- European Federation of Societies for Ultrasound in Medicine and Biology ~ Educating all for competence to practice ultrasound safely

Posterior Interosseous Nerve syndrome caused by a Radial Osteochondroma [Feb 2018]
February 12, 2018
Cystic lesions of the neck: an important reminder to consider malignant pathology in adult patients [Apr 2018]
April 12, 2018Pseudoaneurysm, a rare complication after liver abscess drainage
Correspondence: Prof. Dr. med. Christoph F. Dietrich
Medizinische Klinik 2, Caritas-Krankenhaus, Uhlandstr. 7
97980 Bad Mergentheim
Tel:+49 7931 58 2201. Email: christoph.dietrich@ckbm.de
Claudio Tana: Affiliation Internal Medicine and Subacute Care Unit, Medicine and Geriatric/Rehabilitation Department, University Hospital of Parma, Parma, Italy (ctana@ao.pr.it)
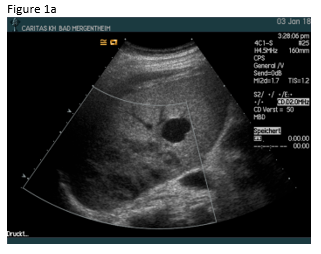
A 49 year old patient was admitted to the hospital for sepsis and shock of unknown origin. The patient presented with signs of sepsis and hemodynamic instability that justified an urgent approach including complex intensive care and intubation. Bedside ultrasound (US) found ascites and an abscess in the right liver lobe (9 cm) (Figure 1a). The patient was treated with broad-spectrum antibiotics and puncture and drainage of the abscess (Figures 1 a-c and 2 a-b). In addition, a biopsy was taken from the periphery of the lesion. A few days after the removal of the drainage the patient presented with a progressive elevation of liver enzymes. US revealed a cystic lesion measuring 30 mm that was proximal to the drained abscess (Figure 1a). Color Doppler Imaging (CDI) showed arterial flow inside the lesion, and contrast enhanced ultrasound (CEUS) showed early arterial enhancement and turbulent flow with a “to-and-fro” sign, suggestive of a pseudoaneurysm (Figure 1b). There was also a heterogeneously vascularized lesion with enhancing septae in the surrounding liver parenchyma (Figure 1c) . A few days later the patient presented with tachycardia and a drop of hemoglobin from 10 g/dl to 7 g/dl. US revealed spontaneous thrombosis of the pseudoaneurysm (Figure 1d) with intra - and perihepatic hemorrhage (Figure 1e).
In general, pseudoaneurysms may be congenital as result of a defective regression of the right primitive vitelline vein, or acquired such as after a trauma or disorders such as liver cirrhosis, HCC or pancreatitis. Iatrogenic pseudoaneurysms occur after hepatic interventions including abscess drainage, and therefore complicate the procedure with further symptoms [2,3].
Phlegmonous inflammation and abscess formations show variable and sometimes confusing US B-mode findings, which may change over time. The surrounding hypervascularitiy of abscesses may support the development of pseudoaneurysm after puncture and drainage in a few patients. On B-mode US pseudoaneurysms may appear like a cystic tumor, therefore CDI should be preferred as the primary screening technique for detection of vascular complications. The swirling colour pattern of the flow within the pseudoaneurysm that mimicks the "yin-yang" symbol (so called “to-and-fro” pattern) and the presence of high velocity are characteristic features of these lesions [(1-3)].
Contrast enhanced imaging techniques including CEUS and CT are used to confirm the sonographic findings or when the US evaluation is inconclusive [4-9]. CEUS has several advantages compared to CT, such as no radiation exposure, low cost and absence of nephrotoxicity [3].
The localization of the pseudoaneurysm can be intrahepatic or extrahepatic. Rupture of a pseudoaneurysm may have fatal consequences where bleeding from an extrahepatic pseudoaneurysm is often fatal with an estimated mortality up to 70%. The prognosis of an intrahepatic rupture of a pseudoaneurysm is better [10-15].
Emergent embolization with permanent embolic materials using superselective catheterization should be considered. Severe bleeding from extrahepatic pseudoaneurysms can be treated with occlusion of the hepatic artery by embolization before arterial reconstruction. Different surgical therapeutic options are available: simple ligation of the artery, aneurysm excision and vascular reconstruction.
However, the therapeutic choice should be evaluated in each individual case, depending on the size, aspect and location of the aneurysm, the clinical situation of the patient, and requires an accurate study of the collateral vascular supply [16-20]. The patient’s medical history and occasionally the physical examination (febrile temperature or signs of sepsis) are the most helpful in differentiating abscesses from necrotic metastases [(4-7)].
In conclusion, iatrogenic vascular complications are rare but typical complications after biopsy and drainage procedures should be considered in patients with unclear symptoms.
For further reading we refer to the EFSUMB INVUS guidelines (interventional ultrasound guidelines) [(8-20)] and comment papers [(21-24)]. See also cases of the month [http://www.efsumb-archive.org/asp/detail06.asp?ref=373&url=/case-month/cm-archive.asp?ref=1].
2. Braden B, Thalhammer A, Schwarz W, Dietrich CF. Bleeding complications from hepatic mucoidal aneurysmata: value of color duplex sonography after liver transplantation. Liver Transpl. 2002;8:636-638.
3. Tana C, Dietrich CF, Badea R, Chiorean L, Carrieri V, Schiavone C. Contrast-enhanced ultrasound in portal venous system aneurysms: a multi-center study. World J Gastroenterol 2014;20:18375-18383. 4. Gottschalk U, Ignee A, Dietrich CF. [Ultrasound guided interventions, part 1, diagnostic procedures]. Z.Gastroenterol. 2009;47:682-690.
5. Gottschalk U, Ignee A, Dietrich CF. [Ultrasound-guided interventions and description of the equipment]. Z.Gastroenterol. 2010;48:1305-1316.
6. Dietrich CF, Nuernberg D. Interventional ultrasound. A practical guide and atlas: Thieme, 2014.
7. Dietrich CF, Nuernberg D. Interventioneller Ultraschall. Lehrbuch und Atlas für die interventionelle Sonographie: Thieme Verlag, 2011.
8. Dietrich CF, Lorentzen T, Sidhu PS, Jenssen C, Gilja OH, Piscaglia F. An Introduction to the EFSUMB Guidelines on Interventional Ultrasound (INVUS). Ultraschall Med 2015;36:460-463.
9. Lorentzen T, Nolsoe CP, Ewertsen C, Nielsen MB, Leen E, Havre RF, Gritzmann N, et al. EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part I. General Aspects (long Version). Ultraschall Med 2015;36:E1-14.
10. Lorentzen T, Nolsoe CP, Ewertsen C, Nielsen MB, Leen E, Havre RF, Gritzmann N, et al. EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part I. General Aspects (Short Version). Ultraschall Med 2015;36:464-472.
11. Sidhu PS, Brabrand K, Cantisani V, Correas JM, Cui XW, D'Onofrio M, Essig M, et al. EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part II. Diagnostic Ultrasound-Guided Interventional Procedures (Long Version). Ultraschall Med 2015;36:E15-35.
12. Sidhu PS, Brabrand K, Cantisani V, Correas JM, Cui XW, D'Onofrio M, Essig M, et al. EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part II. Diagnostic Ultrasound-Guided Interventional Procedures (Short Version). Ultraschall Med 2015;36:566-580.
13. Dietrich CF, Lorentzen T, Appelbaum L, Buscarini E, Cantisani V, Correas JM, Cui XW, et al. EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part III - Abdominal Treatment Procedures (Long Version). Ultraschall Med 2016;37:E1-E32.
14. Dietrich CF, Lorentzen T, Appelbaum L, Buscarini E, Cantisani V, Correas JM, Cui XW, et al. EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part III - Abdominal Treatment Procedures (Short Version). Ultraschall Med 2016;37:27-45.
15. Jenssen C, Hocke M, Fusaroli P, Gilja OH, Buscarini E, Havre RF, Ignee A, et al. EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part IV - EUS-guided Interventions: General aspects and EUS-guided sampling (Long Version). Ultraschall Med 2016;37:E33-76.
16. Jenssen C, Hocke M, Fusaroli P, Gilja OH, Buscarini E, Havre RF, Ignee A, et al. EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part IV - EUS-guided interventions: General Aspects and EUS-guided Sampling (Short Version). Ultraschall Med 2016;37:157-169.
17. Fusaroli P, Jenssen C, Hocke M, Burmester E, Buscarini E, Havre RF, Ignee A, et al. EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part V. Ultraschall Med 2016;37:77-99.
18. Fusaroli P, Jenssen C, Hocke M, Burmester E, Buscarini E, Havre RF, Ignee A, et al. EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part V - EUS-Guided Therapeutic Interventions (short version). Ultraschall Med 2016;37:412-420.
19. Jenssen C, Brkljacic B, Hocke M, Ignee A, Piscaglia F, Radzina M, Sidhu PS, et al. EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part VI - Ultrasound-Guided Vascular Interventions. Ultraschall Med 2016;37:473-476.
20. Dietrich CF. EFSUMB guidelines 2015 on interventional ultrasound. Med Ultrason 2015;17:521-527.
21. Mohaupt MG, Arampatzis S, Atkinson N, Yi D, Cui XW, Ignee A, Dietrich CF. Comments and extensions to EFSUMB guidelines on renal interventional ultrasound (INVUS). Med Ultrason 2016;18:351-361.
22. Dietrich CF, Muller T, Bojunga J, Dong Y, Mauri G, Radzina M, Dighe M, et al. Statement and Recommendations on Interventional Ultrasound as a Thyroid Diagnostic and Treatment Procedure. Ultrasound Med Biol 2018;44:14-36.
23. Dietrich CF, Cui XW, Chiorean L, Appelbaum L, Leen E, Ignee A. Local ablative procedures of the liver. Z Gastroenterol 2015;53:579-590.
24. Dietrich CF, Chiorean L, Potthoff A, Ignee A, Cui X, Sparchez Z. Percutaneous sclerotherapy of liver and renal cysts, comments on the EFSUMB guidelines. Z Gastroenterol 2016;54:155-166.
Figure 2: Computed tomography (CT)showed abscess formation before drainage and perihepatic ascites (a). Twelve days after drainage removal a CT follow-up showed hyperenhancing intrahepatic lesion in proximity of the abscess, suggestive of a pseudoaneurysm (b). CT confirmed the spontaneous thrombosis of the pseudoaneurysm (c).


![Pseudoaneurysm, a rare complication after liver abscess drainage</br> [Mar 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_march2018_f1b.png)
![Pseudoaneurysm, a rare complication after liver abscess drainage</br> [Mar 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_march2018_f1c.png)
![Pseudoaneurysm, a rare complication after liver abscess drainage</br> [Mar 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_march2018_f1d.png)
![Pseudoaneurysm, a rare complication after liver abscess drainage</br> [Mar 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_march2018_f1e.png)
![Pseudoaneurysm, a rare complication after liver abscess drainage</br> [Mar 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_march2018_f2a.png)
![Pseudoaneurysm, a rare complication after liver abscess drainage</br> [Mar 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_march2018_f2b.png)
![Pseudoaneurysm, a rare complication after liver abscess drainage</br> [Mar 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_march2018_f2c.png)
