Pseudoaneurysm, a rare complication after liver abscess drainage [Mar 2018]
March 12, 2018Contrast Enhanced Ultrasound (CEUS)
May 9, 2018Cystic lesions of the neck: an important reminder to consider malignant pathology in adult patients
1. Department of Otorhinolaryngology, Imperial College Healthcare NHS Trust, London, UK.
2. Department of Radiology, Imperial College Healthcare NHS Trust, London, UK.
The diagnostic challenge in the case of a 28-year-old male with nodal metastases from papillary thyroid cancer (PTC) is discussed. The patient presented with a right-sided neck lump which appeared two years previously and had become increasingly painful.
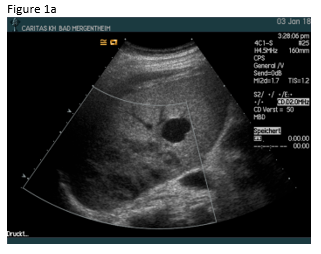
Initial computed tomography (Figure 1) demonstrated multiple right-sided thin walled cystic lesions within the upper to lower jugular chain and posterior triangle (levels II-V) forming a multi-loculated cystic lesion measuring approximately 10cm in maximal dimensions. Assessment with ultrasound (Figure 2a) revealed a multi-loculated cystic mass with thin walls and no intra-lesional flow, extending along the posterior margin of the right sternocleidomastoid muscle, posterolateral to the right internal jugular vein. The thyroid gland (Figure 2b) and major salivary glands appeared unremarkable. Ultrasound-guided fine needle aspiration cytology (FNAC) proved inconclusive.
Findings were thought to be consistent with a slow-flow lymphatic malformation and injection sclerotherapy was performed. The lump however persisted, and seven months later a repeat MRI scan confirmed no clinical response. The patient subsequently underwent selective right neck dissection (levels II-V) the histology of which identified PTC metastases. The diagnosis of microscopic PTC was confirmed on histopathological analysis following total thyroidectomy.
The presence of a thickened wall and/or mural nodularity in a cystic mass on any imaging modality should raise the possibility of malignancy, although this cannot be relied upon, as metastatic nodes may be thin walled and entirely cystic (2). Therefore, any cystic neck mass in the lateral neck in an adult should undergo US-guided FNAC for further assessment.
Ultrasound proves useful in the initial work-up in the assessment for neck masses. PTC nodal metastases have a spectrum of appearances, and can be either solid or cystic. The latter appearance is a diagnostic challenge as they may be misinterpreted as benign cystic masses, potentially resulting in diagnostic delay and deferred radical treatment. A study by Wunderbaldinger and colleagues correlated sonographic imaging findings with pathologically proven PTC nodal metastases (3). In a cohort of 97 patients, 41% were found to have cystic node metastases. In fact, as in our case presentation, in 8% of patients the cystic lymph node metastases were initially mistaken for benign cystic lesions.
This case emphasises the need to always consider malignant lesions, including metastases, in adults presenting with cystic lesions of the neck.
2. Yehuda M, Schechter ME, Abu-Ghanem N, Golan G, Horowitz G, Fliss DM, et al. The incidence of malignancy in clinically benign cystic lesions of the lateral neck: our experience and proposed diagnostic algorithm. Eur Arch Oto-Rhino-Laryngology [Internet]. 2018 Mar 27 [cited 2018 Feb 18];275(3):767–73.
3. Wunderbaldinger P, Harisinghani MG, Hahn PF, Daniels GH, Turetschek K, Simeone J, et al. Cystic Lymph Node Metastases in Papillary Thyroid Carcinoma. Am J Roentgenol [Internet]. 2002 Mar 23 [cited 2018 Mar 31];178(3):693–7.
Figure 2: Ultrasound image (A) demonstrating a thin-walled multi-loculated lesion which correlates with the CT findings. Ultrasound of the thyroid (B) does not demonstrate any identifiable lesion within.
Figure 3: Fluoroscopic image of percutaneous injection sclerotherapy of the right-sided cystic lesion.
Figure 4: T2-fat saturated MRI study of the neck which demonstrates persistence of the right sided cystic lesion despite injection sclerotherapy. There is subtle low signal at the base of the lesion, which was initially thought to be debris. In retrospect, this is likely to reflect mural nodularity of one of the cysts.



![Cystic lesions of the neck: an important reminder to consider malignant pathology in adult patients</br> [Apr 2018]](https://efsumb.org/wp-content/uploads/2020/11/2018apr-Figure-1.jpg)
![Cystic lesions of the neck: an important reminder to consider malignant pathology in adult patients</br> [Apr 2018]](https://efsumb.org/wp-content/uploads/2020/11/2018apr-Figure-2.jpg)
![Cystic lesions of the neck: an important reminder to consider malignant pathology in adult patients</br> [Apr 2018]](https://efsumb.org/wp-content/uploads/2020/11/2018apr-FIgure-3.jpg)
![Cystic lesions of the neck: an important reminder to consider malignant pathology in adult patients</br> [Apr 2018]](https://efsumb.org/wp-content/uploads/2020/11/2018apr-Figure-4.jpg)
