
Trans-Vaginal Scanning – Safety Aspects
December 29, 2020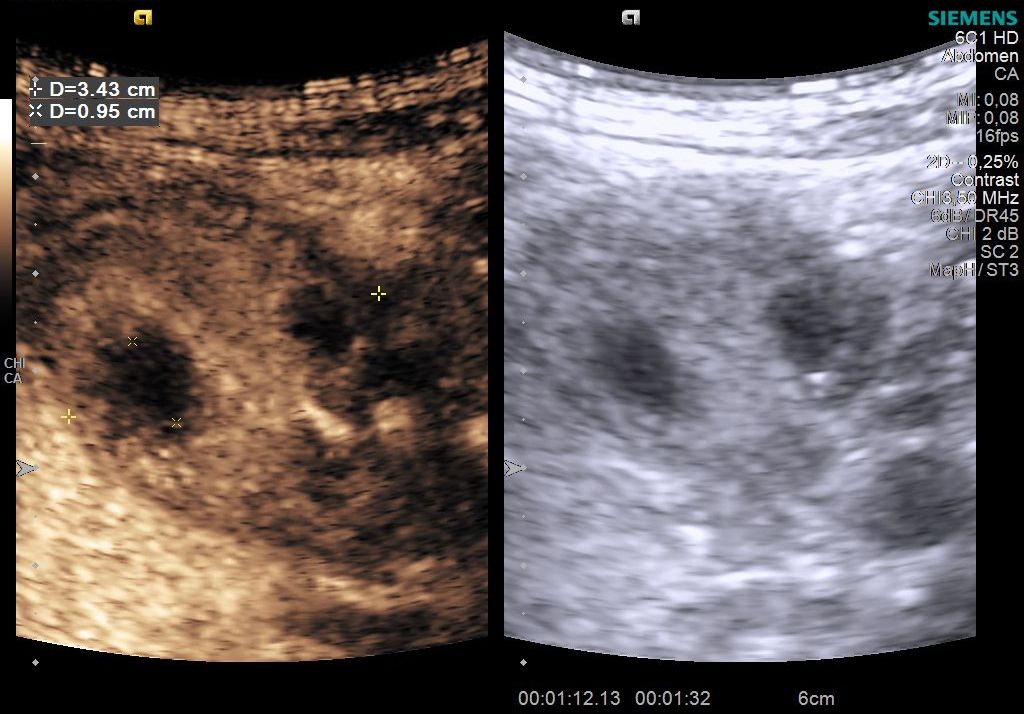
Student Image Challenge 79
January 11, 2021Bowel ultrasound findings in SARS-CoV-2 Pneumonia patients with gastrointestinal symptoms
AUTHORS
Carla Serra, Valentina Cossiga
Interventional and Diagnostic Ultrasound Unit, Dept of Organ Failure and Transplantation, S. Orsola University Hospital, Bologna, Italy.
Carla Serra, Valentina Cossiga
Interventional and Diagnostic Ultrasound Unit, Dept of Organ Failure and Transplantation, S. Orsola University Hospital, Bologna, Italy.
1Clinical history
Two male patients, 41 and 47 years old, with COVID-19 interstitial pneumonia were hospitalized due to acute respiratory failure and were treated with non-invasive ventilation.
Both patients had symptoms of asthenia, fever, myalgia and abdominal pain. One also had diarrhoea before hospitalization and elevation of liver transaminases. The patients had no relevant comorbidities. At clinical examination, patients showed mild pain on deep palpation in the lower right quadrant of the abdomen and valid intestinal peristalsis normal bowel sounds on auscultation
Both patients had symptoms of asthenia, fever, myalgia and abdominal pain. One also had diarrhoea before hospitalization and elevation of liver transaminases. The patients had no relevant comorbidities. At clinical examination, patients showed mild pain on deep palpation in the lower right quadrant of the abdomen and valid intestinal peristalsis normal bowel sounds on auscultation
2Image Findings
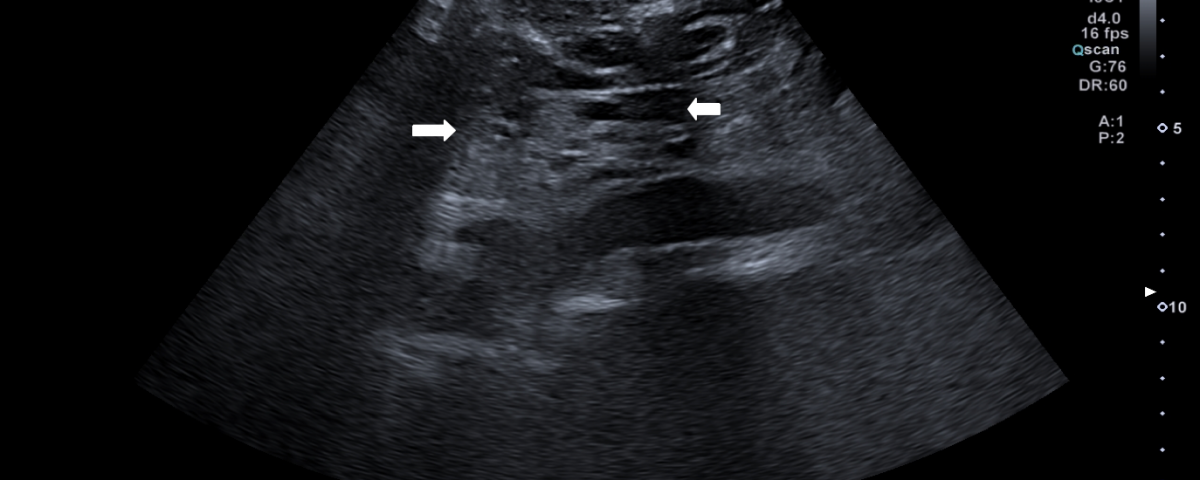
For persistent abdominal pain, we performed bowel ultrasound that showed, in both patients, dilated fluid-filled bowel loops with mildly thickened wall (3-4 mm), in different quadrants of the abdomen (Figure 1). Moreover, the mesenteric root appeared thickened and hyperechoic, with hypo-echogenicity of the adjacent retroperitoneal and meso-colonic fat, with a typical “mass effect” , suggestive of a mesenteritis. The bowel loops and the mesentery root however, did not show increased vascular flow with Colour Doppler and there was no free fluid in the abdomen (Figures 2 & 3; Video 1).
3Discussion
The gastrointestinal tract may be a potential transmission route and target organ of SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2), also known as COVID-19 infection. In early reports, 2–10% of patients with COVID-19 had gastrointestinal (GI) symptoms such as diarrhoea, nausea, vomiting and anorexia [1-5].
In 11.6% of cases patients presenting with GI symptoms at the onset of illness, 49.5% of cases exhibited GI symptoms during hospitalisation, which could be aggravated by various drugs, including antibiotics [6]. Moreover, recent studies reported that some patients (about 12%) can present only with GI symptoms [6,7]. Given that SARS-CoV-2 RNA has been detected in patient’s stool [8], it is possible that SARS-CoV-2 could also be transmitted via the faecal–oral route, causing viral GI infection. There is evidence demonstrating that ACE-2 (angiotensin-converting enzyme 2) is one of the host receptors for cell entry for SARS-CoV-2. Gene expression levels of ACE-2 differ across human body, with the highest expression in the small intestine and terminal ileum [9]. These findings could explain how SARS-CoV-2 infect intestinal cells, causing different types of damage to the GI tract. To confirm this, patients with more severe GI symptoms, such as bleeding, have been subjected to endoscopy, revealing the presence of erosions and ulcers in different sites of the GI tract, especially within the oesophagus [6].
At histological evaluation of biopsy samples, collected during endoscopy, SARS-CoV-2 RNA was detected also in the tissue. This evidence demonstrated that, while the presence of SARS-CoV-2 in faeces does not necessarily involve GI symptoms, the presence of SARS-CoV-2 in GI tissue generally indicates more severe scenarios [6].
Transabdominal gastrointestinal ultrasound (GIUS) is the imaging method of choice for many indications and allows a unique combination of focused medical history, clinical examination and imaging to make a diagnosis. GIUS is also an important method to examine the bowel non-invasively in acute and chronic disease [10,11] including extra-intestinal features such as the splanchnic vessels, mesentery, omentum and lymph nodes [10]. Moreover, ultrasound is a non-invasive imaging method that can be performed at the bedside which is essential in critically ill patients, such as COVID-19 patients, without the necessity of bringing additional staff and equipment to contaminated areas or moving infected patients into clean areas. It also can be repeated frequently to monitor progression or resolution of disease, without contraindications [12] but has the limitation of being operator dependent. For these reasons, GIUS could be used in COVID-19 patients with GI symptoms to assess the severity of disease and monitoring.
In these two patients, bowel ultrasound showed findings similar to patients with a mesenteritis, suggesting that COVID-19 could also cause inflammation to mesentery with consequent abdominal pain. Further research of patients with COVID-19 and GI symptoms are suggested to confirm these observations and to evaluate the clinical impact of bowel US in this setting.
In 11.6% of cases patients presenting with GI symptoms at the onset of illness, 49.5% of cases exhibited GI symptoms during hospitalisation, which could be aggravated by various drugs, including antibiotics [6]. Moreover, recent studies reported that some patients (about 12%) can present only with GI symptoms [6,7]. Given that SARS-CoV-2 RNA has been detected in patient’s stool [8], it is possible that SARS-CoV-2 could also be transmitted via the faecal–oral route, causing viral GI infection. There is evidence demonstrating that ACE-2 (angiotensin-converting enzyme 2) is one of the host receptors for cell entry for SARS-CoV-2. Gene expression levels of ACE-2 differ across human body, with the highest expression in the small intestine and terminal ileum [9]. These findings could explain how SARS-CoV-2 infect intestinal cells, causing different types of damage to the GI tract. To confirm this, patients with more severe GI symptoms, such as bleeding, have been subjected to endoscopy, revealing the presence of erosions and ulcers in different sites of the GI tract, especially within the oesophagus [6].
At histological evaluation of biopsy samples, collected during endoscopy, SARS-CoV-2 RNA was detected also in the tissue. This evidence demonstrated that, while the presence of SARS-CoV-2 in faeces does not necessarily involve GI symptoms, the presence of SARS-CoV-2 in GI tissue generally indicates more severe scenarios [6].
Transabdominal gastrointestinal ultrasound (GIUS) is the imaging method of choice for many indications and allows a unique combination of focused medical history, clinical examination and imaging to make a diagnosis. GIUS is also an important method to examine the bowel non-invasively in acute and chronic disease [10,11] including extra-intestinal features such as the splanchnic vessels, mesentery, omentum and lymph nodes [10]. Moreover, ultrasound is a non-invasive imaging method that can be performed at the bedside which is essential in critically ill patients, such as COVID-19 patients, without the necessity of bringing additional staff and equipment to contaminated areas or moving infected patients into clean areas. It also can be repeated frequently to monitor progression or resolution of disease, without contraindications [12] but has the limitation of being operator dependent. For these reasons, GIUS could be used in COVID-19 patients with GI symptoms to assess the severity of disease and monitoring.
In these two patients, bowel ultrasound showed findings similar to patients with a mesenteritis, suggesting that COVID-19 could also cause inflammation to mesentery with consequent abdominal pain. Further research of patients with COVID-19 and GI symptoms are suggested to confirm these observations and to evaluate the clinical impact of bowel US in this setting.
4Teaching Point
It would be useful to assess the bowel with ultrasound in COVID-19 patients with abdominal pain.
5References
1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet 2020; 395:497–506.
2. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. The Lancet 2020; 395:507–13.
3. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel Coronavirus–Infected pneumonia in Wuhan, China. JAMA 2020; 323:1061.
4. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382:727–33.
5. Guan W-jie, Ni Z-yi, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382(18):1708-1720.
6. Lin L, Jiang X, Zhang Z, et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut 2020; 69: 997-1001
7. Song Y, Liu P, Shi XL, et al. SARS-CoV-2 induced diarrhoea as onset symptom in patient with COVID-19. Gut 2020; 69:1143–4.
8. Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020; 382:929–36.
9. Pirola CJ, Sookoian S. COVID-19 and ACE2 in the liver and gastrointestinal tract: putative biological explanations of sexual dimorphism. Gastroenterology 2020; doi: 10.1053/j.gastro.2020.04.050.
10. Maconi G, Nylund K, Ripolles T, et al. EFSUMB Recommendations and Clinical Guidelines for Intestinal Ultrasound (GIUS) in Inflammatory Bowel Diseases. Ultraschall Med 2018; 39:304-317.
11. Hollerwerger A, Maconi G, Ripolles T, et al. Gastrointestinal Ultrasound (GIUS) in Intestinal Emergencies - An EFSUMB Position Paper. Ultraschall Med 2020; doi: 10.1055/a-1147-1295.
12. Shaw JA, Louw EH, Koelegeneberg CFN. Lung Ultrasound in COVID-19: Not Novel, but Necessary. Respiration 2020. doi: 10.1159/000509763.
2. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. The Lancet 2020; 395:507–13.
3. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel Coronavirus–Infected pneumonia in Wuhan, China. JAMA 2020; 323:1061.
4. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382:727–33.
5. Guan W-jie, Ni Z-yi, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382(18):1708-1720.
6. Lin L, Jiang X, Zhang Z, et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut 2020; 69: 997-1001
7. Song Y, Liu P, Shi XL, et al. SARS-CoV-2 induced diarrhoea as onset symptom in patient with COVID-19. Gut 2020; 69:1143–4.
8. Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020; 382:929–36.
9. Pirola CJ, Sookoian S. COVID-19 and ACE2 in the liver and gastrointestinal tract: putative biological explanations of sexual dimorphism. Gastroenterology 2020; doi: 10.1053/j.gastro.2020.04.050.
10. Maconi G, Nylund K, Ripolles T, et al. EFSUMB Recommendations and Clinical Guidelines for Intestinal Ultrasound (GIUS) in Inflammatory Bowel Diseases. Ultraschall Med 2018; 39:304-317.
11. Hollerwerger A, Maconi G, Ripolles T, et al. Gastrointestinal Ultrasound (GIUS) in Intestinal Emergencies - An EFSUMB Position Paper. Ultraschall Med 2020; doi: 10.1055/a-1147-1295.
12. Shaw JA, Louw EH, Koelegeneberg CFN. Lung Ultrasound in COVID-19: Not Novel, but Necessary. Respiration 2020. doi: 10.1159/000509763.


![Bowel ultrasound findings in SARS-CoV-2 Pneumonia patients with gastrointestinal symptoms </br> [Jan 2021]](https://efsumb.org/wp-content/uploads/2020/12/Screen-Shot-2020-12-30-at-08.50.27.png)
![Bowel ultrasound findings in SARS-CoV-2 Pneumonia patients with gastrointestinal symptoms </br> [Jan 2021]](https://efsumb.org/wp-content/uploads/2020/12/Screen-Shot-2020-12-30-at-08.51.48.png)
![Bowel ultrasound findings in SARS-CoV-2 Pneumonia patients with gastrointestinal symptoms </br> [Jan 2021]](https://efsumb.org/wp-content/uploads/2020/12/Screen-Shot-2020-12-30-at-08.52.53.png)
