- European Federation of Societies for Ultrasound in Medicine and Biology ~ Educating all for competence to practice ultrasound safely

Cystic Liver Metastases of a Neuroendocrine Pancreatic Tumor [Mar 2016]
March 10, 2016CEUS Non Liver
April 28, 2016Bouveret syndrome
Medizinische Klinik 2
Caritas-Krankenhaus
Uhlandstr. 7
97980 Bad Mergentheim
Tel:+49 7931 58 2201
Email: christoph.dietrich@ckbm.de
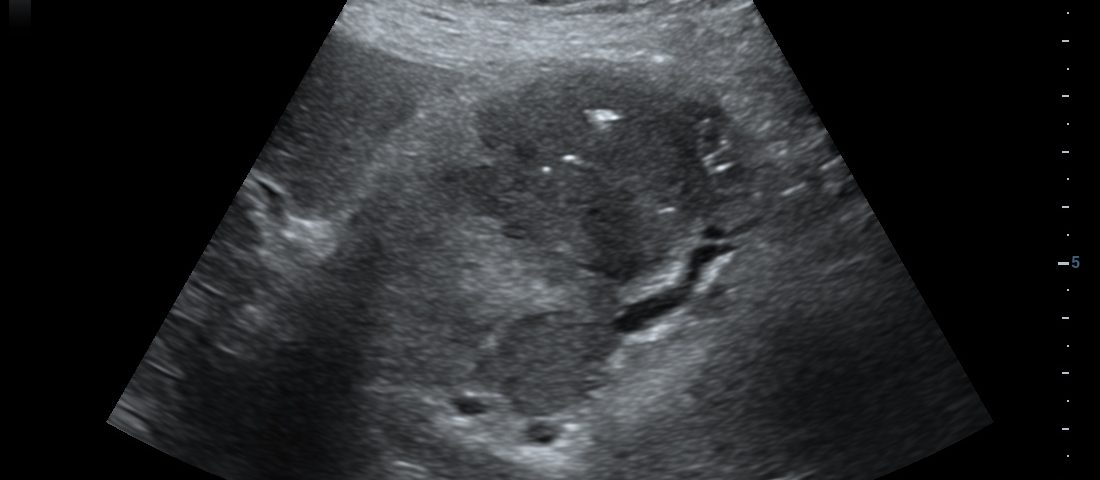
We report on an elderly 76 year old female presenting with an episode of haematemesis in the context of one week of nausea and vomiting for one week, unresponsive to PPI. There was no history of epigastric pain but known cholelithiasis. B-mode imaging revealed large (> 25 mm) presumably bile stones in the liver hilum (duodenal bulb) surrounded by a mass lesion (> 10 x 50 mm). Retention of gastric contents was documented. Localised aerobilia was seen subdiaphragmatically. The B-mode ultrasound findings were suggestive of an inflammatory or neoplastic mass in the liver hilum. Contrast enhanced ultrasound deomonstrated arterial enhancement of the whole mass lesion, excluding an abscess. Enhancement and portal venous wash out was indicative of a malignant neoplasia. Endoscopy revealed the suspected bile stones within the bulb of duodenum but intubation into the distal duodenum was not possible. Endoscopic ultrasound confirmed the findings and revealed the stiff nature of the mass lesion tissue. Biopsies demonstrated underlying gallbladder malignancy. Surgery was declined. Her treatment was conservative, with the option of a stone extraction and stent placement offered.
The typical Bouveret syndrome is characterized by a proximal small bowel gallstone ileus with gastric outlet obstruction, due to impaction of large gallstone(s) within the duodenal bulb or proximal duodenum [(4)]. Sometimes the pylorus or antrum can be affected also. Bilioenteric fistula is often caused secondary to previous cholecystitis [(5)]. Owing to its uncommon and unpredictable presentation, Bouveret's syndrome can pose a diagnostic and therapeutic challenge for clinicians [(6)].
Ultrasound, computed tomography and endoscopy have been diagnostic in our case. CT did not appreciate the underlying pathology (gallbladder carcinoma), whereas contrast enhanced ultrasound revealed typical features.
Risk Factors for Bouveret's syndrome include age over 70 years, female gender, gallstones larger than 2.5 cm and post surgical altered GI anatomy [(7)]. Common symptoms include vomiting (87 %), abdominal pain (71 %), haematemesis (15 %), recent weight loss (14 %) and anorexia (13 %) [(8)]. Bouveret's syndrome results in complications such as duodenal perforation, hematemesis (Mallory-Weiss tear), distal oesophageal rupture (Boerhaave's syndrome) and gastric bezoar [(8)] amongst others. In patients with gastric outlet obstruction primary or secondary malignancy of the duodenum and surrounding structures needs to be considered, including ductal adenocarcinoma of the pancreas, cholangiocarcinoma, lymphoma, carcinoid, metastases and, as shown in our patient, advanced gallbladder carcinoma.
Abdominal X-ray can show the so-called “Rigler's triad” of pneumobilia, small bowel obstruction and gall stones, in 30 – 35 % cases [(9)]. Abdominal ultrasound is most helpful in the hands of experienced examiners, but review of the literature revealed positive diagnosis in 60 % of cases. The sonographic findings include a fluid filled distended stomach, features suggestive of cholecystitis, ectopic gall-stones and pneumobilia. Abdomen CT with contrast has a published sensitivity of 93 %, specificity of 100 % and diagnostic accuracy of 99 % [(10)] but missed the neoplastic nature of the disease in our case. MRCP can differentiate between gall stones and surrounding bile (CT cannot in 15 – 25 % cases) [(11)]. Endoscopy is both diagnostic and therapeutic. The common findings are gall stone causing obstruction (69 %), gastric outlet obstruction without cause identified (31 %) whilst the fistula is visualized in only 13 % of cases [(8)].
Treatment options include endoscopic, open surgical and laparoscopic approaches. Endoscopic techniques include endoscopic extraction, endoscopic laser lithotripsy, extracorporeal shockwave lithotripsy and intracorporeal electrohydraulic lithotripsy [(4)]. The first successful endoscopic extraction was described in 1985 by Bedogni et al [(12)]. Endoscopic management often requires the use of different sized and shaped snares, grasping forceps, retrieval baskets and nets, biliary balloons, and sometimes even a side-viewing endoscope. Hence it can be technically challenging, time-consuming and the success rates reported in case series have been less than 10 % [(13)]. Endoscopy could be considered as the first treatment in the elderly patient with significant comorbidity, combined with mechanical, electrohydraulic, or laser lithotripsy. Surgical options include simple stone extraction or definitive fistula closure in either 1 or 2 stages. The former is associated with a lower mortality rate and spontaneous fistula closure is reported, whilst the latter is thought to decrease the risk of subsequent complications [(14)]. Indications for open surgery are stone size greater than 2.5 cm, residual stones in GB, multiple stones in intestinal lumen, sepsis, perforation, stricture and failure of endoscopic approach [(13)]. Treatment choice should consider advanced age, comorbidity [(15)], underlying etiology and available equipment [(16)].
2. Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, Klauser AS, et al. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: Clinical applications. Ultraschall Med 2013;34:238-253.
3. Bouveret L. Stenose du pylore adherent a la vesicule. Rev Medicale 1896;16:1-16.
4. Kalwaniya DS, Arya SV, Guha S, Kuppuswamy M, Chaggar JG, Ralte L, Chejera R, et al. A rare presentation of gastric outlet obstruction (GOO) - The Bouveret's syndrome. Ann Med Surg (Lond) 2015;16:67-71.
5. Newton RC, Loizides S, Penney N, Singh KK. Laparoscopic management of Bouveret syndrome. BMJ Case Rep 2015;2015.
6. Sağlam F, Sivrikoz E, Alemdar A, Kamalı S, Arslan U, Güven H. Bouveret syndrome: A fatal diagnostic dilemma of gastric outlet obstruction. Ulus Travma Acil Cerrahi Derg 2015;21:157-159.
7. Koulaouzidis A, Moschos J. Bouveret's syndrome Narrative review. Ann Hepatol 2007;6:89-91.
8. Cappell MS, Davis M. Characterization of Bouveret's syndrome: a comprehensive review of 128 cases. Am J Gastroenterol 2006;101:2139-2146.
9. Masannat YA, Caplin S, Brown T. A rare complication of a common disease. Bouveret's syndrome: a case report. World J Gastroenterol 2006;12:2620-2621.
10. Yu CY, Lin CC, Shyu RY, Hsieh CB, Wu HS, Tyan YS, Hwang JI, et al. Value of CT in the diagnosis and management of gallstone ileus. World J Gastroenterol 2005;11:2142-2147.
11. Trubek S, Bhama JK, Lamki N. Radiological findings in bouveret's syndrome. Emerg Radiol 2001;8:335-337.
12. Bedogni G, Contini S, Meinero M, Pedrazzoli C, Piccinini GC. Pyloroduodenal obstruction due to a biliary stone (Bouveret's syndrome) managed by endoscopic extraction. Gastrointest Endosc 1985;31:36-38.
13. Lowe AS, Stephenson S, Kay CL, May J. Duodenal obstruction by gallstones (Bouveret's syndrome): a review of the literature. Endoscopy 2005;37:82-87.
14. Halabi WJ, Kang CY, Ketana N, Lafaro KJ, Nguyen VQ, Stamos MJ, Imagawa DK, et al. Surgery for gallstone ileus: a nationwide comparison of trends and outcomes. Ann Surg 2014;259:329-335.
15. Doycheva I, Limaye A, Suman A, Forsmark CE, Sultan S. Bouveret's syndrome: case report and review of the literature. Gastroenterology Res Pract 2009;2009:4.
16. Baharith H, Khan K. Bouveret syndrome: when there are no options. Can J Gastroenterol Hepatol 2015;29:17-18.
Conventional B-mode ultrasound revealed a mass lesion in the gallbladder region (a) and air bubbles within the liver (aerobilia) (b). Contrast enhanced ultrasound showed arterial enhancement as a sign of neoplasia (c). Endoscopy revealed a gallstone in the duodenal bulb (d). Elastography showed stiff tissue (blue) supportive of neoplasia (e). Details of elastography are explained in the EFSUMB guidelines on elastography [(1, 2)].


![Bouveret syndrome</br> [Apr 2016]](https://efsumb.org/wp-content/uploads/2020/11/cotm_april2016-fig1a.jpg)
![Bouveret syndrome</br> [Apr 2016]](https://efsumb.org/wp-content/uploads/2020/11/cotm_april2016-fig1b.jpg)
![Bouveret syndrome</br> [Apr 2016]](https://efsumb.org/wp-content/uploads/2020/11/cotm_april2016-fig1c.jpg)
![Bouveret syndrome</br> [Apr 2016]](https://efsumb.org/wp-content/uploads/2020/11/cotm_april2016-fig1d.jpg)
![Bouveret syndrome</br> [Apr 2016]](https://efsumb.org/wp-content/uploads/2020/11/cotm_april2016-fig1e.jpg)
