- European Federation of Societies for Ultrasound in Medicine and Biology ~ Educating all for competence to practice ultrasound safely

FRANCE – SFR
January 21, 2021
Student Image Challenge 81 (part 1)
January 28, 2021Acute scrotal pain in a 12-year-old boy
AUTHORS
Jonathan Cohen, Department of Radiology, Rigshospitalet, Copenhagen University Hospital
Caroline Ewertsen, Department of Radiology, Rigshospitalet, Copenhagen University Hospital
Jonathan Cohen, Department of Radiology, Rigshospitalet, Copenhagen University Hospital
Caroline Ewertsen, Department of Radiology, Rigshospitalet, Copenhagen University Hospital
1Clinical history
A 12-year-old boy was admitted to our hospital after one day of pain in the right scrotum. The pain was constant, radiating a bit towards the right groin, and was exacerbated by palpation and movement. There were no abdominal or urinal symptoms, and he did not have a fever. He was in good general health.
Physical examination showed a tender right testicle with a slightly swollen blue dot-shaped miscoloration of the skin at the level of the upper pole of the testicle. The left testicle was normal. A urine dipstick test was negative.
Physical examination showed a tender right testicle with a slightly swollen blue dot-shaped miscoloration of the skin at the level of the upper pole of the testicle. The left testicle was normal. A urine dipstick test was negative.
2Image Findings
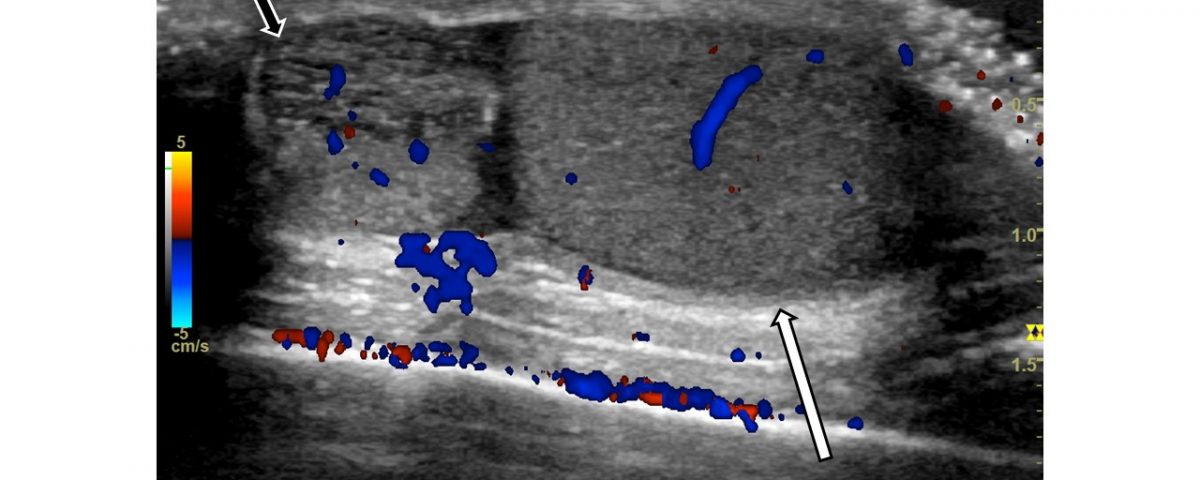
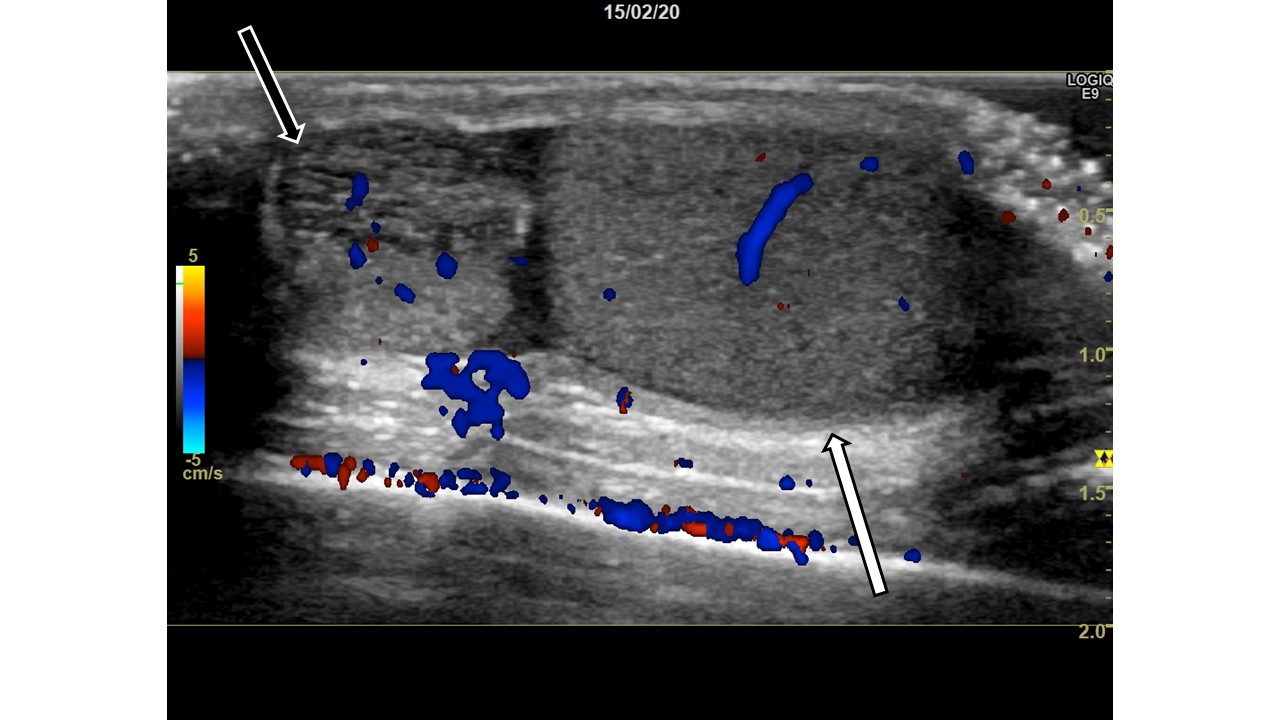
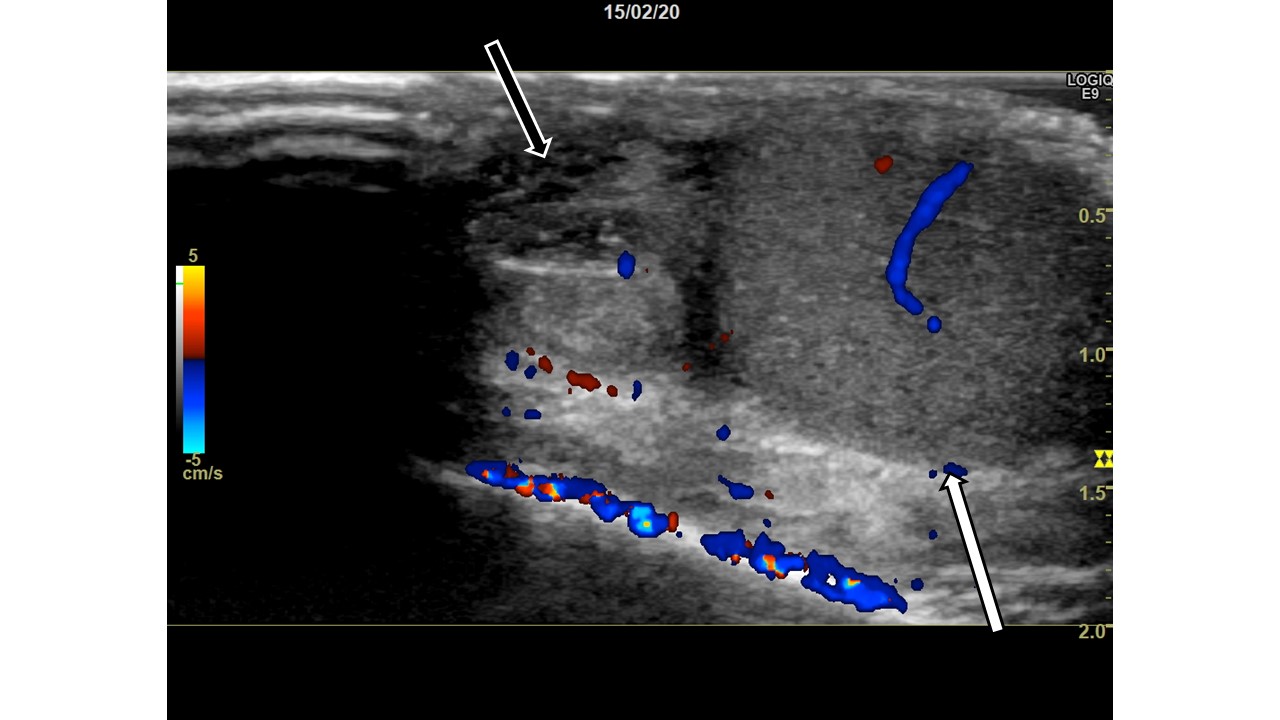
The patient was examined in the supine position with a high frequency linear transducer including color Doppler to determine blood flow, and intermittent Valsalva maneuver. The following images are from the examination.
Image 1: Right scrotum, sagittal view, with color Doppler. Normal testis (white arrow) with normal blood flow. At the upper pole of the testis, a heterogenous slightly hypoechoic lesion (black arrow) is noted with scarce blood flow and slight surrounding edema. No enhancement is seen behind the lesion.
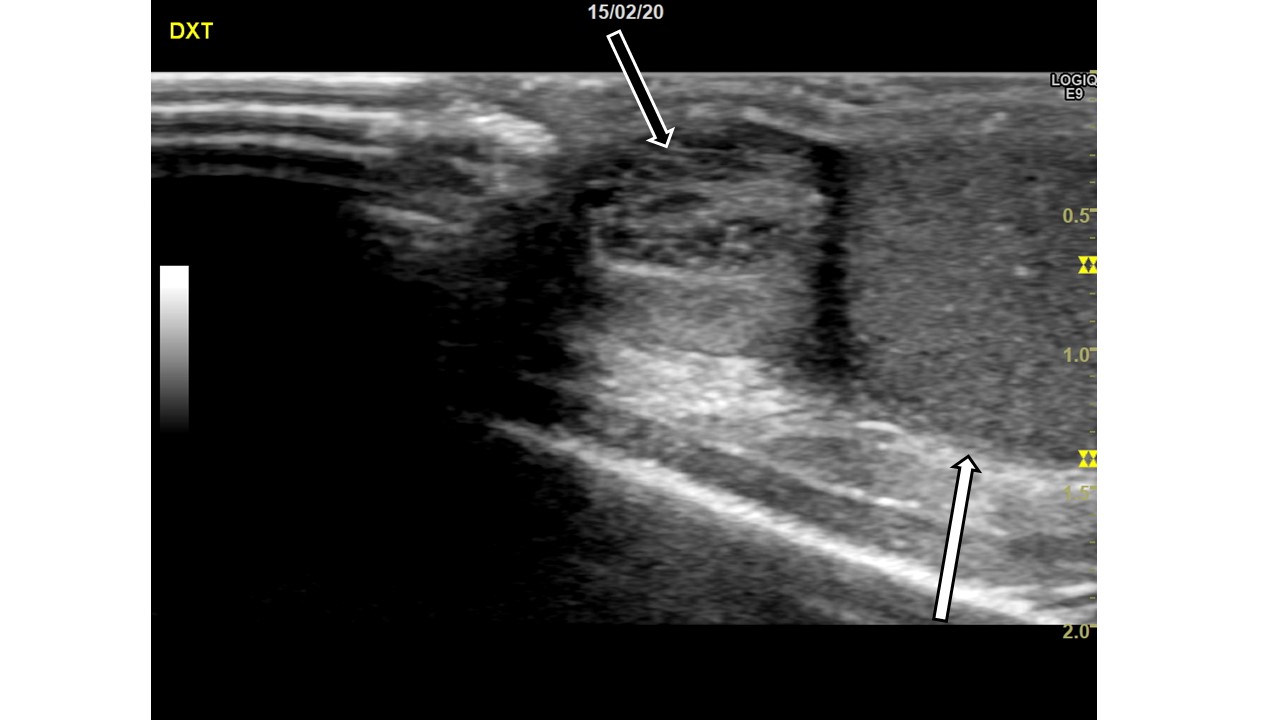
Image 2: Right scrotum, sagittal view. Slightly cranial to image 1. White arrow is the testis, black arrow is the lesion.
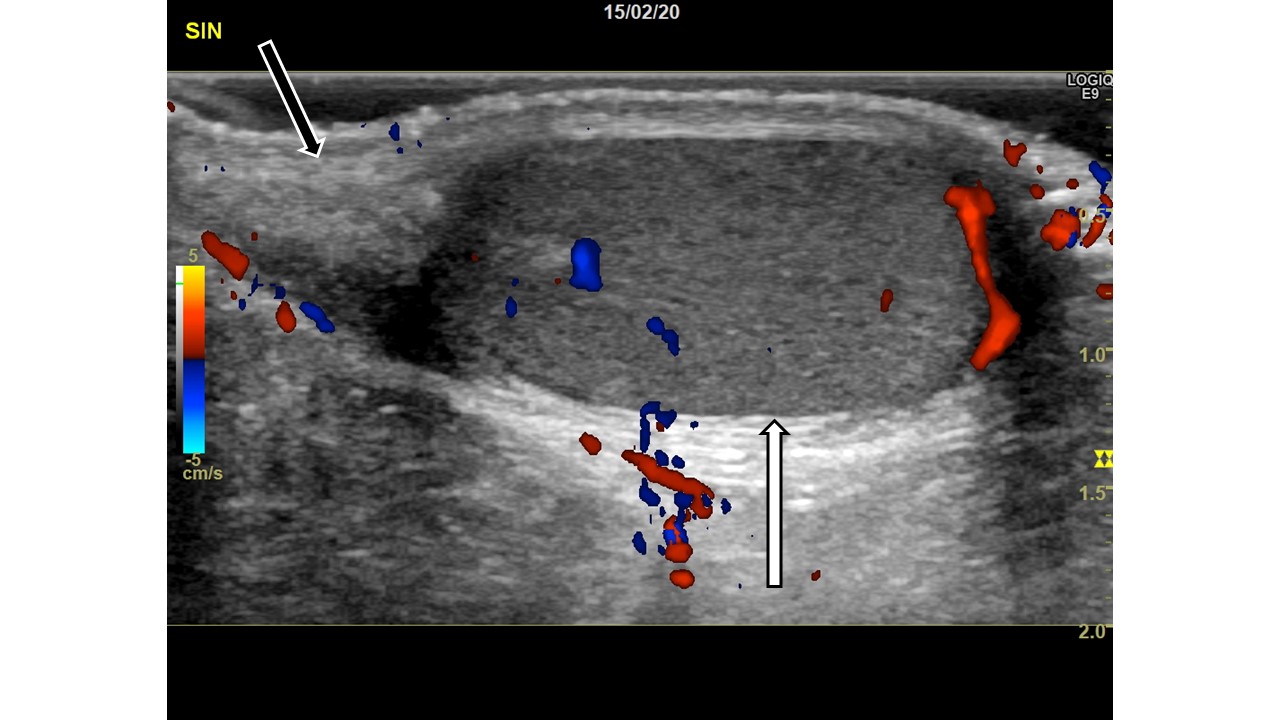
Image 3: Right scrotum, sagittal view. Upper pole of the testis (white arrow). A heterogenous, slightly hypoechoic lesion (black arrow) is visible.
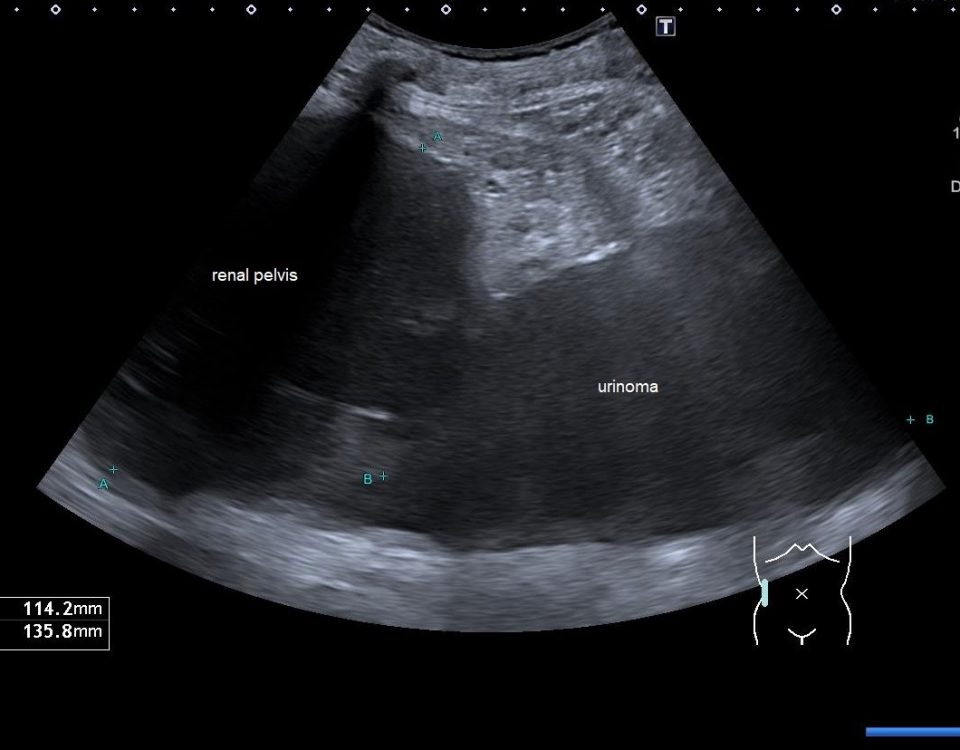
Image 4: Left scrotum, sagital view, with color Doppler. Normal testis with normal blood flow (white arrow). Normal epididymis (black arrow). The appendix epididymis is not clearly distinguishable.
Image 1: Right scrotum, sagittal view, with color Doppler. Normal testis (white arrow) with normal blood flow. At the upper pole of the testis, a heterogenous slightly hypoechoic lesion (black arrow) is noted with scarce blood flow and slight surrounding edema. No enhancement is seen behind the lesion.
Image 2: Right scrotum, sagittal view. Slightly cranial to image 1. White arrow is the testis, black arrow is the lesion.
Image 3: Right scrotum, sagittal view. Upper pole of the testis (white arrow). A heterogenous, slightly hypoechoic lesion (black arrow) is visible.
Image 4: Left scrotum, sagital view, with color Doppler. Normal testis with normal blood flow (white arrow). Normal epididymis (black arrow). The appendix epididymis is not clearly distinguishable.
3Diagnosis
Torsion of the appendix epididymis.
4Discussion
The appendix epididymis and the appendix testis are thought to be embryonic remnants with no vital function. Still, they are highly clinically relevant in the diagnosis of the acute scrotum in pediatric patients, as up to 60% of cases of acute scrotum in children have been reported to arise from torsion of the appendages [1–3].
The appendix epididymis is a small, stalked structure protruding from the head of the epididymis [4,5] not easily discerned from the epididymis unless pathology is present [6]. In the case of a torted appendix, ultrasound findings may include the presence of an enlarged, homo- or heterogenous avascular mass with hyperemia and edema of the surrounding structures [2,5] .
Distinguishing the easily manageable torsion of the appendages from the surgical emergency of testicular torsion or from epididymitis by clinical examination is difficult, as symptoms such as scrotal pain, swelling and erythema overlap [7]. One of the classic clinical features in the presence of a torted appendix is the “blue dot sign” - a bluish discoloration of the scrotal skin overlying the torsed appendage at the upper pole of the testis, although the predictive value of this sign varies between studies [2,3,5,7].
Quick diagnosis is important, as testicular torsion requires immediate surgical intervention. Ultrasound is considered to be both sensitive and specific in discerning testicular torsion from other scrotal pathologies, and findings suggestive of testicular torsion include absent or reduced intra-testicular blood flow compared with the asymptomatic side, twisting of the spermatic cord and abnormal location and appearance of the head of the epididymis [6]. When the diagnosis is uncertain, surgical exploration should be considered [1,7,8].
Torsion of the appendages is most commonly managed conservatively using symptomatic treatment such as non-steroidal anti-inflammatory drugs, bed rest, and scrotal support [5]. Prognosis is good, and lasting injury is rare.
In our case, the patient was indeed treated conservatively, and was discharged within the same day with no complications.
The appendix epididymis is a small, stalked structure protruding from the head of the epididymis [4,5] not easily discerned from the epididymis unless pathology is present [6]. In the case of a torted appendix, ultrasound findings may include the presence of an enlarged, homo- or heterogenous avascular mass with hyperemia and edema of the surrounding structures [2,5] .
Distinguishing the easily manageable torsion of the appendages from the surgical emergency of testicular torsion or from epididymitis by clinical examination is difficult, as symptoms such as scrotal pain, swelling and erythema overlap [7]. One of the classic clinical features in the presence of a torted appendix is the “blue dot sign” - a bluish discoloration of the scrotal skin overlying the torsed appendage at the upper pole of the testis, although the predictive value of this sign varies between studies [2,3,5,7].
Quick diagnosis is important, as testicular torsion requires immediate surgical intervention. Ultrasound is considered to be both sensitive and specific in discerning testicular torsion from other scrotal pathologies, and findings suggestive of testicular torsion include absent or reduced intra-testicular blood flow compared with the asymptomatic side, twisting of the spermatic cord and abnormal location and appearance of the head of the epididymis [6]. When the diagnosis is uncertain, surgical exploration should be considered [1,7,8].
Torsion of the appendages is most commonly managed conservatively using symptomatic treatment such as non-steroidal anti-inflammatory drugs, bed rest, and scrotal support [5]. Prognosis is good, and lasting injury is rare.
In our case, the patient was indeed treated conservatively, and was discharged within the same day with no complications.
5Teaching Point
Torsion of the scrotal appendages is one of the most common findings in the acute scrotum in children. Clinical features and ultrasound examination with colour Doppler are important in ruling out the surgical emergency of testicular torsion. When the diagnosis is unclear, surgical exploration should be considered.
6References
1. Kalfa, N.; Veyrac, C.; Lopez, M.; Lopez, C.; Maurel, A.; Kaselas, C.; Sibai, S.; Arena, F.; Vaos, G.; Bréaud, J.; et al. Multicenter assessment of ultrasound of the spermatic cord in children with acute scrotum. J. Urol. 2007, 177, 297–301; discussion 301.
2. Lev, M.; Ramon, J.; Mor, Y.; Jacobson, J.M.; Soudack, M. Sonographic appearances of torsion of the appendix testis and appendix epididymis in children. J. Clin. Ultrasound 2015, 43, 485–489.
3. Baldisserotto, M.; de Souza, J.C.K.; Pertence, A.P.; Dora, M.D. Color Doppler sonography of normal and torsed testicular appendages in children. AJR. Am. J. Roentgenol. 2005, 184, 1287–92.
4. Sahni, D.; Jit, I.; Joshi, K.; Sanjeev Incidence and structure of the appendices of the testis and epididymis. J. Anat. 1996, 189 ( Pt 2), 341–8.
5. Sellars, M.E.K.; Sidhu, P.S. Ultrasound appearances of the testicular appendages: Pictorial review. Eur. Radiol. 2003, 13, 127–135.
6. Alkhori, N.A.; Barth, R.A. Pediatric scrotal ultrasound: review and update. Pediatr. Radiol. 2017, 47, 1125–1133.
7. Boettcher, M.; Bergholz, R.; Krebs, T.F.; Wenke, K.; Treszl, A.; Aronson, D.C.; Reinshagen, K. Differentiation of epididymitis and appendix testis torsion by clinical and ultrasound signs in children. Urology 2013, 82, 899–904.
8. Yang, C.; Song, B.; Liu, X.; Wei, G.H.; Lin, T.; He, D.W. Acute scrotum in children: An 18-year retrospective study. Pediatr. Emerg. Care 2011, 27, 270–274.
2. Lev, M.; Ramon, J.; Mor, Y.; Jacobson, J.M.; Soudack, M. Sonographic appearances of torsion of the appendix testis and appendix epididymis in children. J. Clin. Ultrasound 2015, 43, 485–489.
3. Baldisserotto, M.; de Souza, J.C.K.; Pertence, A.P.; Dora, M.D. Color Doppler sonography of normal and torsed testicular appendages in children. AJR. Am. J. Roentgenol. 2005, 184, 1287–92.
4. Sahni, D.; Jit, I.; Joshi, K.; Sanjeev Incidence and structure of the appendices of the testis and epididymis. J. Anat. 1996, 189 ( Pt 2), 341–8.
5. Sellars, M.E.K.; Sidhu, P.S. Ultrasound appearances of the testicular appendages: Pictorial review. Eur. Radiol. 2003, 13, 127–135.
6. Alkhori, N.A.; Barth, R.A. Pediatric scrotal ultrasound: review and update. Pediatr. Radiol. 2017, 47, 1125–1133.
7. Boettcher, M.; Bergholz, R.; Krebs, T.F.; Wenke, K.; Treszl, A.; Aronson, D.C.; Reinshagen, K. Differentiation of epididymitis and appendix testis torsion by clinical and ultrasound signs in children. Urology 2013, 82, 899–904.
8. Yang, C.; Song, B.; Liu, X.; Wei, G.H.; Lin, T.; He, D.W. Acute scrotum in children: An 18-year retrospective study. Pediatr. Emerg. Care 2011, 27, 270–274.