- European Federation of Societies for Ultrasound in Medicine and Biology ~ Educating all for competence to practice ultrasound safely

Unclear lesion of the abdominal wall [August 2023]
April 3, 2024
Adrenal Haematoma Versus Liver Cyst: Discrimination by Contrast-Enhanced Ultrasound [October 2023]
May 1, 2024SUBMIT YOUR CASE
EFSUMB invites submission of interesting cases for the website section 'Case of the Month'. All CoM submissions are eligible for selection for free registration at the next Euroson congress. Two cases that receive the most 'likes' in a year will receive free registration for the next EUROSON congress and the third most liked liked case will receive a cash prize of 100 EUR.
Distal pancreatic stent migration: Could POCUS assist in identifying perforation in primary care?
Authors: Tommaso Barnini, Camilla Dalprà, Daria Paladino
– AUSL TOSCANA CENTRO – Sesto Fiorentino, Italy
1Clinical History
Here we present the case of a 72-year-old patient with displacement of a pancreatic stent, placed following duodenocephalopancreatectomy for a neuroendocrine tumor of the head performed 6 years prior.
2Image findings
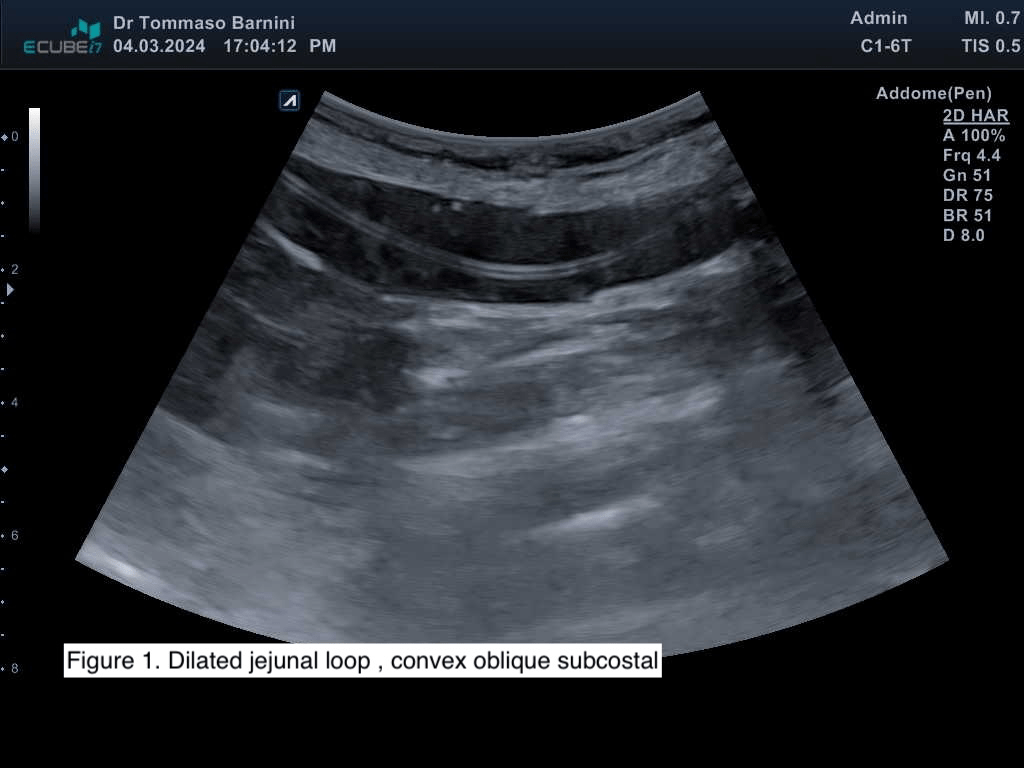
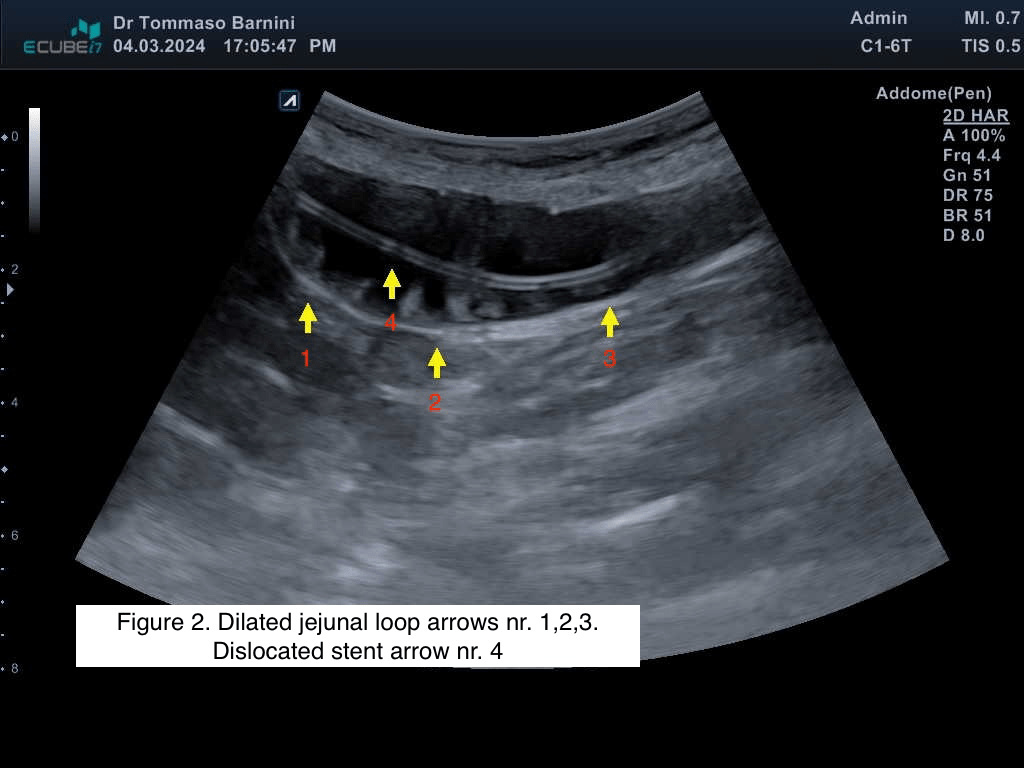
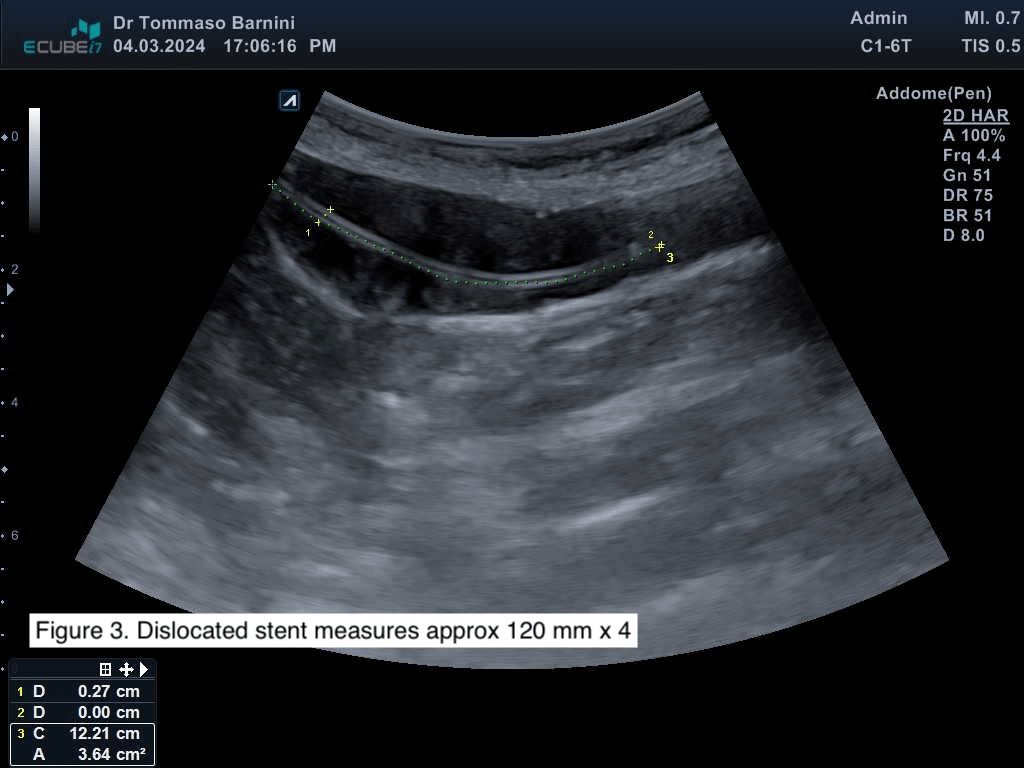
On ultrasound imaging performed with Alpinion eCube i7 using a linear probe of 5-12 MHz, no masses or signs of disease recurrence were found. At the site of pain, dilation of a jejunal loop (Figures 1,2) with the presence of a hyperechoic, linear image, approximately 120x4 mm in size (Figures 2,3), consistent with dislocated pancreatic stent, was observed. The patient was aware of the stent displacement, found in a previous abdominal CT scan. There were no findings of free abdominal air, free fluid, and regular peristalsis was present (Video 1).
3Diagnosis
Distal pancreaticojejunal anastomotic stent migration
4Discussion
THERAPY PLANNING:
The patient was treated with oral laxatives and scheduled for a follow-up visit in one week. Nevertheless, the patient was provided with a safety net, instructing her to contact the clinic in case of worsening pain or fever.
OUTCOME & PROGNOSIS:
The patient was subsequently seen one week later with resolution of abdominal pain, and the point-of-care ultrasound demonstrated reduction of jejunal distension and persistence of the stent.
The patient was treated with oral laxatives and scheduled for a follow-up visit in one week. Nevertheless, the patient was provided with a safety net, instructing her to contact the clinic in case of worsening pain or fever.
OUTCOME & PROGNOSIS:
The patient was subsequently seen one week later with resolution of abdominal pain, and the point-of-care ultrasound demonstrated reduction of jejunal distension and persistence of the stent.
5Teaching Points
Ultrasound of the small intestine can be easily utilized even in the primary care setting to identify causes of constipation or suspected intestinal perforation.
Identification of indirect signs of abdominal perforation on ultrasound (free air - intestinal a lines, free fluid, reduced or absent peristalsis)
Identification of indirect signs of abdominal perforation on ultrasound (free air - intestinal a lines, free fluid, reduced or absent peristalsis)
6References
1.) Re GL, La MantiaF, PiconeD, et al. Small bowel perforations: what the radiologist needs to know. Semin Ultrasound. 2016; 37(1): 23-30.
2.) Ortega PM, Zozaya-Larequi G, Arredondo J, et al. Distal migration of a transanastomotic pancreatic stent resulting in bowel perforation 19 years after pancreatoduodenectomy: report of a case. Surg Today 2015; 45(3): 374-377.
3.) Bao Li, ChenZ-T, Huang J-C,et al. Small bowel perforation caused by pancreaticojejunal anastomotic stent migration after pancreaticoduodenectomy: A case report. Medicine 2020; 99(30): e21120.
2.) Ortega PM, Zozaya-Larequi G, Arredondo J, et al. Distal migration of a transanastomotic pancreatic stent resulting in bowel perforation 19 years after pancreatoduodenectomy: report of a case. Surg Today 2015; 45(3): 374-377.
3.) Bao Li, ChenZ-T, Huang J-C,et al. Small bowel perforation caused by pancreaticojejunal anastomotic stent migration after pancreaticoduodenectomy: A case report. Medicine 2020; 99(30): e21120.