- European Federation of Societies for Ultrasound in Medicine and Biology ~ Educating all for competence to practice ultrasound safely
Intracavity CEUS
January 19, 2018
Pseudoaneurysm, a rare complication after liver abscess drainage [Mar 2018]
March 12, 2018Posterior Interosseous Nerve syndrome caused by a Radial Osteochondroma
1 Radiology Department Clínica Meds, Santiago de Chile, Chile
2 Orthopedic Surgery Clínica Meds, Santiago de Chile, Chile
3 Clinic Hospital, Salamanca University, Spain
4 Sport Sciences Faculty, Castilla La Mancha University, Toledo, Spain
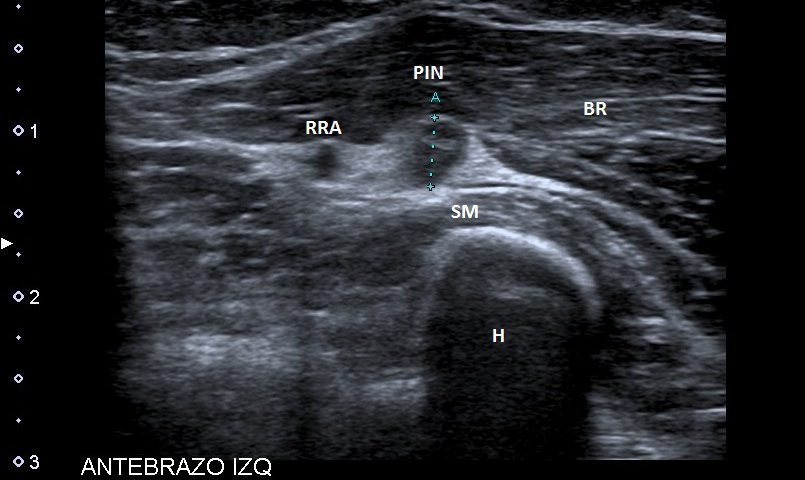
A 51-years-old healthy female, with no history of upper limb injuries, complained of an anterior and proximal left forearm tenderness associated with weakness of the extensor muscles of the forearm. An ultrasound scan was performed and demonstrated a thickened and hypoechoic posterior interosseous nerve (PIN) at the arcade of Frohse, with hypervascularization of the perineurium. In its deeper aspect, there was a subtle irregularity of the radial metaphysis (Fig1,2). The plain film showed a sessile irregularity of the anterior region of the metaphysis (Fig 3). Unenhanced MRI and CT scan were also performed. The CT scan showed the irregularity of the radius (Fig 4) and in the MRI (Fig 5), it was reported as an osteochondroma like metaphyseal lesion of the radius. Initial treatment included a corticosteroid injection around the PIN, but without decrease of symptomatology. The orthopedic surgeon then proceeded with an osteochondroma resection to release the PIN. The upper limb surgical team performed the surgery (Fig 6), and they found a thickened, hyperaemic PIN, adjacent to the osteochondroma (Fig 6,7). They resected the osteochondroma and debrided the PIN (Fig 8). The patient recovered full muscular strength and the tenderness progressively disappeared.
This case report illustrates that evaluation of the PIN, Arcade of Frohse, and radial recurrent artery are very dificult with standard elbow MRI, because small structures (diameters below 5 mm) are beyond the resolution of MRI typically using fields of view (FOV) of 12,0 x 18,6 cm and slice thickness of 3 mm.
With these parameters, obtaining a well defined image of a small structure is almost impossible. However, high frequency ultrasound scans allow high resolution imaging and assessment of these small structures. Furthermore, Power and color Doppler is also a useful adjunct to evaluate the perineural vascularisation.
PIN syndrome can have an extrinsic or intrinsic origin, with extrinsic compressions being the likeliest cause. In addition, the arcade of Frohse is the most common site where the nerve could be entraped. Many other causes of PIN syndrome have been described. A very unusual cause as described in this case, where there was compression from proliferative bone arising from the radius.
This case report demonstrates how useful state of the art ultrasound techniques are especially for evaluating subcentimetre structures, such as peripheral nerves when compared with other cross-sectional modalities.
- 1. You dong Kim et al.Ultrasonographic findings of posterior interosseous nerve syndrome. Ultrasonography 2017; 36(4): 363-369. .
- 2. Martinoli C, et al. Sonography of entrapment neuropathies in the upper limb (wrist excluded). J Clin Ultrasound. 2004 Nov-Dec;32(9):438-50.
- 3. Theodore T. et al. Nerve Entrapment Syndromes of the Elbow, Forearm, and Wrist. American Journal of Roentgenology. 2010;195: 585-594.
- 4. Regal R et al. Must the neuropathy compressive of posterior interoseal nerve at the elbow level (arcade of frohse syndrome) be included in the occupational diseases list? Med. segur. trab. vol.56 no.220 Madrid jul./sep. 2010
Fig 2: Ultrasound long axis view of the AF (Arcade of Frohse), showing a swelled PIN and its anatomical relationship with the radius osteochondroma (arrow). SM (Supinator Muscle), BR (Brachioradialis muscle) and R (Radius metaphysis).
Fig 3: Lateral elbow plain film, showing subtle irregularity of the anterior aspect of the radial metaphysis (circle).
Fig 4: Axial and sagital CT scan views, showing the osteochondroma (circle).
Fig 5: Axial PD and T1 weighted images, showing the relationship between the osteochondroma (arrow) and PIN (circle). Poor visualization of PIN and almost no presence of soft tissue oedema on the PD weighted sequence.
Fig 6: The PIN is exposed at the arcade of Frohse (AF) level, adjacent to the radial osteochondroma (OTC).
Fig 7: Dissection of the supinator (deep head), to expose the osteochondroma (arrow)
Fig 8: Radius (R) after resection of the osteochondroma. The radial recurrent artery is identified next to the PIN at the arcade of Frohse,.


![Posterior Interosseous Nerve syndrome caused by a Radial Osteochondroma</br> [Feb 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm018_feb-Fig.-1.jpg)
![Posterior Interosseous Nerve syndrome caused by a Radial Osteochondroma</br> [Feb 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm018_feb-Fig.-2.jpg)
![Posterior Interosseous Nerve syndrome caused by a Radial Osteochondroma</br> [Feb 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm018_feb-Fig.-3.jpg)
![Posterior Interosseous Nerve syndrome caused by a Radial Osteochondroma</br> [Feb 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm018_feb-Fig.-4.jpg)
![Posterior Interosseous Nerve syndrome caused by a Radial Osteochondroma</br> [Feb 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm018_feb-Fig.-5.jpg)
![Posterior Interosseous Nerve syndrome caused by a Radial Osteochondroma</br> [Feb 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm018_feb-Fig.-6.jpg)
![Posterior Interosseous Nerve syndrome caused by a Radial Osteochondroma</br> [Feb 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm018_feb-Fig.-7.jpg)
![Posterior Interosseous Nerve syndrome caused by a Radial Osteochondroma</br> [Feb 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm018_feb-Fig.-8.jpg)
