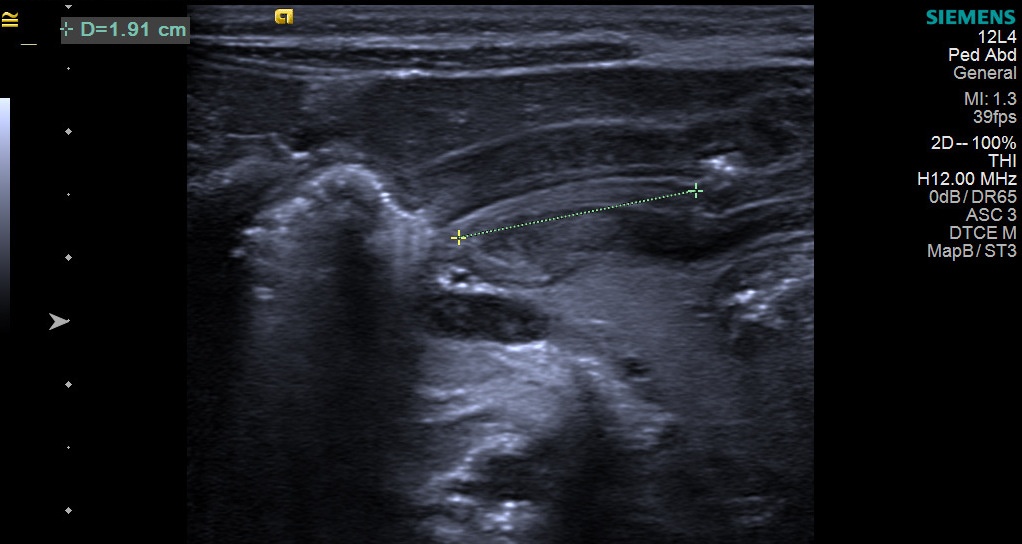
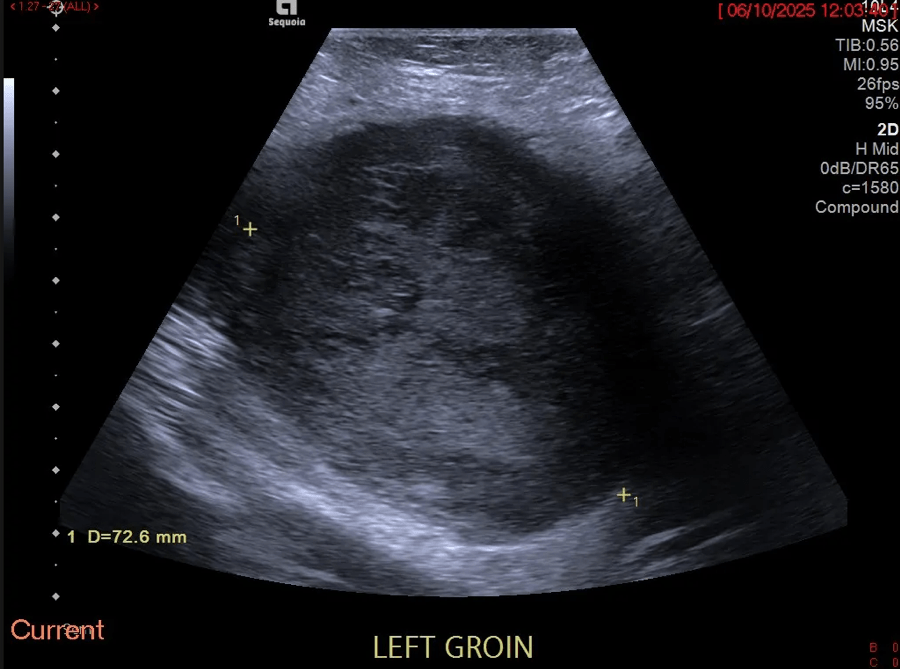
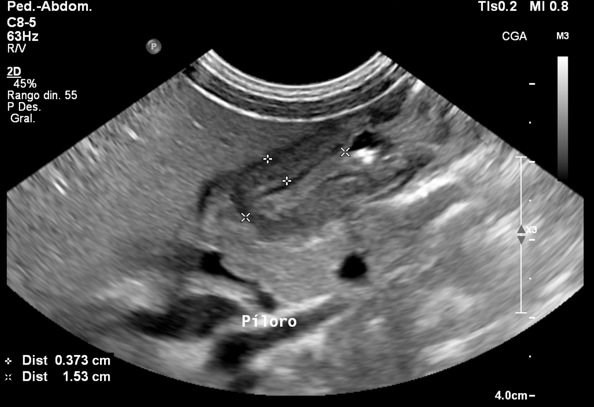
One month and four days old boy was reffered to our hospital due to projectile vomiting and poor weight gain after birth. Abdominal radiograph showed no signs of bowel obstruction and ultrasound (US) showed signs of hypertrophic pyloric stenosis (HPS)( Figures 1,2). The patient was surgically treated and was discharged after two days in good health. Two weeks later, he was admitted to intensive care unit (ICU) with low hemoglobin 62.0 g/L, elevated WBC count of 34.0 10^9/L and tachycardia.
2Image Findings
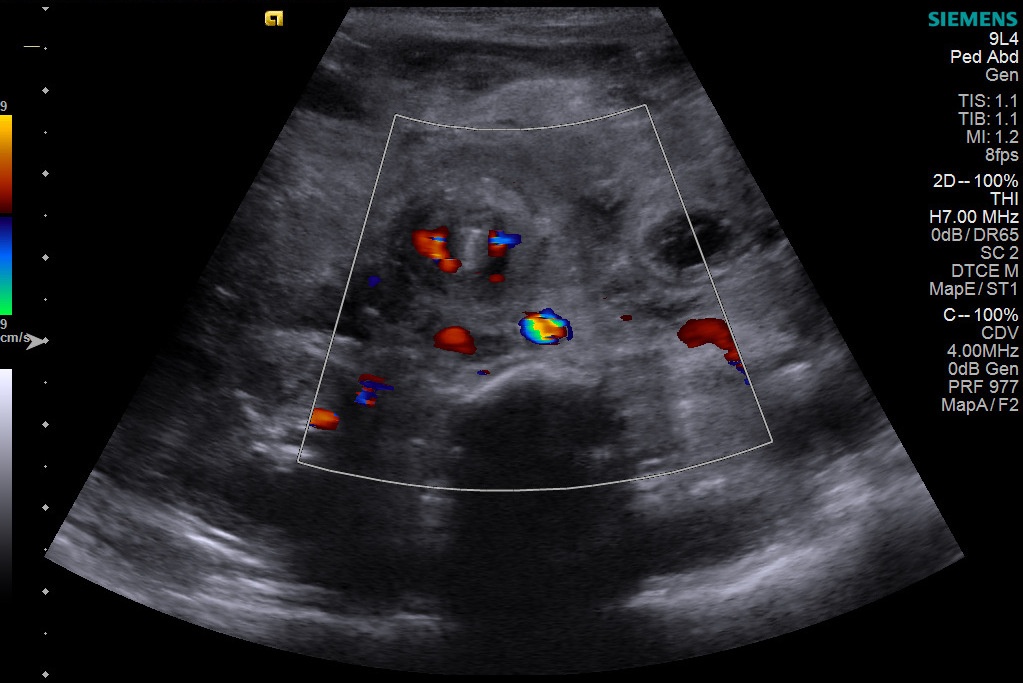
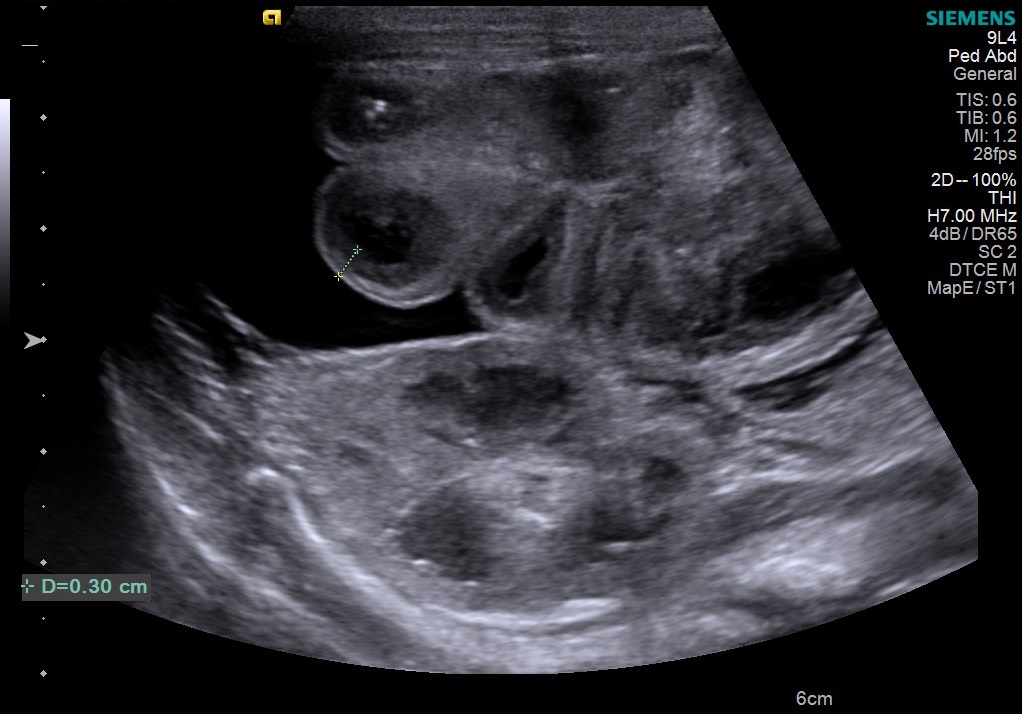
US in the ICU showed the ’whirlpool sign’ representing torsion of the vascular bundle of mesentry and inversion of superior mesenteric artery (SMA) and vein ( Figure 3, movie 1). All small bowel loops were edematous and showed tickened, layered appearance of the bowel wall measuring 3 mm, with no color doppler signal (Figure 4). There were signs of subhepatic, subsplenic and interintestinal free fluid with septations. In conclusion, US suggested the diagnosis of midgut volvulus with signs of necrotic changes of small bowel wall and septated intraperitoneal fluid.
3Diagnosis
Midgut volvulus with small bowel necrosis and presence of free fluid in the abdomen.
4Discussion
BACKGROUND:
Midgut malrotation is a congenital abnormal rotation of the midgut around the axis of the SMA [1]. Volvulus can be a life threatening condition that leads to bowel necrosis and short bowel syndrome if not diagnosed and treated on time [2]. Upper gastrointestinal (GI) series is the current reference standard for the diagnosis of midgut malrotation and volvulus, but it requires patient transport to the radiology department, administration of oral contrast agent, and use of ionizing radiation. The use of US as a first line diagnostic tool for this diagnosis is increasing because of the high sensitivity and specificity, wide availability, absence of radiation and fast interpretation [2,3].
CLINICAL PERSPECTIVE:
HPS and malrotation as separate entities are often encountered in pediatric hospitals, but their simultaneous presence is rarely found in the literature [4]. Since the patient presented with projectile vomiting and the diagnosis of HPS was confirmed on US, standard Ramstedt pyloromyotomy was performed and malrotation was not suspected. The second time the patient was admitted to our hospital, US examination was sufficient to confirm the diagnosis and the patient was not in the good condition to perform any other radiological examinations.
THERAPY PLANNING:
Given the fact that the patient was severely ill, immediate surgical treatment was needed. At surgery a 360 degree twist of the mesenteric bundle was found. The bowel wall was livid from duodenum to the transverse colon. After untwisting of the bowel and warming up, some of the bowel loops recovered so the Ladd procedure with appendectomy was performed. Malrotation should always be surgically treated even when it’s an incidental finding, because of the risk of midgut volvulus. Gross et al. [5] suggested laparoscopy as a minimally invasive method for performing the Ladd’s procedure in 1996. Aside from advantages such as shorter hospital stay, less pain and less postoperative complications, another benefit of the laparoscopic approach is that while performing the surgical procedure for pyloric stenosis, surgeon can also look for a potential simultaneous midgut malrotation [6].
OUTCOME:
After the surgery, patient was vomiting, had a distended and livid abdomen, so he was taken back to the operating room after two days. The small bowel loops were necrotic and only 3 cm of proximal jejunum and 3 cm of distal ileum could be saved. One month later a small bowel follow-through showed a stenosis at the level of the ileocecal valve and another operation was performed. After resecting the stenotic segment, there was only 12 cm of the bowel left from pylorus to colon.
PROGNOSIS:
The main concern in our patient is the short bowel syndrome which is defined as a reduction in the surface area available for absorption after extensive bowel resection. This can lead to malnutrition, steatorrhea, vitamin malabsorption, macrocytic anemia and other chronic complications. Intestinal rehabilitation in a specialized center can lead to enteral autonomy in majority of the patients. Intestinal transplantation is reserved for selected patients [6].
Midgut malrotation is a congenital abnormal rotation of the midgut around the axis of the SMA [1]. Volvulus can be a life threatening condition that leads to bowel necrosis and short bowel syndrome if not diagnosed and treated on time [2]. Upper gastrointestinal (GI) series is the current reference standard for the diagnosis of midgut malrotation and volvulus, but it requires patient transport to the radiology department, administration of oral contrast agent, and use of ionizing radiation. The use of US as a first line diagnostic tool for this diagnosis is increasing because of the high sensitivity and specificity, wide availability, absence of radiation and fast interpretation [2,3].
CLINICAL PERSPECTIVE:
HPS and malrotation as separate entities are often encountered in pediatric hospitals, but their simultaneous presence is rarely found in the literature [4]. Since the patient presented with projectile vomiting and the diagnosis of HPS was confirmed on US, standard Ramstedt pyloromyotomy was performed and malrotation was not suspected. The second time the patient was admitted to our hospital, US examination was sufficient to confirm the diagnosis and the patient was not in the good condition to perform any other radiological examinations.
THERAPY PLANNING:
Given the fact that the patient was severely ill, immediate surgical treatment was needed. At surgery a 360 degree twist of the mesenteric bundle was found. The bowel wall was livid from duodenum to the transverse colon. After untwisting of the bowel and warming up, some of the bowel loops recovered so the Ladd procedure with appendectomy was performed. Malrotation should always be surgically treated even when it’s an incidental finding, because of the risk of midgut volvulus. Gross et al. [5] suggested laparoscopy as a minimally invasive method for performing the Ladd’s procedure in 1996. Aside from advantages such as shorter hospital stay, less pain and less postoperative complications, another benefit of the laparoscopic approach is that while performing the surgical procedure for pyloric stenosis, surgeon can also look for a potential simultaneous midgut malrotation [6].
OUTCOME:
After the surgery, patient was vomiting, had a distended and livid abdomen, so he was taken back to the operating room after two days. The small bowel loops were necrotic and only 3 cm of proximal jejunum and 3 cm of distal ileum could be saved. One month later a small bowel follow-through showed a stenosis at the level of the ileocecal valve and another operation was performed. After resecting the stenotic segment, there was only 12 cm of the bowel left from pylorus to colon.
PROGNOSIS:
The main concern in our patient is the short bowel syndrome which is defined as a reduction in the surface area available for absorption after extensive bowel resection. This can lead to malnutrition, steatorrhea, vitamin malabsorption, macrocytic anemia and other chronic complications. Intestinal rehabilitation in a specialized center can lead to enteral autonomy in majority of the patients. Intestinal transplantation is reserved for selected patients [6].
5Teaching Points
Even though the US diagnosis of HPS was enough to expain patients symptoms of projectile vomiting, sometimes it can appear simultaneously with midgut malrotation which can lead to volvulus an bowel wall necrosis. Since the whirlpool sign on US is sufficient to confirm the diagnosis of midgut volvulus, it highlights the importance of US in making the proper diagnosis in a child presenting with these symptoms [7].
6References
1. Chaffin L, Snyder WH. Malrotation of the intestine. Surg Clin North Am 1956; 1479–1494.
2. Nguyen HN, Navarro OM, Bloom, DA, Feinstein KA, Guillerman RP, Munden et al. Ultrasound for midgut malrotation and midgut volvulus: AJR expert panel narrative review. AJR. 2022; 218(6):931–939.
3. Binu V, Nicholson C, Cundy T, et al. Ultrasound imaging as the first line of investigation to diagnose intestinal malrotation in children: Safety and efficacy. J Pediatr Surg 2021;56(12), 2224–2228.
4. Abo Elyazeed AM, Shalaby MM, Awad, et al. Idiopathic hypertrophic pyloric stenosis with complete Ladd's band: A rare association. European J Pediatr Surg Rep 2019; 7(1), e66–e68.
5. Gross E, Chen MK, Lobe TE. Laparoscopic evaluation and treatment of intestinal malrotation in infants. Surg Endosc 1996; 10(9), 936–937.
6. Bhalla VK, Harper JG, Hatley RM, Howell CG, Pipkin WL. Laparoscopic treatment of simultaneously occurring pyloric stenosis and malrotation. J Laparoendosc Adv Surg Tech A. 2008;18(4), 641–643.
7. Hong CR, Han SM, Staffa SJ, Carey AN, Modi BP, Jaksic T. Long-term outcomes of ultrashort bowel syndrome due to malrotation with midgut volvulus managed at an interdisciplinary pediatric intestinal rehabilitation center. J Pediatr Surg 2019; 54(5), 964–967.
2. Nguyen HN, Navarro OM, Bloom, DA, Feinstein KA, Guillerman RP, Munden et al. Ultrasound for midgut malrotation and midgut volvulus: AJR expert panel narrative review. AJR. 2022; 218(6):931–939.
3. Binu V, Nicholson C, Cundy T, et al. Ultrasound imaging as the first line of investigation to diagnose intestinal malrotation in children: Safety and efficacy. J Pediatr Surg 2021;56(12), 2224–2228.
4. Abo Elyazeed AM, Shalaby MM, Awad, et al. Idiopathic hypertrophic pyloric stenosis with complete Ladd's band: A rare association. European J Pediatr Surg Rep 2019; 7(1), e66–e68.
5. Gross E, Chen MK, Lobe TE. Laparoscopic evaluation and treatment of intestinal malrotation in infants. Surg Endosc 1996; 10(9), 936–937.
6. Bhalla VK, Harper JG, Hatley RM, Howell CG, Pipkin WL. Laparoscopic treatment of simultaneously occurring pyloric stenosis and malrotation. J Laparoendosc Adv Surg Tech A. 2008;18(4), 641–643.
7. Hong CR, Han SM, Staffa SJ, Carey AN, Modi BP, Jaksic T. Long-term outcomes of ultrashort bowel syndrome due to malrotation with midgut volvulus managed at an interdisciplinary pediatric intestinal rehabilitation center. J Pediatr Surg 2019; 54(5), 964–967.