Direct proof of hepatic hydrothorax by intracavitary contrast-enhanced ultrasound [Mar 2022]
April 29, 2022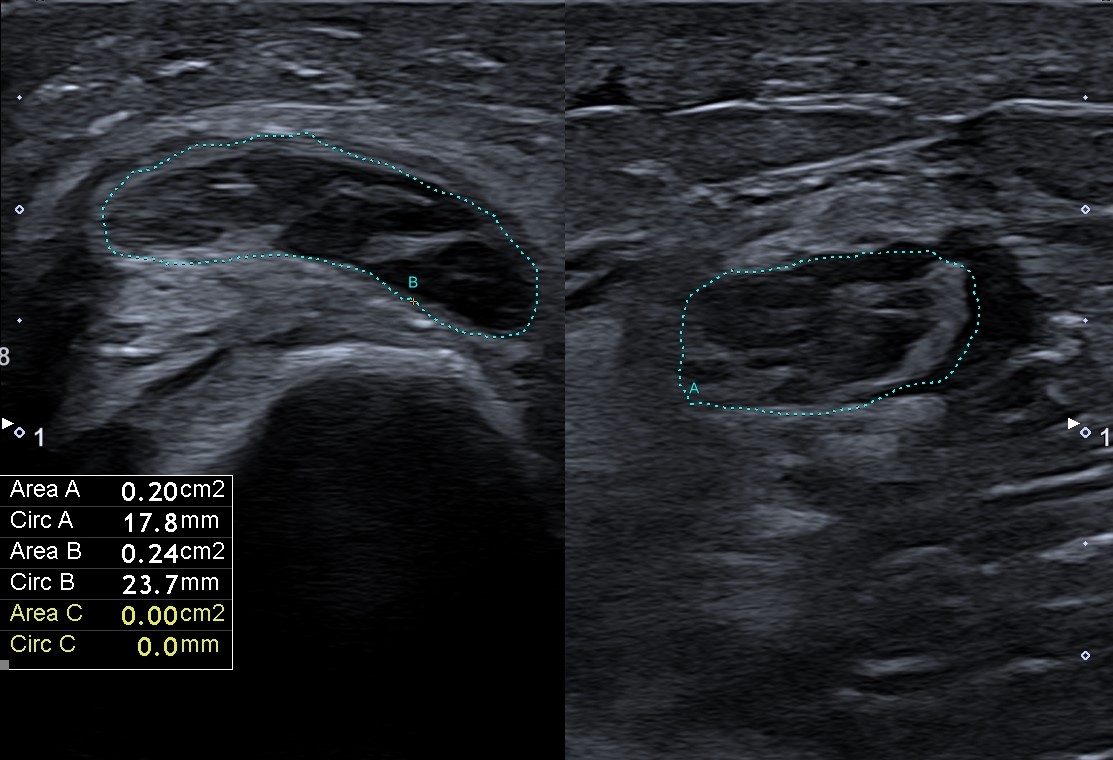
Ultrasonography in the diagnosis of vasculitic neuropathy – a case report [May 2022]
June 10, 2022Gas in the portal system in a patient with Crohn's disease
AUTHORS
Churchev S.1,
Kalcheva V.1,
Getsov P.2,
Genov J.1,
Golemanov B.1
1 Department of Gastroenterology
2 Department of Medical Imaging
University Hospital "Tsaritsa Yoanna – ISUL" – Sofia, Medical University - Sofia
Churchev S.1,
Kalcheva V.1,
Getsov P.2,
Genov J.1,
Golemanov B.1
1 Department of Gastroenterology
2 Department of Medical Imaging
University Hospital "Tsaritsa Yoanna – ISUL" – Sofia, Medical University - Sofia
Video 1 – Multiple speckle-like artefacts (representing gas bubbles) move with the portal system's blood flow.
1Clinical History
A 42-years old female patient with a prior history of Crohn's disease, small intestinal resection, and right hemicolectomy presents to the emergency department with abdominal pain two weeks after hospital admission to the GE department. The patient is receiving oral corticosteroids and is scheduled to initiate biologic therapy with an anti-TNF agent. Laboratory findings show mild leukocytosis and slight elevation of CRP and are otherwise unremarkable. Plain abdominal x-ray shows several air-fluid levels with no free air in the abdomen.
2Image findings
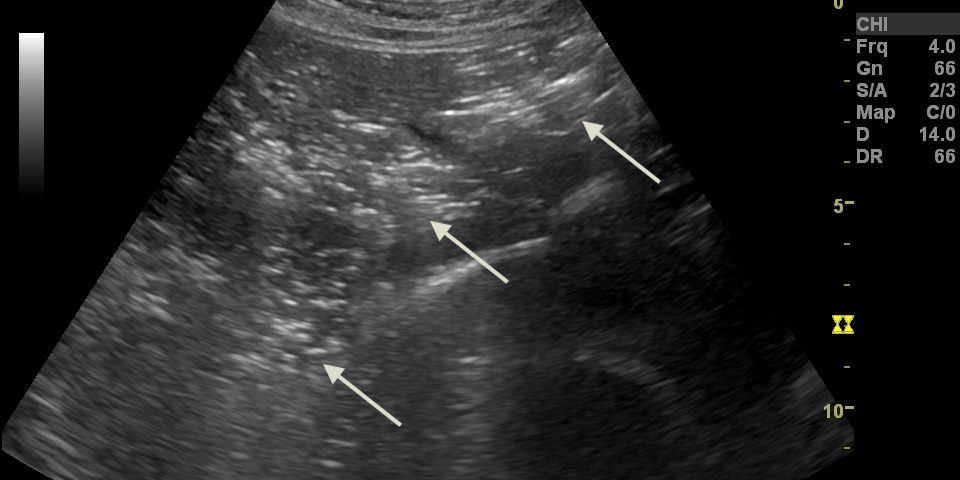
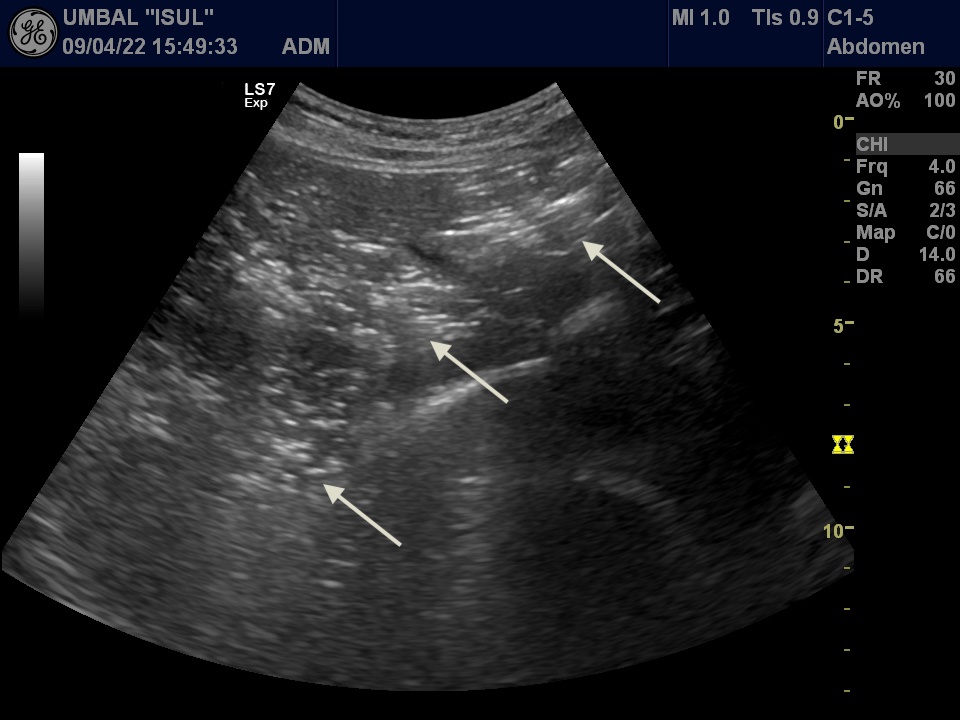
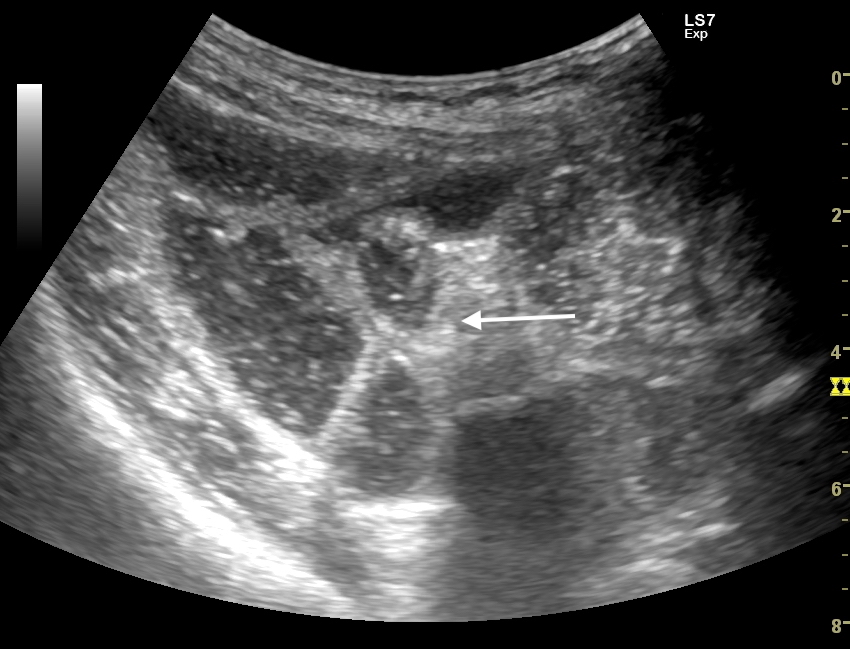
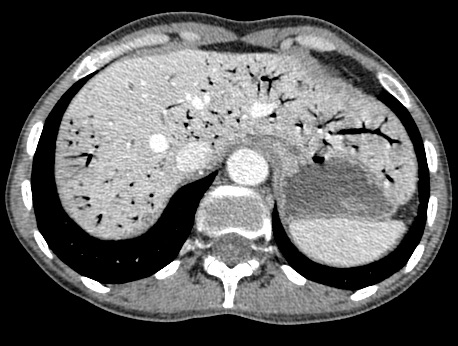
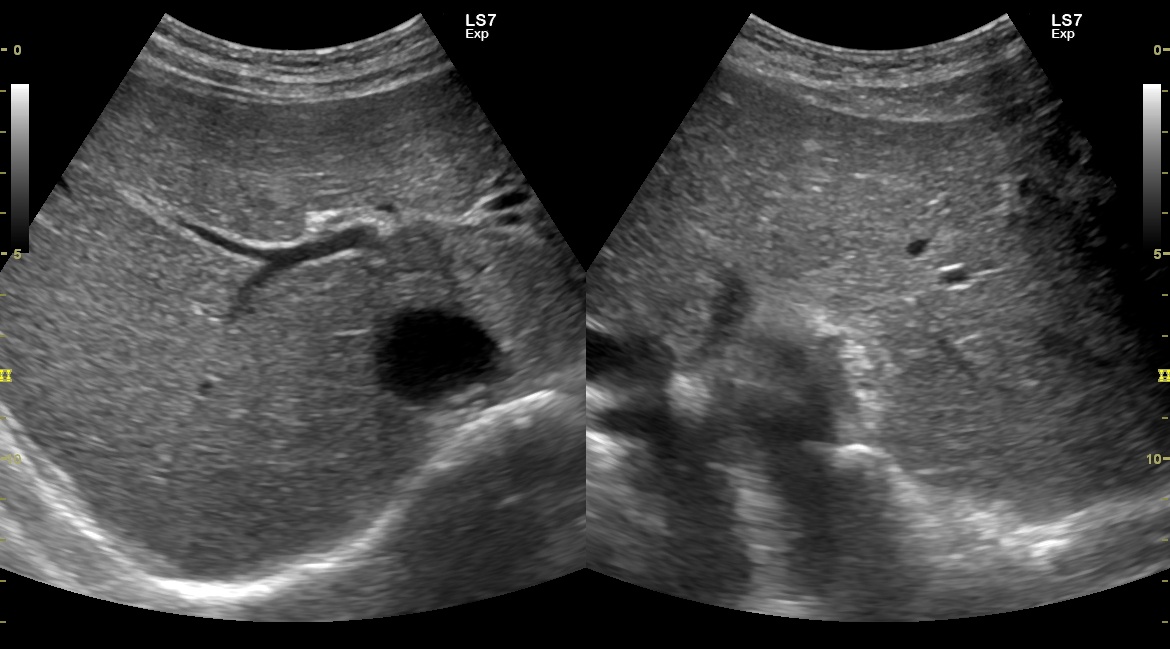
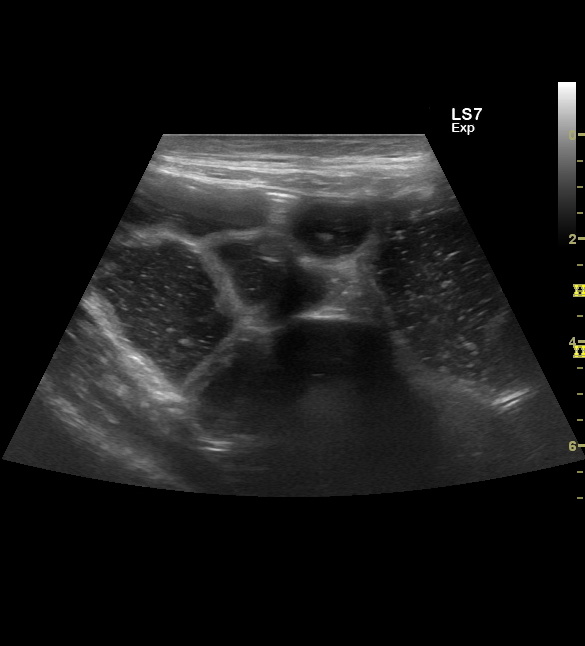
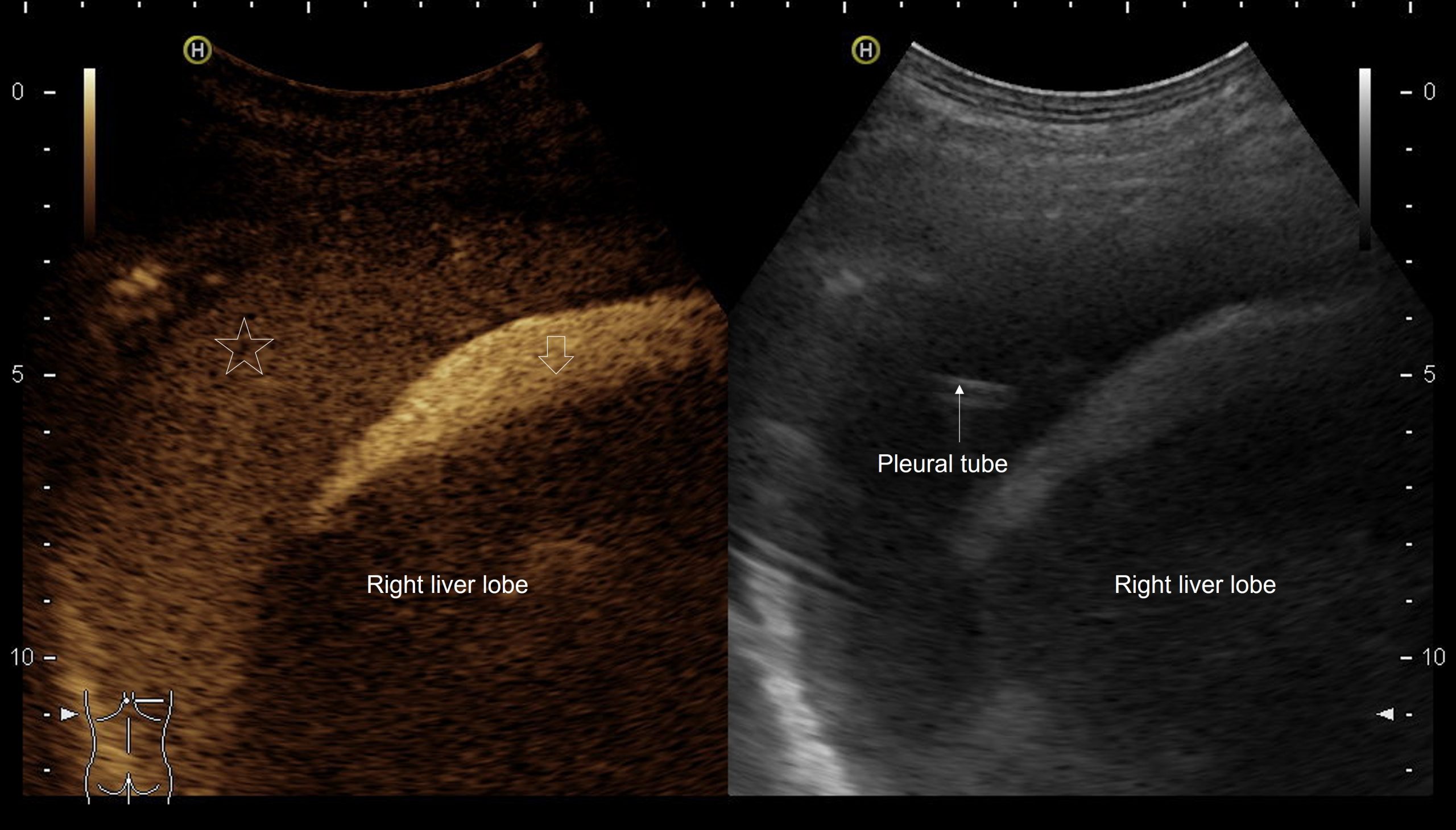
B-mode ultrasound demonstrated multiple hyperechoic speckle-like artefacts moving with the portal vein's blood flow (hepatopetal) (Video. 1). Visualization of the liver parenchyma was obscured by highly hyperechoic areas, especially in the left lobe (Fig. 1). The portal and splenic veins and superior mesenteric artery were patent on Doppler-US examination. A segment of dilated small intestinal bowel loop was seen (Fig 2). There was no ascites. Contrast-enhanced computer tomography (CT) showed no signs of mesenteric thrombosis, but the finding in the liver was initially interpreted as aerobilia (Fig. 3). The CT findings were later reevaluated as intestinal pneumatosis with hepatic portal vein gas (Fig. 4).
3Diagnosis
Based on the typical US image (and revised CT), the final diagnosis was: hepatic portal vein gas (HPVG) caused by intestinal pneumatosis in a patient with Crohn’s disease and small intestinal obstruction due to postoperative adhesions.
4Discussion
BACKGROUND
Hepatic portal venous gas (HPVG) is a rare imaging finding often associated with intestinal ischemia. First described in 1956 in a series of pediatric cases by Wolfe and Evans and in 1960 by Susman and Senturia in an adult patient, early studies showed a mortality rate of 75% (1-3). Later it was recognized that the condition could be seen in a variety of clinical settings, such as IBD (especially Crohn's disease), gastric dilatation, gastric ulcer, diverticulitis, pelvic abscess, necrotizing enterocolitis, intra-peritoneal tumor, cholangitis, pancreatitis, etc., or it can be iatrogenic (after endoscopic procedures and imaging studies - ERCP, colonoscopy, barium enema)(1). Mortality rate reported in studies after the 2000s is 32 to 47,5% (4-6).
CLINICAL PERSPECTIVE
Therapy Planning:
Given the lack of evidence for mesenteric thrombosis and clinical or imaging signs of peritonitis, a multidisciplinary decision for initial conservative treatment with close observation and reevaluation of the need for surgical treatment was taken.
Outcome:
Intravenous supplementation with fluids and electrolytes, nil per os and naso-gastric decompression led to positive clinical response, reduction and later disappearance of the abdominal pain. On the second day of admission, there were no imaging signs of portal vein gas but persistently dilated small intestinal loops (Fig 5-6). A decision for surgical treatment was taken – adhesive small bowel obstruction was found, and surgical adhesiolysis was performed with an uneventful postoperative course.
Prognosis:
HPVG can result from numerous intraabdominal conditions and diseases, often with detrimental consequences. Rarely it can have a benign course or even no apparent clinical significance. The patient in the reported case is followed up with further therapeutic interventions to control Crohn's disease activity and prevent future surgical interventions.
Hepatic portal venous gas (HPVG) is a rare imaging finding often associated with intestinal ischemia. First described in 1956 in a series of pediatric cases by Wolfe and Evans and in 1960 by Susman and Senturia in an adult patient, early studies showed a mortality rate of 75% (1-3). Later it was recognized that the condition could be seen in a variety of clinical settings, such as IBD (especially Crohn's disease), gastric dilatation, gastric ulcer, diverticulitis, pelvic abscess, necrotizing enterocolitis, intra-peritoneal tumor, cholangitis, pancreatitis, etc., or it can be iatrogenic (after endoscopic procedures and imaging studies - ERCP, colonoscopy, barium enema)(1). Mortality rate reported in studies after the 2000s is 32 to 47,5% (4-6).
CLINICAL PERSPECTIVE
Therapy Planning:
Given the lack of evidence for mesenteric thrombosis and clinical or imaging signs of peritonitis, a multidisciplinary decision for initial conservative treatment with close observation and reevaluation of the need for surgical treatment was taken.
Outcome:
Intravenous supplementation with fluids and electrolytes, nil per os and naso-gastric decompression led to positive clinical response, reduction and later disappearance of the abdominal pain. On the second day of admission, there were no imaging signs of portal vein gas but persistently dilated small intestinal loops (Fig 5-6). A decision for surgical treatment was taken – adhesive small bowel obstruction was found, and surgical adhesiolysis was performed with an uneventful postoperative course.
Prognosis:
HPVG can result from numerous intraabdominal conditions and diseases, often with detrimental consequences. Rarely it can have a benign course or even no apparent clinical significance. The patient in the reported case is followed up with further therapeutic interventions to control Crohn's disease activity and prevent future surgical interventions.
5Teaching Points
The presence of HPVG is a worrisome imaging finding. It can be seen on B-mode US as intense hyperechoic non-shadowing speckles in the portal vein (following hepatopetal direction) and/or adjacent liver parenchyma. The gas trapped in the liver (sometimes termed "intrahepatic gas") can obscure and make the portal vein difficult for visualization (7). HPVG may be difficult to differentiate from air in the biliary tree (on CT), intrahepatic inferior vena cava and hepatic parenchyma (gas-forming liver abscess). If HVPG is suspected, it requires prompt assessment, including contrast-enhanced CT (8).
6References
(1) Pan Y. Hepatic portal vein gas associated with intestinal ischemia and acute gastric dilatation: a case report. Ann Palliat Med 2021;10(6):7095-7098.
(2) Wolfe JN, Evans WA. Gas in the portal veins of the liver in infants; a roentgenographic demonstration with postmortem anatomical correlation. Am J Roentgenol Radium Ther Nucl Med 1955;74:486-8.
(3) Sebastià C, Quiroga S, Espin E, et al. Portomesenteric Vein Gas: Pathologic Mechanisms, CT Findings, and Prognosis. RadioGraphics 2000; 20(5), 1213–1224.
(4) Fujii, M., Yamashita, S., Tanaka, M. et al. Clinical features of patients with hepatic portal venous gas. BMC Surg 2020;20: 300.
(5) Nelson AL, Millington TM, Sahani D, et al. Hepatic portal venous gas: the ABCs of management. Arch Surg 2009;144:575-81.
(6) Gonda M, Osuga T, Ikura Y, et al. Optimal treatment strategies for hepatic portal venous gas: A retrospective assessment. World J Gastroenterol 2020;26(14):1628-1637.
(7) Liang KW, Huang HH, Tyan YS, et al. Hepatic Portal Venous Gas: Review of Ultrasonographic Findings and the Use of the "Meteor Shower" Sign to Diagnose It. Ultrasound Q. 2018 Dec;34(4):268-271.
(8) Daneshmand A, Parys S, Rao S, et al. (2020). Portal venous gas: different aetiologies and their respective outcomes. ANZ J Surg. 2020 May;90(5):767-771.
(2) Wolfe JN, Evans WA. Gas in the portal veins of the liver in infants; a roentgenographic demonstration with postmortem anatomical correlation. Am J Roentgenol Radium Ther Nucl Med 1955;74:486-8.
(3) Sebastià C, Quiroga S, Espin E, et al. Portomesenteric Vein Gas: Pathologic Mechanisms, CT Findings, and Prognosis. RadioGraphics 2000; 20(5), 1213–1224.
(4) Fujii, M., Yamashita, S., Tanaka, M. et al. Clinical features of patients with hepatic portal venous gas. BMC Surg 2020;20: 300.
(5) Nelson AL, Millington TM, Sahani D, et al. Hepatic portal venous gas: the ABCs of management. Arch Surg 2009;144:575-81.
(6) Gonda M, Osuga T, Ikura Y, et al. Optimal treatment strategies for hepatic portal venous gas: A retrospective assessment. World J Gastroenterol 2020;26(14):1628-1637.
(7) Liang KW, Huang HH, Tyan YS, et al. Hepatic Portal Venous Gas: Review of Ultrasonographic Findings and the Use of the "Meteor Shower" Sign to Diagnose It. Ultrasound Q. 2018 Dec;34(4):268-271.
(8) Daneshmand A, Parys S, Rao S, et al. (2020). Portal venous gas: different aetiologies and their respective outcomes. ANZ J Surg. 2020 May;90(5):767-771.