Student Image Challenge 101
February 27, 2024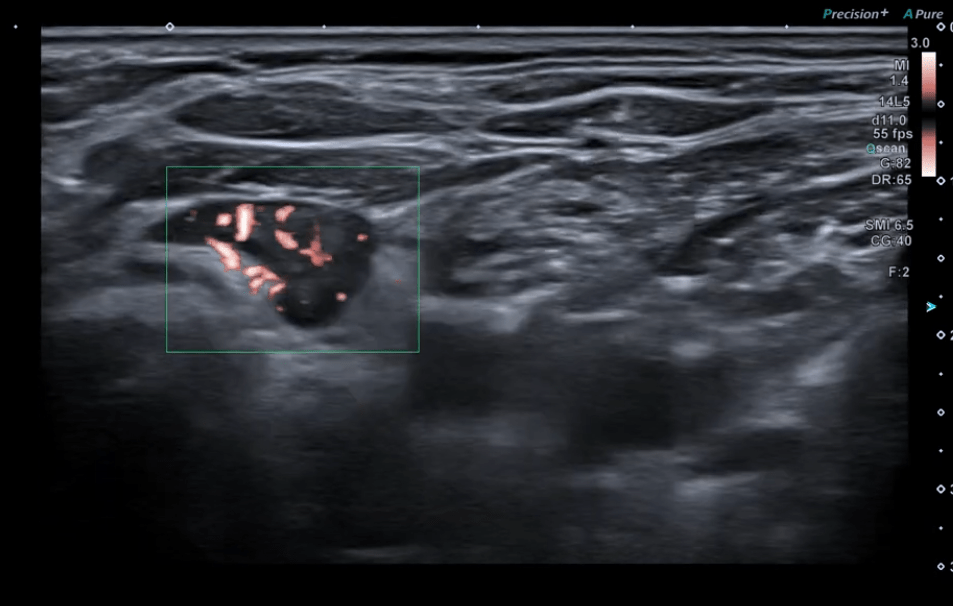
Student Image Challenge 102
March 7, 2024SUBMIT YOUR CASE
EFSUMB invites submission of interesting cases for the website section 'Case of the Month'. All CoM submissions are eligible for selection for free registration at the next Euroson congress. Two cases that receive the most 'likes' in a year will receive free registration for the next EUROSON congress and the third most liked liked case will receive a cash prize of 100 EUR.
Sliding hiatal hernia in 11-month old boy: role of ultrasonography
Authors: Fufezan Otilia Maria, Totelecan Alexandru
Department of Radiology, Emergency Children Hospital, Cluj-Napoca
1Clinical History
The 11 months old male patient was brought in the Department for persistent postprandial regurgitations starting from 1 month of age. He received proton pump inhibitor treatment from the age of 4 months up to present. Two weeks ago, the symptomatology worsened, with reported blood-stained vomit and melena, leading to hospitalization for further investigations.
2Image findings
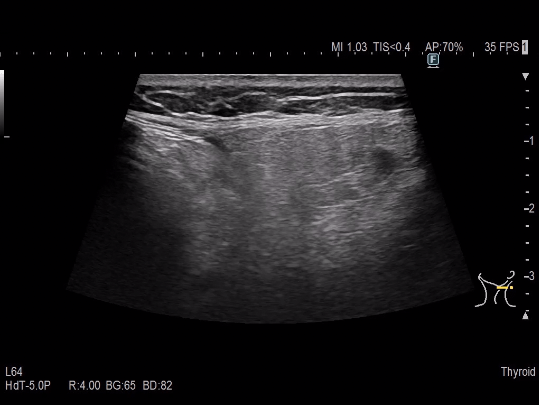
Abdominal ultrasound was performed to evaluate gastroesophageal reflux and gastric emptying.
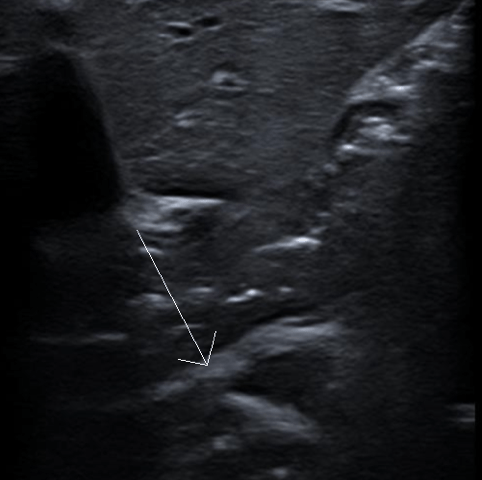
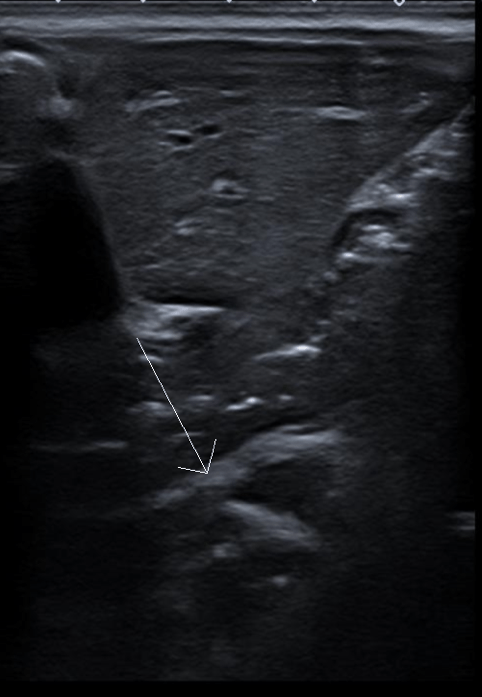
The examination was performed a jeun, at 1 hour and again at 1 hour 30 minutes postprandial (breastfeeding). The examinations showed normal gastric emptying. The pyloric antrum was permissive. The ultrasound (longitudinal scan) revealed supradiaphragmatic sliding of the gastric fundus and enlargement of the esophageal hiatus (up to 2 cm), suggesting a hiatus hernia (Fig. 1 and Movie 1).
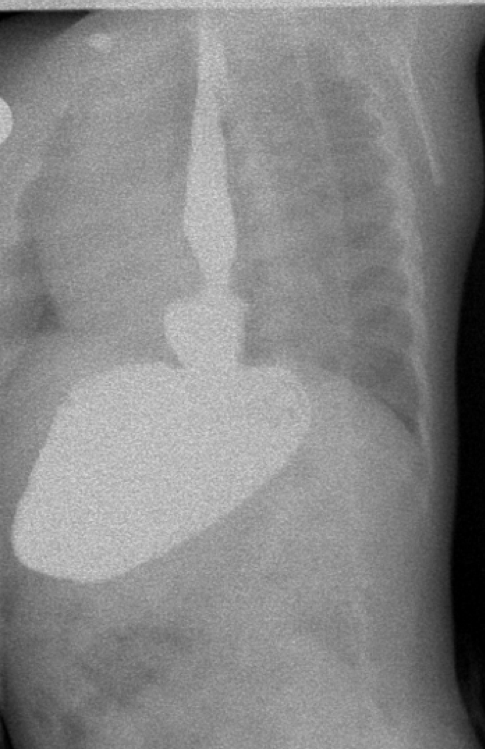
In addition to US, the barium swallow fluoroscopy examination was recommended to confirm the suspicion. This procedure showed a dilated esophagus and a sliding hiatal hernia with significant enlargement of the diaphragmatic hiatus and gastroesophageal junction (GEJ) localized 2.5 cm above it (Fig. 2).
An upper gastrointestinal endoscopy was also performed, confirming the sliding hiatal hernia, additionally revealing non-circumferential distributed mucosal breaks above the GEJ. The gastric and duodenal mucosa were not affected.
The examination was performed a jeun, at 1 hour and again at 1 hour 30 minutes postprandial (breastfeeding). The examinations showed normal gastric emptying. The pyloric antrum was permissive. The ultrasound (longitudinal scan) revealed supradiaphragmatic sliding of the gastric fundus and enlargement of the esophageal hiatus (up to 2 cm), suggesting a hiatus hernia (Fig. 1 and Movie 1).
In addition to US, the barium swallow fluoroscopy examination was recommended to confirm the suspicion. This procedure showed a dilated esophagus and a sliding hiatal hernia with significant enlargement of the diaphragmatic hiatus and gastroesophageal junction (GEJ) localized 2.5 cm above it (Fig. 2).
An upper gastrointestinal endoscopy was also performed, confirming the sliding hiatal hernia, additionally revealing non-circumferential distributed mucosal breaks above the GEJ. The gastric and duodenal mucosa were not affected.
3Diagnosis
Congenital hiatal hernia - type 1 with esophagitis grade C.
4Discussion
BACKGROUND:
Hiatal hernia is a condition where a part of the stomach protrudes into the chest through the diaphragm. It's often caused by a weakening of the muscles and tissues that support the diaphragm. There are four types of hiatus hernia: type 1 - sliding, type 2 - paraesophageal and type 3 - a combination of the first two. Type 4 hiatal hernia involves herniation of other organs (omentum, colon, small intestine, peritoneum and spleen). Sliding hernias are more common and usually don't cause complications, while paraesophageal hernias can be more serious and may require treatment. It's important to note that, by guidelines, hiatal hernia can be diagnosed through imaging tests like endoscopy or barium swallow. Ultrasound is therefore not standardized as a primary investigation method, although the non-invasive characteristic and the absence of ionizing radiation would be a big advantage in the paediatric population.
CLINICAL PERSPECTIVE:
Signs and symptoms of hiatal hernia include vomiting, failure to thrive and dysphagia. In the sliding hernia the pathological complications are the result of gastro-esophageal reflux and persistent vomiting. These may be failure to thrive, respiratory infections and esophagitis with its complications. Regular follow-up visits with appropriate clinical assessments, diagnostic imaging, and endoscopic evaluations may be required to ensure the ongoing effectiveness of the selected therapeutic approach.
THERAPY PLANNING:
Given the severity of the symptoms, therapy planning should involve a multidisciplinary approach including paediatric gastroenterologists, surgeons and radiologists. The primary therapeutic goal would be to address the underlying causes and alleviate the associated symptoms. This may include a combination of pharmacological and non-pharmacological interventions. In the short term, the patient may require acid suppression therapy to manage esophagitis and control symptoms. Additionally, non-pharmacological strategies, such as dietary modifications (frequent small feeds should be given) and positional therapy, may be recommended to reduce regurgitation and improve feeding tolerance. Sliding hernias have two broad indications for surgery: 1) failure of conservative treatment or 2) dysphagia and bleeding (signs of severe esophagitis). In the present case the blood-stained vomiting, melena and esophagitis were clear indicators for surgical treatment. Laparoscopic hernia repair and Nissen fundoplication is considered safe and effective, making it the preferred intervention in our patient.
OUTCOME & PROGNOSIS:
Laparoscopic hernia repair and Nissen fundoplication is reported as a safe and effective procedure for oesophageal hiatal hernia patients. Most commonly seen, intra- and postoperative complications include vagus nerve injury, partial spleen infarction, oesophageal stenosis and gastroesophageal reflux. In terms of long term complications, a recurrent hiatal hernia must be taken into consideration. The present patient quality of life was significantly improved after the surgical treatment, without further gastroesophageal reflux symptoms.
Hiatal hernia is a condition where a part of the stomach protrudes into the chest through the diaphragm. It's often caused by a weakening of the muscles and tissues that support the diaphragm. There are four types of hiatus hernia: type 1 - sliding, type 2 - paraesophageal and type 3 - a combination of the first two. Type 4 hiatal hernia involves herniation of other organs (omentum, colon, small intestine, peritoneum and spleen). Sliding hernias are more common and usually don't cause complications, while paraesophageal hernias can be more serious and may require treatment. It's important to note that, by guidelines, hiatal hernia can be diagnosed through imaging tests like endoscopy or barium swallow. Ultrasound is therefore not standardized as a primary investigation method, although the non-invasive characteristic and the absence of ionizing radiation would be a big advantage in the paediatric population.
CLINICAL PERSPECTIVE:
Signs and symptoms of hiatal hernia include vomiting, failure to thrive and dysphagia. In the sliding hernia the pathological complications are the result of gastro-esophageal reflux and persistent vomiting. These may be failure to thrive, respiratory infections and esophagitis with its complications. Regular follow-up visits with appropriate clinical assessments, diagnostic imaging, and endoscopic evaluations may be required to ensure the ongoing effectiveness of the selected therapeutic approach.
THERAPY PLANNING:
Given the severity of the symptoms, therapy planning should involve a multidisciplinary approach including paediatric gastroenterologists, surgeons and radiologists. The primary therapeutic goal would be to address the underlying causes and alleviate the associated symptoms. This may include a combination of pharmacological and non-pharmacological interventions. In the short term, the patient may require acid suppression therapy to manage esophagitis and control symptoms. Additionally, non-pharmacological strategies, such as dietary modifications (frequent small feeds should be given) and positional therapy, may be recommended to reduce regurgitation and improve feeding tolerance. Sliding hernias have two broad indications for surgery: 1) failure of conservative treatment or 2) dysphagia and bleeding (signs of severe esophagitis). In the present case the blood-stained vomiting, melena and esophagitis were clear indicators for surgical treatment. Laparoscopic hernia repair and Nissen fundoplication is considered safe and effective, making it the preferred intervention in our patient.
OUTCOME & PROGNOSIS:
Laparoscopic hernia repair and Nissen fundoplication is reported as a safe and effective procedure for oesophageal hiatal hernia patients. Most commonly seen, intra- and postoperative complications include vagus nerve injury, partial spleen infarction, oesophageal stenosis and gastroesophageal reflux. In terms of long term complications, a recurrent hiatal hernia must be taken into consideration. The present patient quality of life was significantly improved after the surgical treatment, without further gastroesophageal reflux symptoms.
5Teaching Points
Although abdominal ultrasound is not presented as a current imaging diagnostic method by the guidelines on hiatal hernia, it can be considered a useful examination especially in pediatric patients, where avoiding ionizing radiation is very important. In the present case, both the barium swallow fluoroscopy and the upper digestive tract endoscopy confirmed the pathological findings seen on the ultrasound examination, highlighting its potential contribution in hiatal hernia diagnosis.
6References
1.) Yu HX, Han CS, Xue JR, Han ZF, Xin H . Esophageal hiatal hernia: risk, diagnosis and management, Expert Rev Gastroenterol Hepatol 2018; 12: 319-329.
2.) Esposito F, Antonini AE, Brusciano V et al. Para-oesophageal hernia in 4-month-old girl: possible role of ultrasound—case report and literature review. J Ultrasound 2023; 26: 945–950.
3.) Lister J. Hiatus hernia in children. Postgrad Med J 1972; 48:501-6.
4.) Garvey EM, Ostlie DJ. Hiatal and paraesophageal hernia repair in pediatric patients. Semin Pediatr Surg.2017; 26: 61-66.
5.) Sfara A, Dumitrascu DL. The management of hiatal hernia: an update on diagnosis and treatment. Med Pharm Rep 2019; 92:321-325. .
6.) Cheng C, Wu Y, Pan W, Wang J, Wu Z, Lv F. Follow-up report of laparoscopic fundoplication in different types of oesophageal hiatal hernia in children. J Laparoendosc Adv Surg Tech A 2019; 29: 1320-1324.
2.) Esposito F, Antonini AE, Brusciano V et al. Para-oesophageal hernia in 4-month-old girl: possible role of ultrasound—case report and literature review. J Ultrasound 2023; 26: 945–950.
3.) Lister J. Hiatus hernia in children. Postgrad Med J 1972; 48:501-6.
4.) Garvey EM, Ostlie DJ. Hiatal and paraesophageal hernia repair in pediatric patients. Semin Pediatr Surg.2017; 26: 61-66.
5.) Sfara A, Dumitrascu DL. The management of hiatal hernia: an update on diagnosis and treatment. Med Pharm Rep 2019; 92:321-325. .
6.) Cheng C, Wu Y, Pan W, Wang J, Wu Z, Lv F. Follow-up report of laparoscopic fundoplication in different types of oesophageal hiatal hernia in children. J Laparoendosc Adv Surg Tech A 2019; 29: 1320-1324.