Hot Topics in Interventional Ultrasound
March 19, 2021
Student Image Challenge 86
March 30, 2021Key Words: Renal, Kidneys, Ultrasound, MRI, Abscess
Renal Abscess progression a case study
AUTHORS
Mr Stephen Moore
Sonographer; Greater Glasgow and Clyde NHS Trust, The Royal infirmary
Ultrasound Images provided by:
Mrs Lynne Cassidy
Sonographer; Greater Glasgow and Clyde NHS Trust, The Royal infirmary, Mrs Helen Baylis
Sonographer; Greater Glasgow and Clyde NHS Trust, The Royal infirmary
Corresponding Author: Stephen Moore s.moore11nhs@gmail.com
Mr Stephen Moore
Sonographer; Greater Glasgow and Clyde NHS Trust, The Royal infirmary
Ultrasound Images provided by:
Mrs Lynne Cassidy
Sonographer; Greater Glasgow and Clyde NHS Trust, The Royal infirmary, Mrs Helen Baylis
Sonographer; Greater Glasgow and Clyde NHS Trust, The Royal infirmary
Corresponding Author: Stephen Moore s.moore11nhs@gmail.com
1Clinical history
A 27 year old female patient presented with a known pregnancy of 11 weeks and left sided flank pain. Clinical examination demonstrated focal tenderness in the left upper quadrant however, was otherwise unremarkable. A positive urine dipstick test confirmed the presence of a urinary tract infection (UTI) and raised the suspicion of left sided pyelonephritis. An ultrasound scan was requested to review the urinary tract for any structural abnormalities.
2Imaging findings
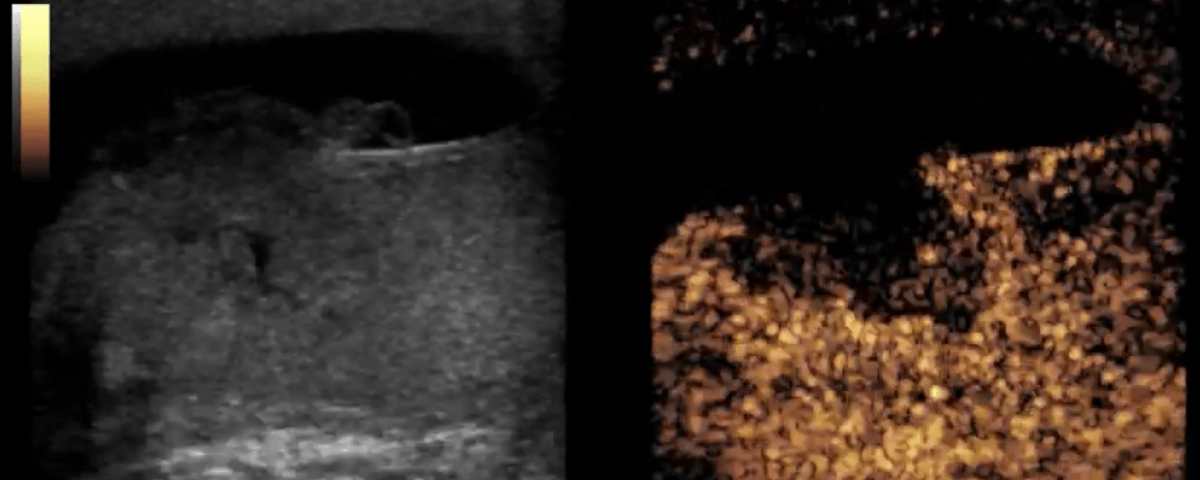
Ultrasound demonstrated an isoechoic area of heterogeneity within the renal cortex of the left kidney (Fig 1), this correlated to the point of maximum tenderness for the patient and was suggestive of acute focal pyelonephritis. The patient was given oral antibiotics and discharged in due course.
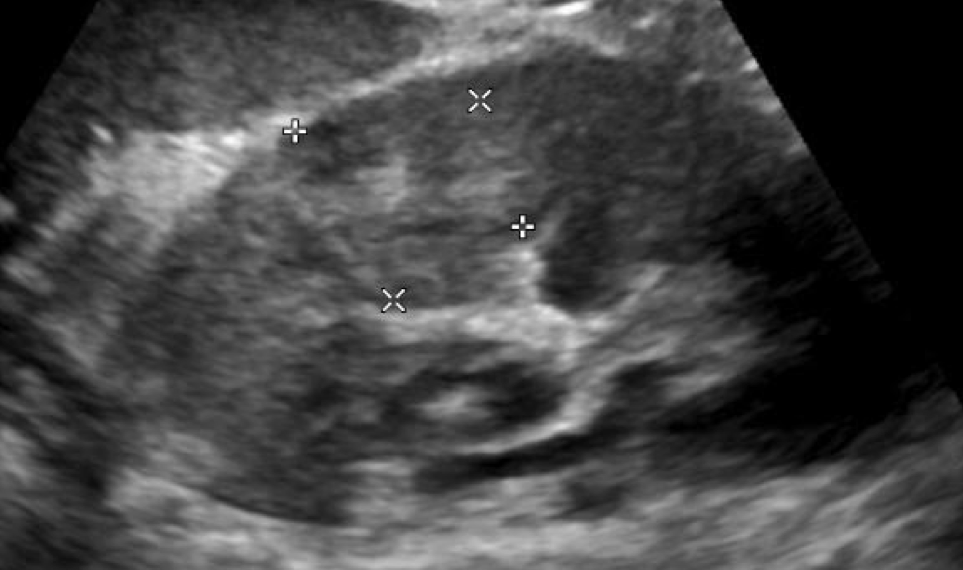
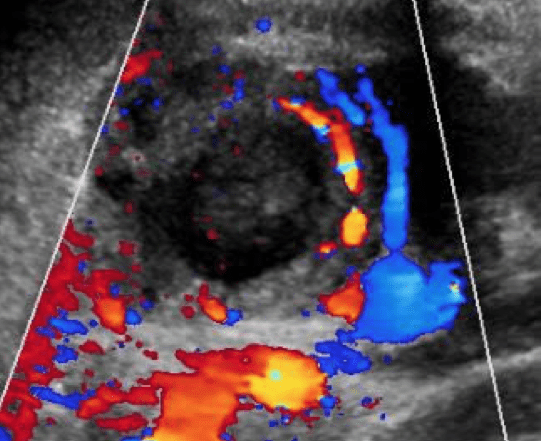
The patient re-presented 16 days later with worsening left flank pain. A second ultrasound was conducted to assess for any resolution or progression of the known left sided focal pyelonephritis. Ultrasound demonstrated a trace of perinephric fluid and a thick walled, complex, cystic mass with internal debris and septations. This lesion occupied the previously identified region of infection. Colour doppler demonstrated a peripheral halo of increased vascularity surrounding the lesion (Fig 2&3). These findings were suggestive of renal abscess formation.
Magnetic Resonance Imaging (MRI) was undertaken to confirm the diagnosis of a left renal abscess (Fig 4) and recommended ultrasound-guided percutaneous drainage (UGPD) which successfully drained ~2ml of pus from the lesion. The patient progressed well and was discharged in due course with no further adverse effects to date.
The patient re-presented 16 days later with worsening left flank pain. A second ultrasound was conducted to assess for any resolution or progression of the known left sided focal pyelonephritis. Ultrasound demonstrated a trace of perinephric fluid and a thick walled, complex, cystic mass with internal debris and septations. This lesion occupied the previously identified region of infection. Colour doppler demonstrated a peripheral halo of increased vascularity surrounding the lesion (Fig 2&3). These findings were suggestive of renal abscess formation.
Magnetic Resonance Imaging (MRI) was undertaken to confirm the diagnosis of a left renal abscess (Fig 4) and recommended ultrasound-guided percutaneous drainage (UGPD) which successfully drained ~2ml of pus from the lesion. The patient progressed well and was discharged in due course with no further adverse effects to date.
3Diagnosis
The case presented demonstrates textbook ultrasound appearances of acute focal pyelonephritis progressing to a focal renal abscess. These findings were confirmed on MRI with a DW-MRI scan series. The utilisation of ultrasound and MRI was opted for to avoid exposing a young, pregnant female to ionising radiation.
4Discussion - Background
Acute pyelonephritis is a bacterial infection of the renal tract commonly affecting renal parenchyma (1). The most common causal bacteria for acute pyelonephritis is Escherichia coli which is complicated by the rising incidence of antibiotic resistance (1).
Pyelonephritis affects ~28/10,000 people (2) and is more common in females aged 18-49 (1-3). Approximately 7% of all cases of acute pyelonephritis require hospitalisation (2), however with increasing antibiotic resistance this figure could rise. Risk-factors for pyelonephritis include diabetes, sickle-cell, female gender, and pregnancy (2,3). Acute pyelonephritis affects up to 2% of pregnancies often occurring the second trimester (3). However poorly managed or antibiotic resistant pyelonephritis can progress to abscess formation, sepsis and renal failure (4).
Pyelonephritis affects ~28/10,000 people (2) and is more common in females aged 18-49 (1-3). Approximately 7% of all cases of acute pyelonephritis require hospitalisation (2), however with increasing antibiotic resistance this figure could rise. Risk-factors for pyelonephritis include diabetes, sickle-cell, female gender, and pregnancy (2,3). Acute pyelonephritis affects up to 2% of pregnancies often occurring the second trimester (3). However poorly managed or antibiotic resistant pyelonephritis can progress to abscess formation, sepsis and renal failure (4).
5Discussion - Clinical Perspective
The diagnosis of UTI’s is often undertaken with clinical examination and a urine dipstick test. A urine dipstick test has a sensitivity and specificity of ~75-84% and 82-98% respectively (5) and the combination of clinical symptoms and positive urine cultures is often sufficient to achieve a diagnosis. In cases where pyelonephritis is suspected Computed Tomography is the modality of choice (2-4) however, in pregnant women ultrasound should be undertaken due to its ionising radiation free nature (4).
Ultrasound appearances of acute pyelonephritis are subtle and rarely present (4). One study documented positive ultrasound findings for pyelonephritis in only 24% of confirmed cases (4). When present, ultrasound appearances of pyelonephritis demonstrate parenchymal changes which may be isoechoic and heterogeneous with increased vascularity on colour doppler imaging (4). Other findings of pyelonephritis include renal enlargement, loss of corticomedullary differentiation and abscess formation (4).
When pyelonephritis progresses to a renal abscess, ultrasound demonstrates a progressive change over time (6). Early abscess formation demonstrates a focal area of reduced echogenicity and hypovascularity on colour doppler interrogation (6). As a renal abscess progresses it may undergo liquefaction resulting in a thick-walled, complex cystic lesion with internal debris and a hyperaemic rim on colour doppler (6).
MRI can confirm renal abscess formation within the pregnant population due to its ionising radiation free nature (6). MRI confirms renal abscess formation with Diffusion Weighted MRI (DW-MRI) (6) which demonstrates suppressed/ restricted diffusion within the abscess body (6).
UGPD of renal abscesses as treatment is often reserved for serious cases or cases which do not respond to antibiotic treatment (7). UGPD are often successful however, due to the complex appearances of abscesses on B-mode ultrasound; targeting purely cystic portions of the lesion can be challenging for the operator (8). The use of Contrast Enhanced Ultrasound (CEUS) can help delineate between the enhancing renal parenchyma and the avascular cystic regions of the collection (8). CEUS may also help improve targeting of the fluid components of the abscess and lead to better procedural success rates (8). However, the use of CEUS in pregnancy is not advocated owing to a lack of research into this area.
Ultrasound appearances of acute pyelonephritis are subtle and rarely present (4). One study documented positive ultrasound findings for pyelonephritis in only 24% of confirmed cases (4). When present, ultrasound appearances of pyelonephritis demonstrate parenchymal changes which may be isoechoic and heterogeneous with increased vascularity on colour doppler imaging (4). Other findings of pyelonephritis include renal enlargement, loss of corticomedullary differentiation and abscess formation (4).
When pyelonephritis progresses to a renal abscess, ultrasound demonstrates a progressive change over time (6). Early abscess formation demonstrates a focal area of reduced echogenicity and hypovascularity on colour doppler interrogation (6). As a renal abscess progresses it may undergo liquefaction resulting in a thick-walled, complex cystic lesion with internal debris and a hyperaemic rim on colour doppler (6).
MRI can confirm renal abscess formation within the pregnant population due to its ionising radiation free nature (6). MRI confirms renal abscess formation with Diffusion Weighted MRI (DW-MRI) (6) which demonstrates suppressed/ restricted diffusion within the abscess body (6).
UGPD of renal abscesses as treatment is often reserved for serious cases or cases which do not respond to antibiotic treatment (7). UGPD are often successful however, due to the complex appearances of abscesses on B-mode ultrasound; targeting purely cystic portions of the lesion can be challenging for the operator (8). The use of Contrast Enhanced Ultrasound (CEUS) can help delineate between the enhancing renal parenchyma and the avascular cystic regions of the collection (8). CEUS may also help improve targeting of the fluid components of the abscess and lead to better procedural success rates (8). However, the use of CEUS in pregnancy is not advocated owing to a lack of research into this area.
6Discussion - Therapy Planning
The use of ultrasound in the diagnosis and monitoring of acute focal pyelonephritis and its progression to renal abscesses, or to resolution can help guide patients management, if the imaging findings worsen despite oral antibiotics then therapy planning can be adjusted to a more aggressive intravenous antibiotic to help ensure optimal care for the patient.
7Teaching Points and Outcome
This case highlights how subtle ultrasound findings can progress to a more advanced and serious condition requiring percutaneous drainage. To date there have been no complications experienced by the patient and the fetal progression is unremarkable.
8References
[1] Colgan, R., Williams, M and Johnson, J. (2011) ‘Diagnosis and Treatment of Acute Pyelonephritis in Women’, American Family Physician, 84(5), pp. 519-526 doi / PMID: 21888302
[2] Medina, M and Castillo-Pino, E. (2019) ‘An introduction to the epidemiology and burden of urinary tract infections’, Therapeutic Advances in Urology, 11(1), pp. 3-7 doi: 10.1177/1756287219832172
[3] Dawkins, JC., Fletcher, HM., Rattray, CA., Reid, M and Gordon-Strachan, G. (2012) ‘Acute Pyelonephritis in Pregnancy: A Retrospective Descriptive Hospital Based Study’, International Scholarly Research Network Obstetrics and Gynaecology, 2012(1), pp. 1-6 doi: 10.5402/2012/519321
[4] William, DC., Brent, JD and Mark, DT (2008) ‘From the archives of the AFIP Pyelonephritis: Radiologic-Pathologic Review’, RadioGraphics, 28(1), pp. 255-278 doi: https://doi.org/10.1148/rg.281075171
[5] Ramakrishnan, K and Scheid, DC (2005) ‘Diagnosis and Management of Acute Pyelonephritis in Adults’, American Family Physician, 71(5) pp. 933-942 doi/ PMID: 15768623
[6] Das, CJ., Ahmad, Z., Sharma, S and Gupta, AK (2014) ‘Multimodality imaging of renal inflammatory lesions’, World Journal of Radiology, 6(11) pp. 865-873 doi: 10.4329/wjr.v6.i11.865
[7] Rai, RS., Karan, SC and A Kayastha, SM (2007) ‘Renal and Perinephric Abscesses Revisited’, Medical Journal Armed Forces India, 63(3), pp. 223-225 doi: https://doi.org/10.1016/S0377-1237(07)80139-0
[8] Huang, DY. Yusuf, GT., Daneshi, M., Ramnarine, R., Deganello, A., Sellars, ME., Sidhu, PS (2018) ‘Contrast-enhanced ultrasound (CEUS) in abdominal intervention’, Abdominal Radiology, 43(4), pp. 960-976 doi: 10.1007/s00261-018-1473-8.
[2] Medina, M and Castillo-Pino, E. (2019) ‘An introduction to the epidemiology and burden of urinary tract infections’, Therapeutic Advances in Urology, 11(1), pp. 3-7 doi: 10.1177/1756287219832172
[3] Dawkins, JC., Fletcher, HM., Rattray, CA., Reid, M and Gordon-Strachan, G. (2012) ‘Acute Pyelonephritis in Pregnancy: A Retrospective Descriptive Hospital Based Study’, International Scholarly Research Network Obstetrics and Gynaecology, 2012(1), pp. 1-6 doi: 10.5402/2012/519321
[4] William, DC., Brent, JD and Mark, DT (2008) ‘From the archives of the AFIP Pyelonephritis: Radiologic-Pathologic Review’, RadioGraphics, 28(1), pp. 255-278 doi: https://doi.org/10.1148/rg.281075171
[5] Ramakrishnan, K and Scheid, DC (2005) ‘Diagnosis and Management of Acute Pyelonephritis in Adults’, American Family Physician, 71(5) pp. 933-942 doi/ PMID: 15768623
[6] Das, CJ., Ahmad, Z., Sharma, S and Gupta, AK (2014) ‘Multimodality imaging of renal inflammatory lesions’, World Journal of Radiology, 6(11) pp. 865-873 doi: 10.4329/wjr.v6.i11.865
[7] Rai, RS., Karan, SC and A Kayastha, SM (2007) ‘Renal and Perinephric Abscesses Revisited’, Medical Journal Armed Forces India, 63(3), pp. 223-225 doi: https://doi.org/10.1016/S0377-1237(07)80139-0
[8] Huang, DY. Yusuf, GT., Daneshi, M., Ramnarine, R., Deganello, A., Sellars, ME., Sidhu, PS (2018) ‘Contrast-enhanced ultrasound (CEUS) in abdominal intervention’, Abdominal Radiology, 43(4), pp. 960-976 doi: 10.1007/s00261-018-1473-8.