Student Image Challenge 83
February 16, 2021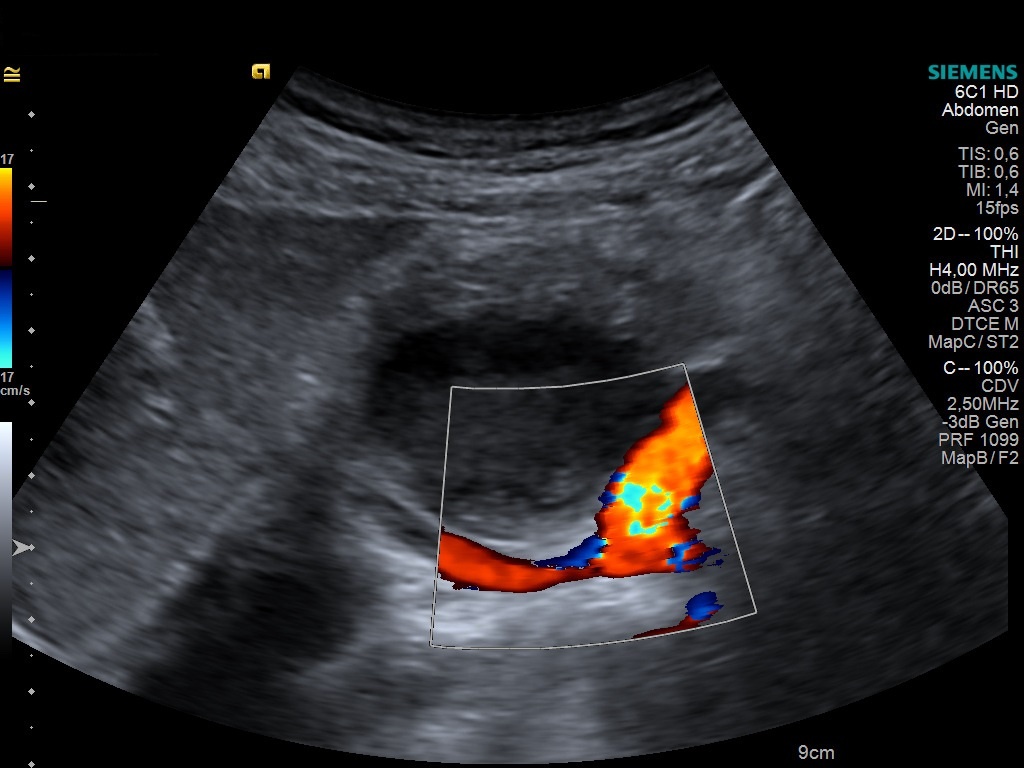
Student Image Challenge 84
March 5, 2021Nut Cracker
AUTHORS
Craig Ferguson (Radiology SpR),
Chris Harvey (Consultant Radiologist)
Dept Of Imaging, Imperial College NHS Healthcare Trust, London, UK
Craig Ferguson (Radiology SpR),
Chris Harvey (Consultant Radiologist)
Dept Of Imaging, Imperial College NHS Healthcare Trust, London, UK
1Clinical history
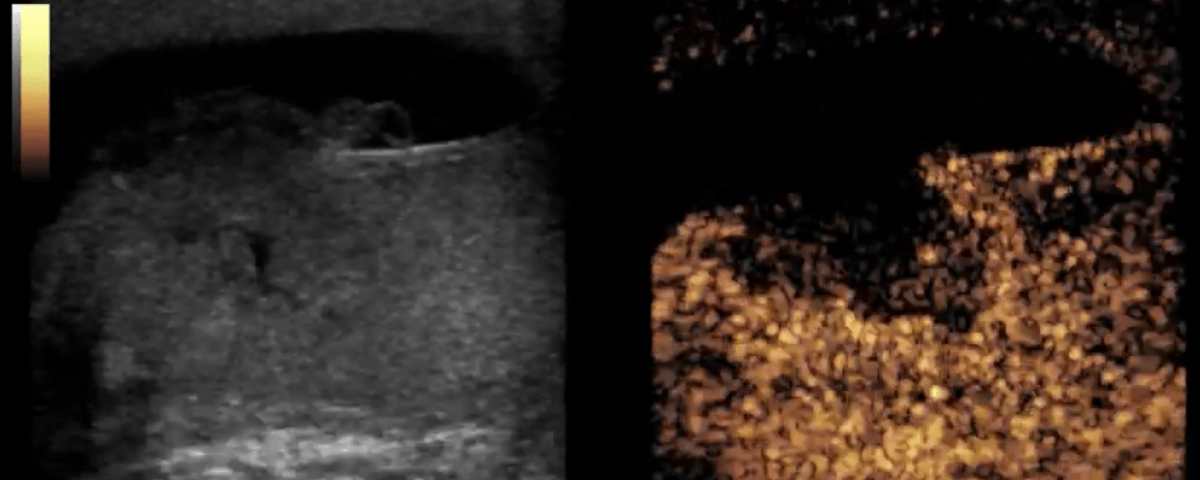
A 24-year old man who was kicked in the scrotum during martial arts training pre-sented with right testicular swelling and pain. A testicular ultrasound (Fig 1) demonstrated heterogeneous change in the midpole of the testicle with irregularity of the capsule and a haemoscrotum. It was difficult to accurately assess the viability of the testicle on Doppler. An orchidectomy was contemplated. A contrast-enhanced ultrasound (CEUS) with Sonovue (Bracco, Italy) was performed to re-solve the dilemma. CEUS (Fig 2) demonstrated a capsular breach and fractured testicle with some extrusion of soft tissue. CEUS showed that there was only a small area of non-viable tissue but preserved normal perfusion of the majority of the right testicle.
The patient underwent successful surgical repair salvaging the right testicle.
This case highlights the utility of CEUS in non-invasively assessing the nature and extent of testicular injury in trauma.
2Diagnosis
Blunt scrotal trauma resulting in testicular fracture
3Discussion
Most cases of scrotal trauma are self limiting but more severe cases can require hospital admission and surgical management. The majority of cases occur in the first three decades of life and severe trauma can require necessitate orchidectomy [1, 2]. Orchidectomy can lead to significant morbidity issues, such as sub fertility and body dysmorphia [3]. Clinical assessment may be limited due to swelling and pain and therefore imaging is crucial in the assessment of testicular viability to guide surgical management.
Ultrasound assessment is the gold standard in assessment of acute testicular trau-ma [4]. High frequency B-mode ultrasound can demonstrate scrotal haematoma, breach of the tunica albuginea and regions of parenchymal hypoechogenicity in testicular fracture. Unfortunately, B mode and colour Doppler ultrasound cannot accurately characterise testicular perfusion and the viability of the testicle [5].
Contrast enhanced testicular ultrasound (CEUS) has been found to improve the di-agnostic accuracy in the context of scrotal trauma. CEUS is able to more accurately characterise testicular perfusion which can guide management [6-8].
Ultrasound assessment is the gold standard in assessment of acute testicular trau-ma [4]. High frequency B-mode ultrasound can demonstrate scrotal haematoma, breach of the tunica albuginea and regions of parenchymal hypoechogenicity in testicular fracture. Unfortunately, B mode and colour Doppler ultrasound cannot accurately characterise testicular perfusion and the viability of the testicle [5].
Contrast enhanced testicular ultrasound (CEUS) has been found to improve the di-agnostic accuracy in the context of scrotal trauma. CEUS is able to more accurately characterise testicular perfusion which can guide management [6-8].
4Clinical Implication
This case demonstrates the benefit of contrast enhanced ultrasound in the assess-ment of blunt scrotal trauma. The ability to accurately document preserved perfu-sion of the majority of the testicle enabled the managing team to pursue testicular salvaging management and avoid an unnecessary orchidectomy.
5Learning Point
Severe scrotal trauma can require surgical management and orchidectomy.
B mode and colour doppler US is the current gold standard in assessing scrotal in-juries.
The addition of CEUS in the context of acute testicular trauma improves the opera-tors ability to quantify the extent of testicular perfusion and establish the viability of the testicle. This improved diagnostic capability can support testicular salvaging management.
B mode and colour doppler US is the current gold standard in assessing scrotal in-juries.
The addition of CEUS in the context of acute testicular trauma improves the opera-tors ability to quantify the extent of testicular perfusion and establish the viability of the testicle. This improved diagnostic capability can support testicular salvaging management.
6References
[1] Yusuf GT, Sidhu PS A review of ultrasound imaging in scrotal emergencies. J Ultrasound (2013) 16:171–178
[2] Missiroli C, Mansouri, M., Singh, A. Imaging of acute conditions of male repro-ductive organs. In: Singh A (ed) Emergency Radiology: Imaging of Acute Patholo-gies. 2nd ed edn. Springer, Switzerland, (2017) pp 116-132.
[3] Lee SH, Lee DG, Choi SK, Choi T, Yoo KH Trends in testicular injury in Korea, 1986-2015. J Korean Med Sci (2017) 32:1669–1673
[4] Adlan T, Freeman SJ (2014) Can ultrasound help to manage patients with scro-tal trauma? Ultrasound 22:205–212
[5] Yusuf G, Konstantatou E, Sellars ME, Huang DY, Sidhu PS Multiparametric so-nography of testicular hematomas: features on grayscale, color Doppler, and con-trast-enhanced sonography and strain elastography. J Ultrasound Med (2015) 34:1319–1328
[6] Sidhu P, Piscaglia F, Cantisani V et al. The EFSUMB Guidelines and Recom-mendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications. Ultraschall in Med 2018; 39: 1–42
[7] Hedayati V, Sellars ME, Sharma DM, Sidhu PS. Contrast-enhanced ultrasound in testicular trauma: role in directing exploration, debridement and organ salvage. Br J Radiol (2012); 85:e65–e68 [8] Valentino M, Bertolotto M, Derchi L et al Role of contrast enhanced ultrasound in acute scrotal diseases. Eur Radiol (2011) 21:1831–1840
[2] Missiroli C, Mansouri, M., Singh, A. Imaging of acute conditions of male repro-ductive organs. In: Singh A (ed) Emergency Radiology: Imaging of Acute Patholo-gies. 2nd ed edn. Springer, Switzerland, (2017) pp 116-132.
[3] Lee SH, Lee DG, Choi SK, Choi T, Yoo KH Trends in testicular injury in Korea, 1986-2015. J Korean Med Sci (2017) 32:1669–1673
[4] Adlan T, Freeman SJ (2014) Can ultrasound help to manage patients with scro-tal trauma? Ultrasound 22:205–212
[5] Yusuf G, Konstantatou E, Sellars ME, Huang DY, Sidhu PS Multiparametric so-nography of testicular hematomas: features on grayscale, color Doppler, and con-trast-enhanced sonography and strain elastography. J Ultrasound Med (2015) 34:1319–1328
[6] Sidhu P, Piscaglia F, Cantisani V et al. The EFSUMB Guidelines and Recom-mendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications. Ultraschall in Med 2018; 39: 1–42
[7] Hedayati V, Sellars ME, Sharma DM, Sidhu PS. Contrast-enhanced ultrasound in testicular trauma: role in directing exploration, debridement and organ salvage. Br J Radiol (2012); 85:e65–e68 [8] Valentino M, Bertolotto M, Derchi L et al Role of contrast enhanced ultrasound in acute scrotal diseases. Eur Radiol (2011) 21:1831–1840