- European Federation of Societies for Ultrasound in Medicine and Biology ~ Educating all for competence to practice ultrasound safely

Thermal & Mechanical Indices – An Explanation [Update 2022]
March 15, 2022
Gas in the portal system in a patient with Crohn’s disease [Apr 2022]
May 13, 2022Direct proof of hepatic hydrothorax by intracavitary contrast-enhanced ultrasound
Christian Jenssen 1,2,
Christine Siebert 1
1 Krankenhaus Märkisch Oderland, Strausberg/ Wriezen, Germany
2 Brandenburg Institute for Clinical Ultrasound, Neuruppin, Germany
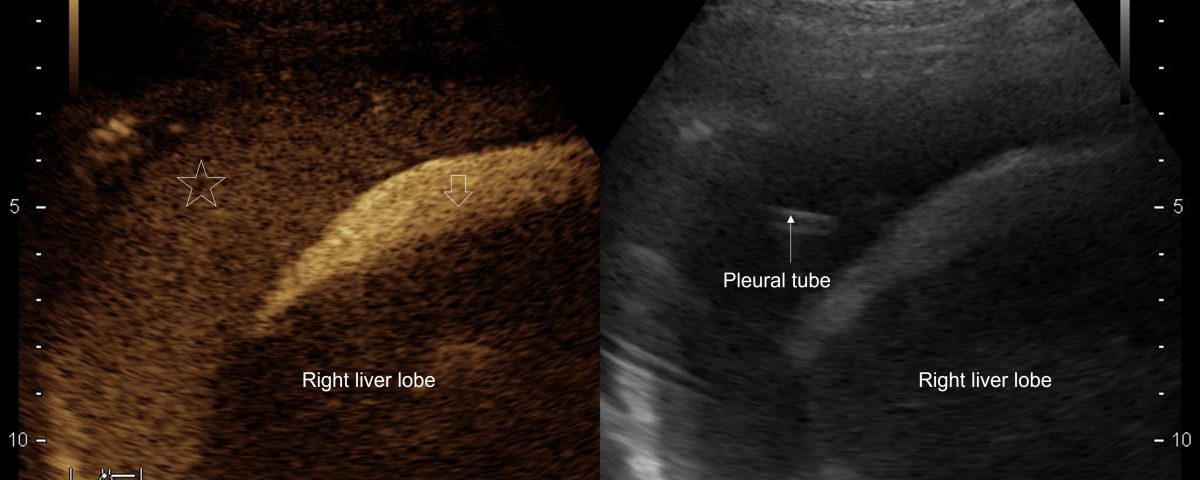
Figure 3: After injection of Saline mixed with only 1 drop of the Ultrasound Contrast Agent SonoVue® into he subdiaphragmatic ascites strong enhancement of the ascitic fluid occurs (↓). A communication between the peritoneal and the right pleural cavity is proven by slightly delayed and less intense enhancement also of the pleural fluid (*)
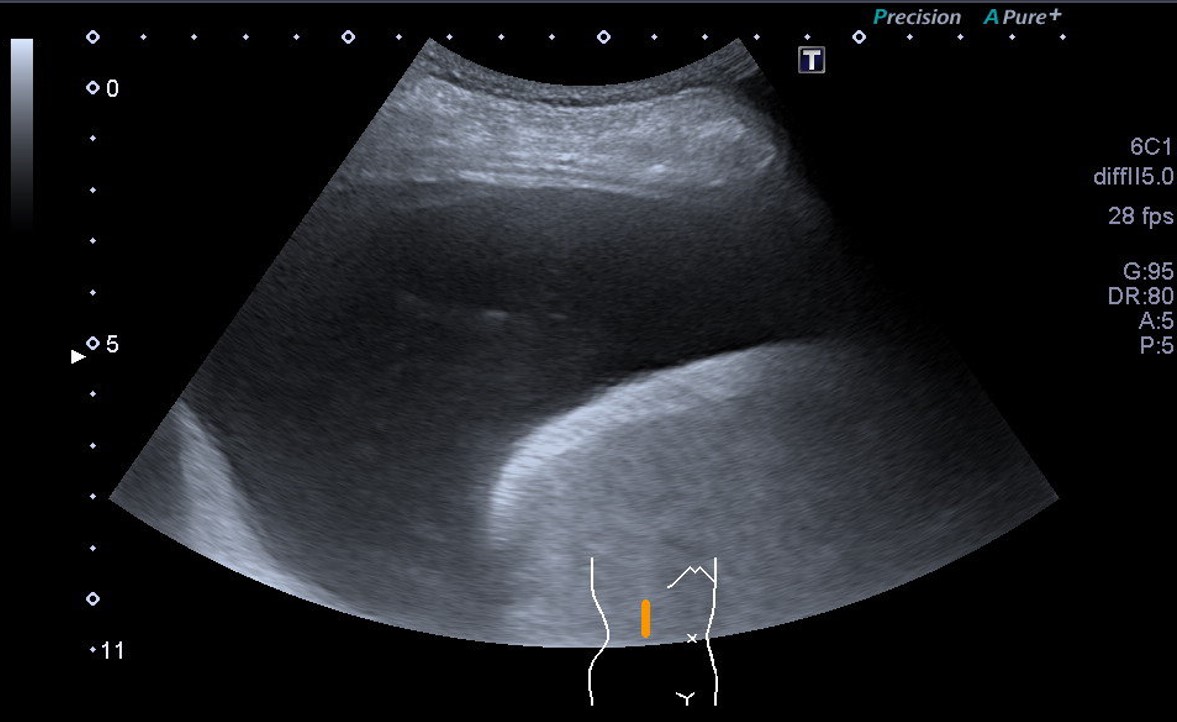
Video 1: US-guided puncture of the subdiaphragmatic ascites for injection of Saline with SonoVue: the echogenic needle tip is seen below the diaphragm.
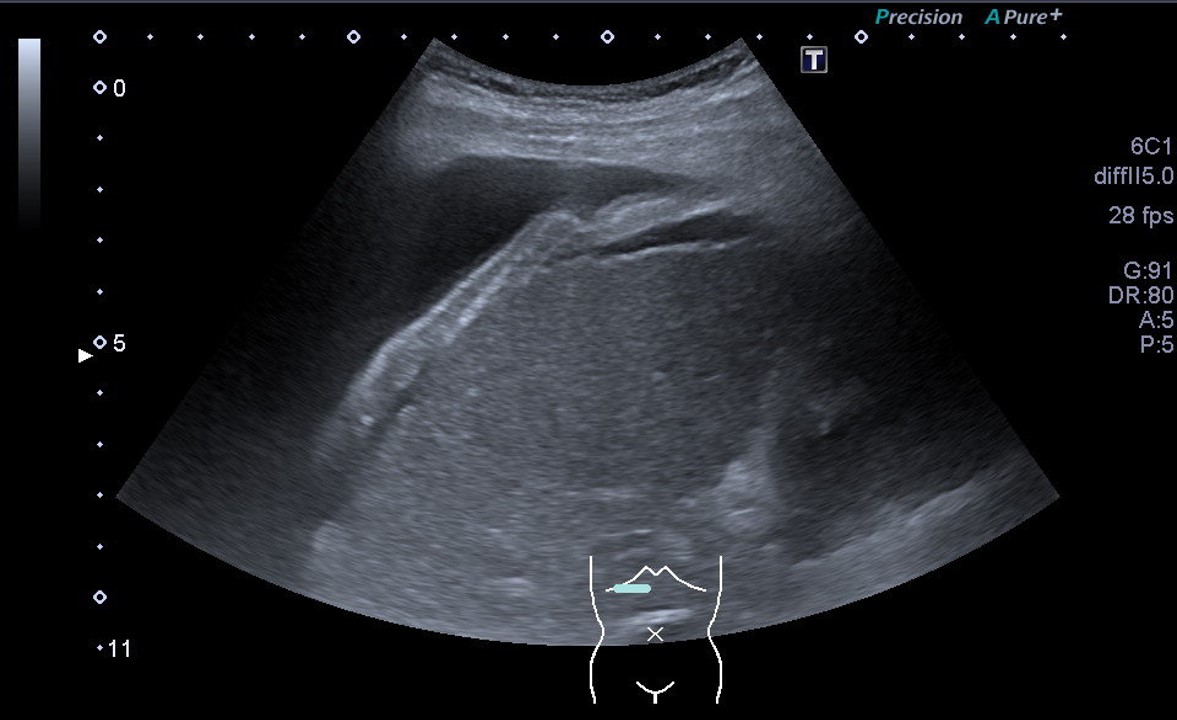
Video 2: 10 ml Saline with a single drop of SonoVue is injected using the needle: a very intense enhacement of ascites is observed, followed by occurence of microbubbles also in the right pleural cavity. The echogenic reflex in the pleural cavity is the indwelling pleural catheter.
There are many causes of unilateral pleural effusions. Diagnostic puncture with biochemical analysis, supplemented, if necessary, by cytological and microbiological analyses, allows differentiation into transudate or exudate and can also provide specific clues to the etiology. In this case, a transudate was detected. In most cases, this will be caused by cardiac insufficiency or hypervolemia. Hepatic hydrothorax should be considered in patients with liver cirrhosis and portal hypertension.
CLINICAL PERSPECTIVE
Hepatic hydrothorax is a rare clinical manifestation of portal hypertension and was described to occur in up to 15% of patients hospitalized due to decompensated liver cirrhosis and ascites. Hepatic hydrothorax virtually always presents with ascites, but often the amount of ascites is relatively small. Typically, hepatic hydrothorax presents as unliteral right-sided pleural effusion. Pathophysiology is related to direct passage of ascitic fluid from the peritoneal cavity to the pleural cavity through small diaphragmatic defects due to an increased abdominal pressure. These small diaphragmatic defects are not detectable with ultrasound or other imaging modalities (1-3).
THERAPY PLANNING
Pleural interventions (therapeutic thoracocentesis, indwelling pleural catheters, pleurodesis) have limited efficacy and are associated with a relatively high risk of infection and mortality (4, 5). Hepatic hydrothorax is treated like ascites aiming at the elimination of the fluid in both peritoneal and pleural cavities by maintaining a negative sodium balance, through dietary sodium intake and diuretics (aldosterone antagonists and loop diuretics). In refractory cases, transjugular intrahepatic stent shunt (TIPPS) and liver transplantation are useful treatment options (1-3). br/>br/> OUTCOME
Hepatic hydrothorax may be complicated by spontaneous bacterial pleuritis and is associated with a poor outcome (6). Risk factors for hepatic hydrothorax are recurrent need for paracentesis, a high bilirubin level, diabetes, and non-use of non-selective beta-blockers (7).
(3) Benz F, Mohr R, Tacke F, Roderburg C. Pulmonary Complications in Patients with Liver Cirrhosis. J Transl Int Med. 2020 Sep 25;8(3):150-158
(4) Hou F, Qi X, Guo X. Effectiveness and Safety of Pleurodesis for Hepatic Hydrothorax: A Systematic Review and Meta-Analysis. Dig Dis Sci 2016; 61: 3321–34.
(5) Gilbert CR, Shojaee S, Maldonado F, Yarmus LB, Bedawi E, Feller-Kopman D, Rahman NM, Akulian JA, Gorden JA. Pleural Interventions in the Management of Hepatic Hydrothorax. Chest. 2022 Jan;161(1):276-283
(6) Matei D, Craciun R, Crisan D, Procopet B, Mocan T, Pasca S, Zaharie R, Popovici B, Sparchez Z. Hepatic Hydrothorax - An Independent Decompensating Event Associated with Long-Term Mortality in Patients with Cirrhosis. J Clin Med. 2021;10(16):3688
(7) Deleuran T, Watson H, Vilstrup H, Jepsen P. Risk Factors for Hepatic Hydrothorax in Cirrhosis Patients with Ascites - A Clinical Cohort Study. Dig Dis Sci. 2021, Epub ahead of print
(8) Foschi FG, Piscaglia F, Pompili M, Corbelli C, Marano G, Righini R, Alvisi V, Gasbarrini G, Bolondi L, Bernard M, Stefanini GF. Real-Time Contrast-Enhanced Ultrasound – a new simple tool for detection of peritoneal-pleural communications in hepatic hydrothorax. Ultraschall in Med 2008;29:538–42.
(9) Sparchez Z, Radu P, Sparchez M, Vasile T, Anton O, Tantau M. Intracavitary Applications of Ultrasound Contrast Agents in Hepatogastroenterology. J Gastrointestin Liver Dis. 2013 Sep;22(3):349-53


![Direct proof of hepatic hydrothorax by intracavitary contrast-enhanced ultrasound </br> [Mar 2022]](https://efsumb.org/wp-content/uploads/2022/04/Fig.3_CoM_2022-scaled.jpg)
