- European Federation of Societies for Ultrasound in Medicine and Biology ~ Educating all for competence to practice ultrasound safely

Distal pancreatic stent migration: Could POCUS assist in identifying perforation in primary care? [September 2023]
April 26, 2024
Student Image Challenge 105
May 7, 2024SUBMIT YOUR CASE
EFSUMB invites submission of interesting cases for the website section 'Case of the Month'. All CoM submissions are eligible for selection for free registration at the next Euroson congress. Two cases that receive the most 'likes' in a year will receive free registration for the next EUROSON congress and the third most liked liked case will receive a cash prize of 100 EUR.
Adrenal Haematoma Versus Liver Cyst: Discrimination by Contrast-Enhanced Ultrasound
Authors: Jasmine Bajaj, Timothy Gibran Yusuf, Barbie Giri, Shaheer Baig, Jessica Lubel, Neslihan Isleyen, Priyan Tantrige, Khalid Ballal
– Department of Radiology, Kings College Hospital, London
1Clinical History
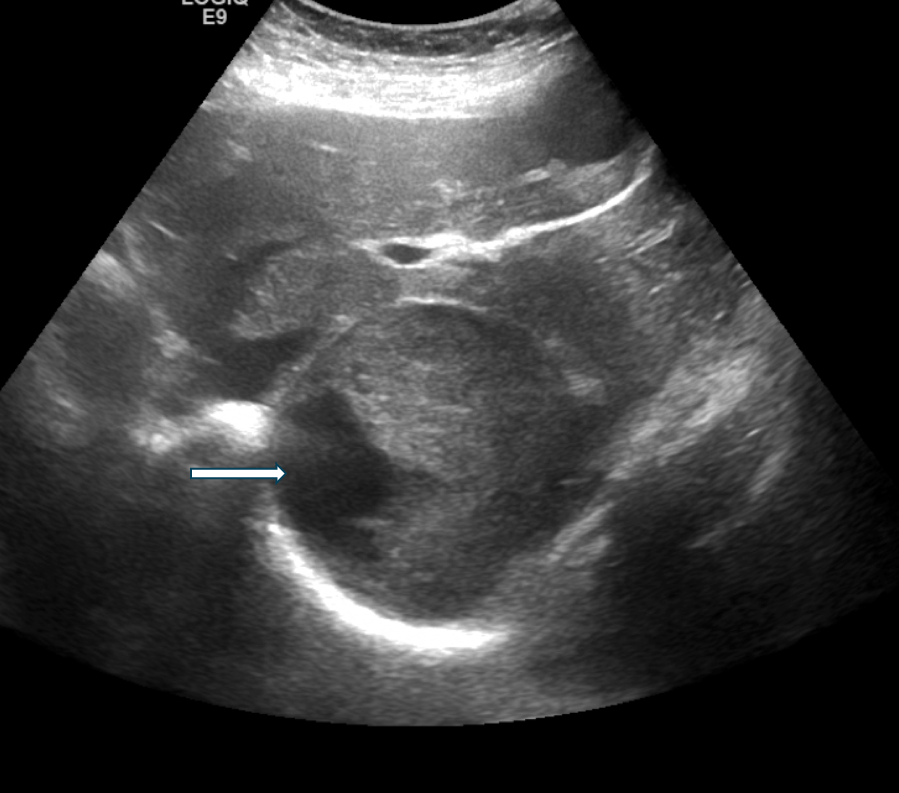
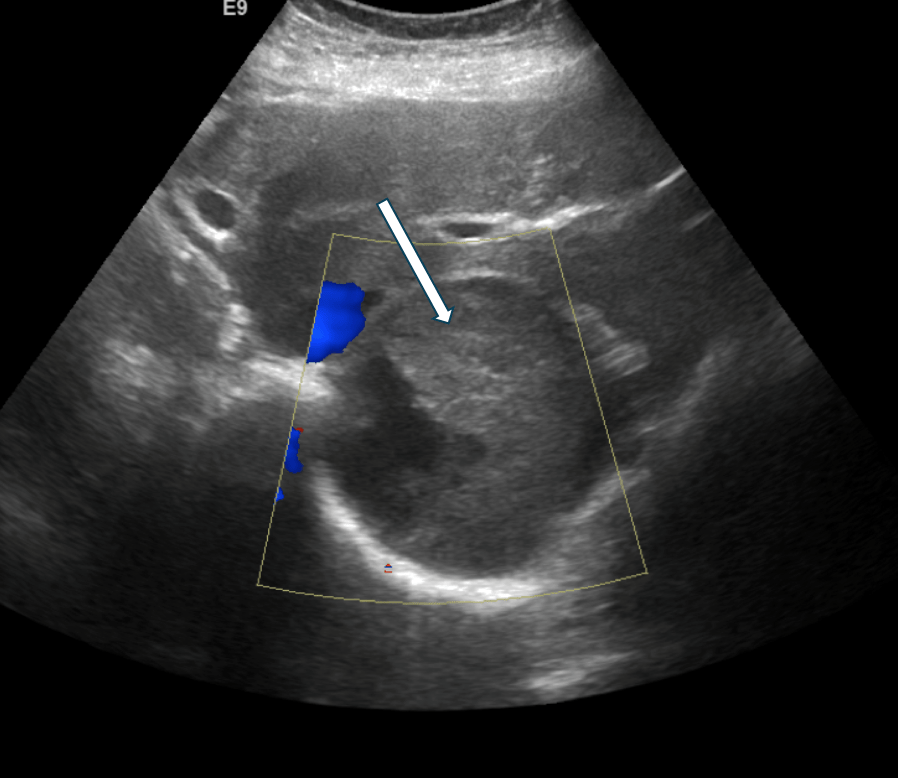
This case report describes the presentation of a 92 year old lady patient who presented to the Accident and Emergency Department with right sided abdominal pain and complained of recent falls and trauma. She underwent a FAST (Focussed Assessment with Sonography in Trauma) scan in the Emergency Department, that revealed a newly diagnosed “liver cyst”. Following best practice guidelines, the “liver cyst” was initially visualized using B-mode ultrasonography, followed by Colour Doppler examination (Figure 1 and 2).
2Image findings
B-mode ultrasound (Figure 1) and colour Doppler (Figure 2) was used to characterise the suspected liver lesion, however this yielded indeterminate results. The scan showed a well defined heterogenous lesion with part cystic and part solid components separated from the liver with a distinct fat line. There was no colour flow demonstrated within the lesion on the Colour Doppler (Figure 2). Given this ambiguity, further assessment with contrast-enhanced ultrasound was deemed necessary.
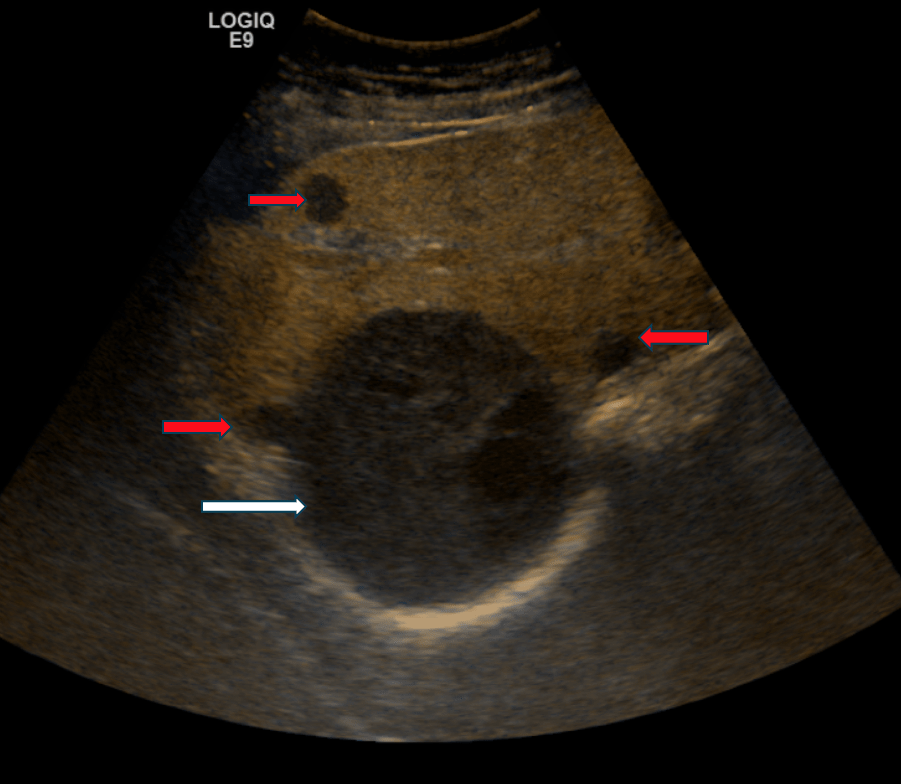
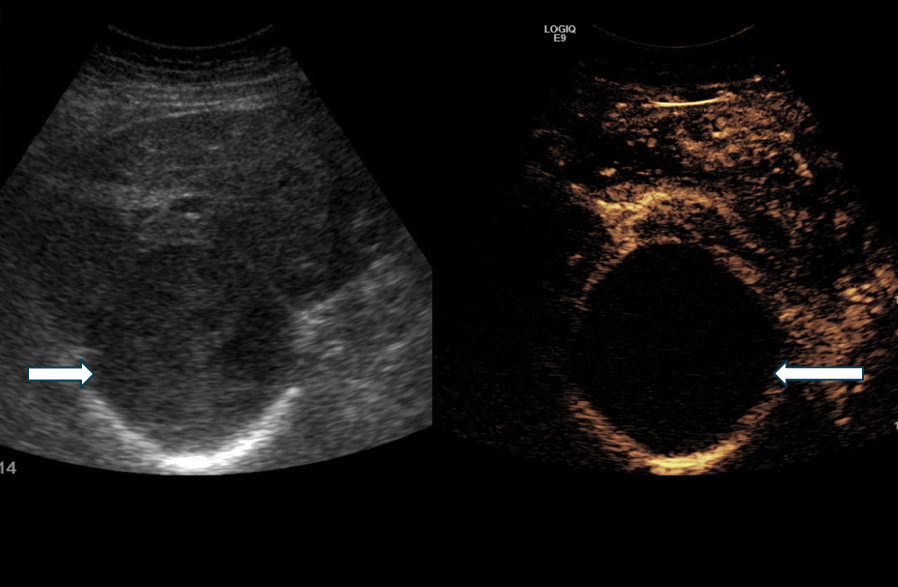
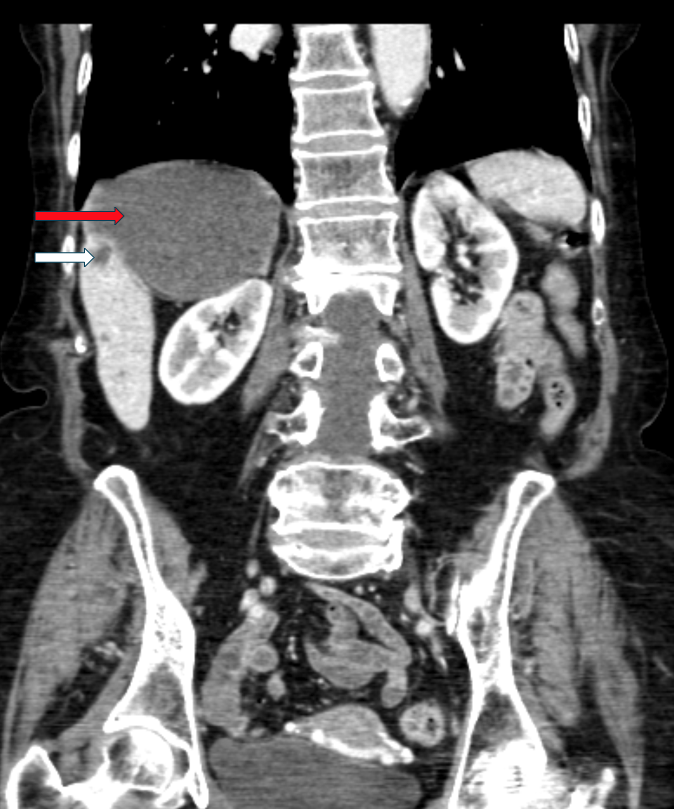
Upon contrast-enhanced ultrasound examination (Figure 3 and 4), the lesion revealed both solid and cystic components. There was once again a fat line noted between the lesion and the liver, confirming an extra- hepatic origin. Notably, no enhancement was observed within the lesion following the injection of contrast agent. In addition, there were simple cysts noted in the liver (Figure 3, Figure 5 and Figure 6), the largest one measuring approximately 45/34mm (Figure 5).
A brief clinical history uncovered a prior incidence of falls and trauma. When combined with the imaging findings, this clinical context strongly supported a diagnosis of an adrenal hematoma.
For confirmation, a Computed Tomography (CT) abdomen and pelvis (Figure 5 and 6) was subsequently performed, that corroborated the above findings.
Upon contrast-enhanced ultrasound examination (Figure 3 and 4), the lesion revealed both solid and cystic components. There was once again a fat line noted between the lesion and the liver, confirming an extra- hepatic origin. Notably, no enhancement was observed within the lesion following the injection of contrast agent. In addition, there were simple cysts noted in the liver (Figure 3, Figure 5 and Figure 6), the largest one measuring approximately 45/34mm (Figure 5).
A brief clinical history uncovered a prior incidence of falls and trauma. When combined with the imaging findings, this clinical context strongly supported a diagnosis of an adrenal hematoma.
For confirmation, a Computed Tomography (CT) abdomen and pelvis (Figure 5 and 6) was subsequently performed, that corroborated the above findings.
3Diagnosis
Adrenal haematoma due to prior trauma.
4Discussion
BACKGROUND:
Adrenal haematomas can manifest with a spectrum of symptoms, ranging from nonspecific abdominal pain to cardiovascular collapse (1). Etiological factors can be primary or secondary; with the latter encompassing trauma, anticoagulant use, pregnancy, acute stressors such as surgery or sepsis, or neoplastic conditions (1). Imaging plays a crucial role in diagnosis, with CT being the primary modality (1). However, in the paediatric population, there is a greater reliance on contrast-enhanced ultrasound and MRI to minimize radiation exposure (1).
Contrast-enhanced ultrasound serves as a valuable tool in distinguishing adrenal hematoma from malignancy (2). For example, in the imaging of malignant adrenal masses such as pheochromocytoma, one would anticipate hypervascularity in certain regions with no contrast enhancement in necrotic areas (3). In contrast to this, adrenal hematomas typically exhibit no enhancement (3).Thus, contrast enhanced ultrasound can confirm the presence of an adrenal haematoma with absence of vascularity. In addition as mentioned above , it is also useful in distinguishing benign from malignant adrenal lesions. Furthermore, contrast-enhanced ultrasound has been extensively utilized for visualizing liver lesions by identifying distinct vascular patterns across arterial, portal, and late phases (4). This modality plays a key role as a safe and effective tool for paediatric patients, allowing for the surveillance of adrenal trauma while minimizing the risks associated with radiation and contrast exposure (5).
CLINICAL PERSPECTIVE:
The presentation of adrenal hematoma can be perplexing, posing a challenge for swift treatment. This is more applicable if it is occult or history of trauma is not forthcoming. Prompt recognition of this condition is imperative. It may manifest with a variety of signs and symptoms, including loin pain, nausea, vomiting, tachycardia, hypotension, and hypertension (particularly if the underlying cause is a pheochromocytoma) (1). Compounding the challenge, laboratory parameters typically appear normal (1). Cortisol levels may fluctuate, being either elevated or reduced depending on the phase of haemorrhage (1).
THERAPY PLANNING and OUTCOME:
Given the potential severity of adrenal hematoma, treatment is tailored to each patient's specific presentation. Conservative management with serial monitoring may be deemed appropriate in some cases (1). Alternatively, interventions such as blood transfusion may be necessary if the patient is hemodynamically unstable (1). In instances of large retroperitoneal haemorrhage, angiography and embolisation could be warranted (1). In the case described, conservative management with serial imaging was employed.
PROGNOSIS:
The prognosis of adrenal hematoma can vary depending on individual presentations (1). In the case of this patient, a favourable prognosis was observed.
Adrenal haematomas can manifest with a spectrum of symptoms, ranging from nonspecific abdominal pain to cardiovascular collapse (1). Etiological factors can be primary or secondary; with the latter encompassing trauma, anticoagulant use, pregnancy, acute stressors such as surgery or sepsis, or neoplastic conditions (1). Imaging plays a crucial role in diagnosis, with CT being the primary modality (1). However, in the paediatric population, there is a greater reliance on contrast-enhanced ultrasound and MRI to minimize radiation exposure (1).
Contrast-enhanced ultrasound serves as a valuable tool in distinguishing adrenal hematoma from malignancy (2). For example, in the imaging of malignant adrenal masses such as pheochromocytoma, one would anticipate hypervascularity in certain regions with no contrast enhancement in necrotic areas (3). In contrast to this, adrenal hematomas typically exhibit no enhancement (3).Thus, contrast enhanced ultrasound can confirm the presence of an adrenal haematoma with absence of vascularity. In addition as mentioned above , it is also useful in distinguishing benign from malignant adrenal lesions. Furthermore, contrast-enhanced ultrasound has been extensively utilized for visualizing liver lesions by identifying distinct vascular patterns across arterial, portal, and late phases (4). This modality plays a key role as a safe and effective tool for paediatric patients, allowing for the surveillance of adrenal trauma while minimizing the risks associated with radiation and contrast exposure (5).
CLINICAL PERSPECTIVE:
The presentation of adrenal hematoma can be perplexing, posing a challenge for swift treatment. This is more applicable if it is occult or history of trauma is not forthcoming. Prompt recognition of this condition is imperative. It may manifest with a variety of signs and symptoms, including loin pain, nausea, vomiting, tachycardia, hypotension, and hypertension (particularly if the underlying cause is a pheochromocytoma) (1). Compounding the challenge, laboratory parameters typically appear normal (1). Cortisol levels may fluctuate, being either elevated or reduced depending on the phase of haemorrhage (1).
THERAPY PLANNING and OUTCOME:
Given the potential severity of adrenal hematoma, treatment is tailored to each patient's specific presentation. Conservative management with serial monitoring may be deemed appropriate in some cases (1). Alternatively, interventions such as blood transfusion may be necessary if the patient is hemodynamically unstable (1). In instances of large retroperitoneal haemorrhage, angiography and embolisation could be warranted (1). In the case described, conservative management with serial imaging was employed.
PROGNOSIS:
The prognosis of adrenal hematoma can vary depending on individual presentations (1). In the case of this patient, a favourable prognosis was observed.
5Teaching Points
1. Adrenal masses can sometimes be misinterpreted as liver lesions, given the proximity of the right lobe of the liver and the right suprarenal gland.
2. Adrenal hematomas typically exhibit no enhancement on contrast-enhanced ultrasound.
3. A comprehensive clinical history is crucial, particularly during dynamic scanning procedures like ultrasound, as it can provide valuable context to complement imaging findings.
4. Contrast-enhanced ultrasound proves to be a robust tool for rapidly identifying adrenal hematomas.
2. Adrenal hematomas typically exhibit no enhancement on contrast-enhanced ultrasound.
3. A comprehensive clinical history is crucial, particularly during dynamic scanning procedures like ultrasound, as it can provide valuable context to complement imaging findings.
4. Contrast-enhanced ultrasound proves to be a robust tool for rapidly identifying adrenal hematomas.
6References
1. Gawande R, Castaneda R, Daldrup-Link HE. Adrenal Hemorrhage. Pearls and Pitfalls in Pediatric Imaging: Variants and Other Difficult Diagnoses. Cambridge University Press. 2012; 9781107017498: 291-293.
2. Piskunowickz M, Stefanowicz J, Batko T et al. Contrast enhanced ultrasound of adrenal hemorrhage. Med Ultrason. 2022; 24(3): 284-289.
3. Sidhu PS, Cantisani V, Dietrich CF et al. The EFSUMB Guidelines and Recommendations for the Clinical Practise of Contrast Enhanced Ultrasound (CEUS) in Non Hepatic -Applications: Update 2017 (Long Version). Ultraschall Med.2018 ; 39(2): e2-e44.
4. D’Onofrio M, Crosara S, De Robartis R et al. Contrast Enhanced Ultrasound of Focal Liver Lesions. AJR Am J Roentgenol. 2015; 205(1): W56-66.
5. Rafailidis V, Deganello A, Sellars ME. Pediatric adrenal trauma: evaluation and follow up with contrast enhanced ultrasound (CEUS). J Ultrasound. 2016; 20(4): 325-331.
2. Piskunowickz M, Stefanowicz J, Batko T et al. Contrast enhanced ultrasound of adrenal hemorrhage. Med Ultrason. 2022; 24(3): 284-289.
3. Sidhu PS, Cantisani V, Dietrich CF et al. The EFSUMB Guidelines and Recommendations for the Clinical Practise of Contrast Enhanced Ultrasound (CEUS) in Non Hepatic -Applications: Update 2017 (Long Version). Ultraschall Med.2018 ; 39(2): e2-e44.
4. D’Onofrio M, Crosara S, De Robartis R et al. Contrast Enhanced Ultrasound of Focal Liver Lesions. AJR Am J Roentgenol. 2015; 205(1): W56-66.
5. Rafailidis V, Deganello A, Sellars ME. Pediatric adrenal trauma: evaluation and follow up with contrast enhanced ultrasound (CEUS). J Ultrasound. 2016; 20(4): 325-331.