- European Federation of Societies for Ultrasound in Medicine and Biology ~ Educating all for competence to practice ultrasound safely

Gas in the portal system in a patient with Crohn’s disease [Apr 2022]
May 13, 2022
Ischemic Colitis as Complication of SARS-CoV-2 Infection [June 2022]
July 4, 2022Ultrasonography in the diagnosis of vasculitic neuropathy – a case report
AUTHORS
Dace Gailīte¹,
Viktors Ļiņovs²,
¹ Rīga Stradiņš University, Faculty of Medicine, Latvia
² Rīga 2nd Hospital, Latvia
Dace Gailīte¹,
Viktors Ļiņovs²,
¹ Rīga Stradiņš University, Faculty of Medicine, Latvia
² Rīga 2nd Hospital, Latvia
1Clinical History
A 32-year-old man presented to the ultrasound department complaining of pain in the right arm and numbness affecting the right fourth and fifth fingers. Hand pain has been worsening over the past two weeks. A week before the patient also had a purpuric rash on the right arm (Fig. 1). Prior to ultrasonography examination the nerve conduction study (NCS) of the right arm had been performed. It revealed severe axonal damage of the ulnar nerve at the level of the arm and proximal 1/3 of the forearm.
2Image findings
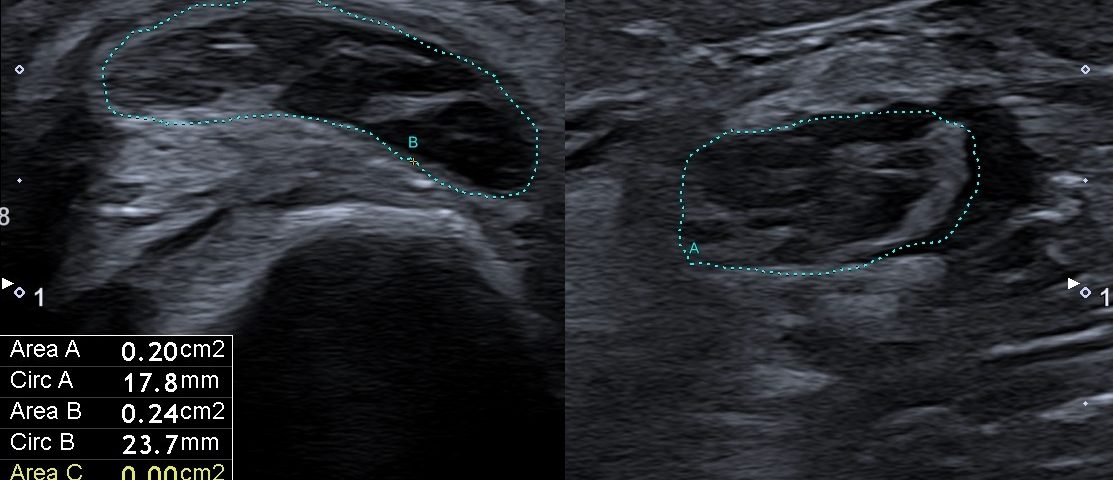
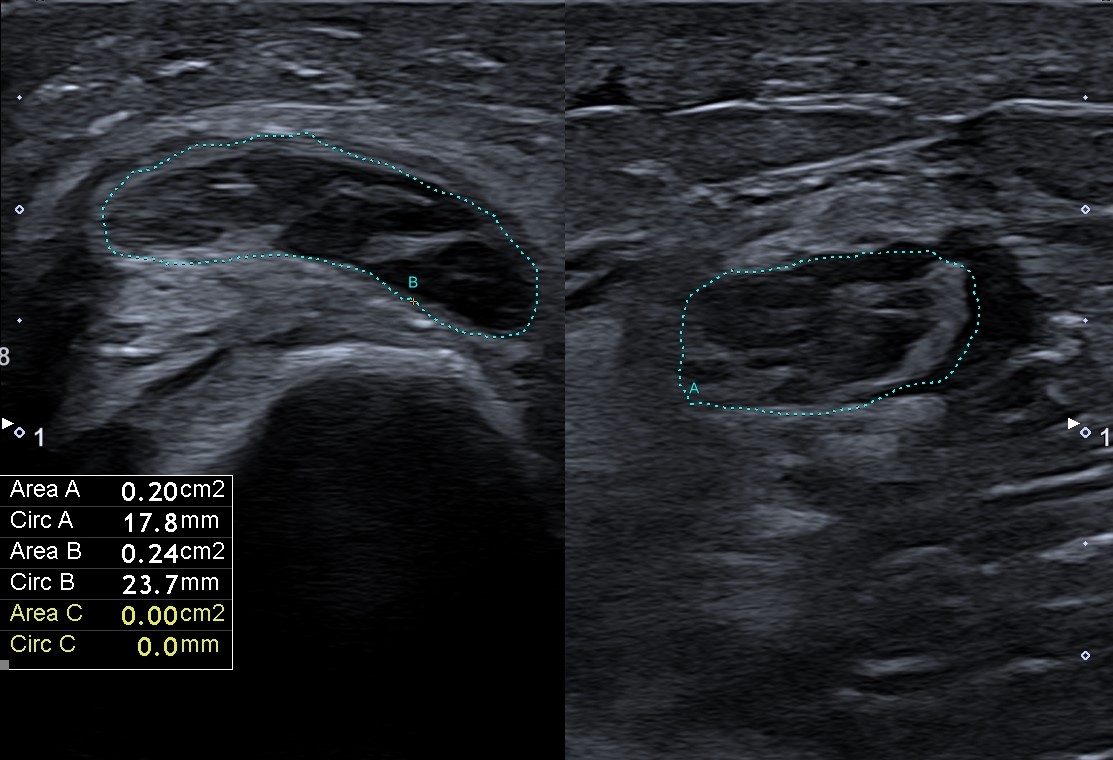
Ultrasonography (US) of the right arm revealed diffuse right ulnar nerve enlargement at the level of the arm and forearm (it was greater compared to the contralateral side for 50 %), more pronounced in the cubital region – 0,24cm² (Fig. 2A). Edema of individual fascicles of brachial plexus and nonhomogeneous and hypervascular periarterial tissue with edema of the right axillary (Fig. 2B), brachial , ulnar and IV and V digital arteries were detected. The previously mentioned artery wall thickening was more pronounced distally. US of the abdominal aorta revealed a 4 mm thick hypoechoic area (Fig. 3) surrounding the aorta anteriorly at the level of the renal arteries.
FURTHER EVALUATION:
Considering the signs of ischemia and vasculitis, the patient was referred to the emergency department and the next day was admitted to the hospital.
At admission he still had pain in the right arm and signs of ischemia affecting the right fourth and fifth fingers. The patient also admitted to have a sub-febrile temperature and night sweats. Physical examination revealed bluish and white discoloration of the right fourth and fifth fingers.
An urgent echocardiography and computed tomography angiography were performed both with no acute findings. Laboratory evaluation revealed increased white blood cell count due to elevated neutrophils, increased C-reactive protein (CRP 11,28 mg/L), decreased aspartate aminotransferase. Coagulation tests, creatinine, alanine aminotransferase and gamma-glutamyl transferase were within normal limits. Urine analysis was normal. Other laboratory tests and autoimmune profile blood tests were negative except for elevated C4, decreased thyroid-stimulating hormone and serum protein electrophoresis which revealed elevated quantitative IgE.
FURTHER EVALUATION:
Considering the signs of ischemia and vasculitis, the patient was referred to the emergency department and the next day was admitted to the hospital.
At admission he still had pain in the right arm and signs of ischemia affecting the right fourth and fifth fingers. The patient also admitted to have a sub-febrile temperature and night sweats. Physical examination revealed bluish and white discoloration of the right fourth and fifth fingers.
An urgent echocardiography and computed tomography angiography were performed both with no acute findings. Laboratory evaluation revealed increased white blood cell count due to elevated neutrophils, increased C-reactive protein (CRP 11,28 mg/L), decreased aspartate aminotransferase. Coagulation tests, creatinine, alanine aminotransferase and gamma-glutamyl transferase were within normal limits. Urine analysis was normal. Other laboratory tests and autoimmune profile blood tests were negative except for elevated C4, decreased thyroid-stimulating hormone and serum protein electrophoresis which revealed elevated quantitative IgE.
3Diagnosis
Based on the typical US image and other results from laboratory and imaging studies performed in the hospital, the final diagnosis was medium and large vessel vasculitis and right ulnar nerve axonal mononeuropathy.
4Discussion
BACKGROUND
Vasculitic neuropathy (VN) can be a part of primary or secondary systemic vasculitis, or it also can present as a non-systemic VN (1). The main pathophysiological feature of VN is inflammation of the walls of nutrient and epineural arteries which have limited evaluation possibilities using ultrasound. Evaluation of major arteries, which were inflammed in our case, is instead possible.It is reported that the common final path is thrombosis and ischaemic damage. Most affected nerves usually are the peroneal and/or tibial nerve in the lower extremity and the ulnar nerve in the upper extremity (2). The diagnostic gold standard for VN consists of clinical examination, NCS and laboratory tests such as antineutrophil cytoplasmic antibodies, erythrocyte sedimentation rate, antinuclear antibodies, and the rheumatoid factor. Definite diagnosis can only be done by a peripheral nerve biopsy. However, the sensitivity of nerve biopsy is no more than 50–60% (2,3).
Diffuse enlargement of major nerves in the arm on US can be considered as one of the major signs for VN (1). With high-resolution sonography superficial peripheral nerves can be thoroughly investigated. US allows the detailed visualisation of nerve fascicles and small structural changes as well as vascularization assessment; therefore, it might advance to become a useful additional tool to electrodiagnostic studies (4).
CLINICAL PERSPECTIVE
Therapy Planning:
Because of the US and neurography findings the patient was treated for presumed systemic vasculitis with corticosteroids.
Outcome:
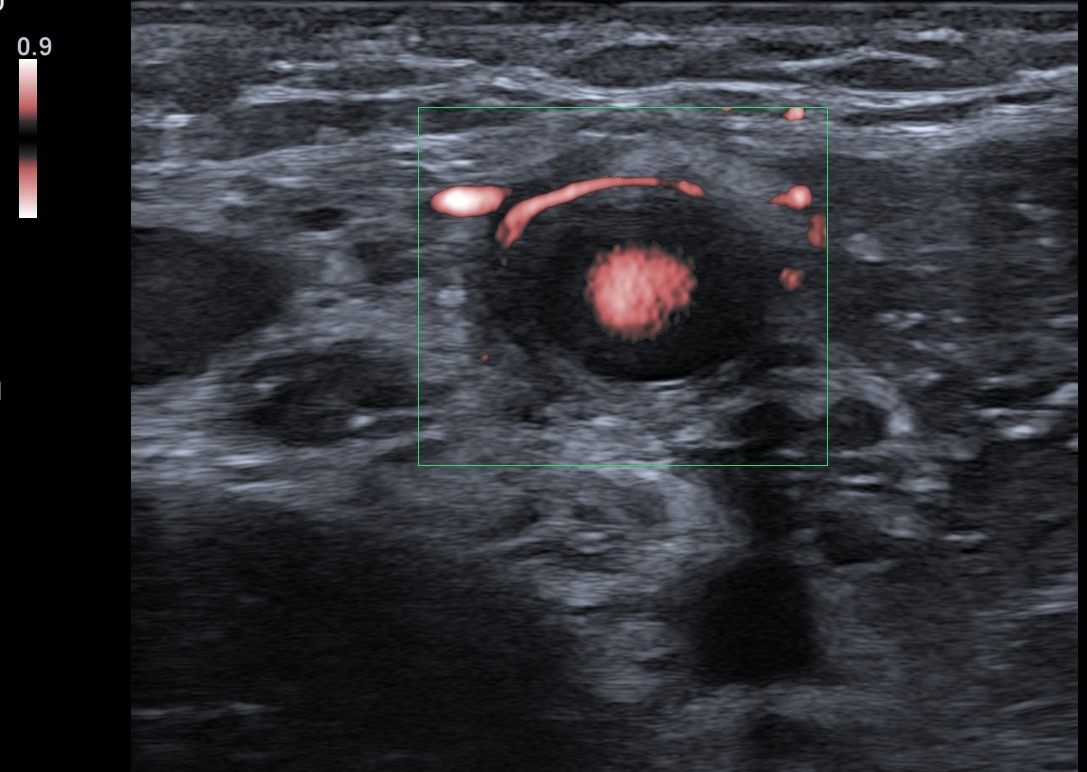
After a five-day treatment with corticosteroids, an additional US was performed, which concluded that there was no edema surrounding previously affected arteries and no other acute findings. The patient appeared for the follow-up visit after a month when a Doppler ultrasound examination revealed no acute inflammation signs. However, the right ulnar nerve enlargement was still detected up to 0.2cm² (it was larger compared to the contralateral side for 50 %)(Fig. 4A-B). Compared to the previous US exam, there seemed to be less edema.
Prognosis:
Standard treatment of systemic vasculitic neuropathy (SVN) and classical non SVN are corticosteroids which were also used in our case (5). Doppler US of affected arteries shows hypoechoic edematous wall swelling in acute arteritis that disappears with corticosteroid treatment after 1–3 weeks in most patients. Ultrasound displays a wall swelling of more than 1.0 mm; cases with a wall thickening of 1.5 mm or more are regarded as definite cases. Sometimes axillary or proximal brachial arteries are occluded due to vasculitis (6,7).
Vasculitic neuropathy (VN) can be a part of primary or secondary systemic vasculitis, or it also can present as a non-systemic VN (1). The main pathophysiological feature of VN is inflammation of the walls of nutrient and epineural arteries which have limited evaluation possibilities using ultrasound. Evaluation of major arteries, which were inflammed in our case, is instead possible.It is reported that the common final path is thrombosis and ischaemic damage. Most affected nerves usually are the peroneal and/or tibial nerve in the lower extremity and the ulnar nerve in the upper extremity (2). The diagnostic gold standard for VN consists of clinical examination, NCS and laboratory tests such as antineutrophil cytoplasmic antibodies, erythrocyte sedimentation rate, antinuclear antibodies, and the rheumatoid factor. Definite diagnosis can only be done by a peripheral nerve biopsy. However, the sensitivity of nerve biopsy is no more than 50–60% (2,3).
Diffuse enlargement of major nerves in the arm on US can be considered as one of the major signs for VN (1). With high-resolution sonography superficial peripheral nerves can be thoroughly investigated. US allows the detailed visualisation of nerve fascicles and small structural changes as well as vascularization assessment; therefore, it might advance to become a useful additional tool to electrodiagnostic studies (4).
CLINICAL PERSPECTIVE
Therapy Planning:
Because of the US and neurography findings the patient was treated for presumed systemic vasculitis with corticosteroids.
Outcome:
After a five-day treatment with corticosteroids, an additional US was performed, which concluded that there was no edema surrounding previously affected arteries and no other acute findings. The patient appeared for the follow-up visit after a month when a Doppler ultrasound examination revealed no acute inflammation signs. However, the right ulnar nerve enlargement was still detected up to 0.2cm² (it was larger compared to the contralateral side for 50 %)(Fig. 4A-B). Compared to the previous US exam, there seemed to be less edema.
Prognosis:
Standard treatment of systemic vasculitic neuropathy (SVN) and classical non SVN are corticosteroids which were also used in our case (5). Doppler US of affected arteries shows hypoechoic edematous wall swelling in acute arteritis that disappears with corticosteroid treatment after 1–3 weeks in most patients. Ultrasound displays a wall swelling of more than 1.0 mm; cases with a wall thickening of 1.5 mm or more are regarded as definite cases. Sometimes axillary or proximal brachial arteries are occluded due to vasculitis (6,7).
5Teaching Points
Focal cross-sectional areas (CSA) enlargement in one or more nerves in electrophysiologically axonal neuropathies can be a hint for VN and thus facilitate diagnostic and therapeutic procedures. In this case, ultrasound played an important role in the initial assessment of arm pain and finger numbness and was a valuable investigation tool of peripheral nerves and affected arteries (8). Nerve ultrasound is a non-invasive diagnostic tool for the confirmation of peripheral nerve vasculitis supplementary to electrophysiological studies. It is easy to use in experienced hands, is not invasive and has no relevant side effects. Findings can be explained to the patient during the examination. Ultrasonography can provide appreciable diagnostic performance for VN (6).
6References
(1.) Goedee HS, van der Pol WL, van Asseldonk JH, Vrancken A, Notermans NC, Visser LH et al.: Nerve sonography to detect peripheral nerve involvement in vasculitis syndromes. Neurology. Clinical practice 2016; 6: 293–303.
(2.) Grimm A, Décard BF, Bischof A, Axer H.: Ultrasound of the peripheral nerves in systemic vasculitic neuropathies. J Neurol Sci 2014; 347: 44-49.
(3.) Collins MP, Arnold WD, Kissel JT: The neuropathies of vasculitis. Neurologic Clin 2013; 31: 557-595.
(4.) Peer S, Bodner G: High-Resolution Sonography of the Peripheral Nervous System. American Journal of Neuroradiology 2009; 30: 59-60.
(5.) Blaes F: Diagnosis and therapeutic options for peripheral vasculitic neuropathy. Ther Adv Musculoskelet 2015; 7: 45-55.
(6.) Schmidt WA: Role of ultrasound in the understanding and management of vasculitis. Ther Adv Musculoskelet Dis. 2014; 6: 39-47.
(7.)Schmidt WA: Imaging in vasculitis. Best Pract Res Clin Rheumatol 2013; 27: 107-118.
(8.) Leupold D, Felbecker A, Tettenborn B, Hundsberger T: Nerve Ultrasound as a Decisive Tool in Nonsystemic Vasculitic Neuropathy - case report. Case Rep Neurol. 2016; 8: 108-114.
(2.) Grimm A, Décard BF, Bischof A, Axer H.: Ultrasound of the peripheral nerves in systemic vasculitic neuropathies. J Neurol Sci 2014; 347: 44-49.
(3.) Collins MP, Arnold WD, Kissel JT: The neuropathies of vasculitis. Neurologic Clin 2013; 31: 557-595.
(4.) Peer S, Bodner G: High-Resolution Sonography of the Peripheral Nervous System. American Journal of Neuroradiology 2009; 30: 59-60.
(5.) Blaes F: Diagnosis and therapeutic options for peripheral vasculitic neuropathy. Ther Adv Musculoskelet 2015; 7: 45-55.
(6.) Schmidt WA: Role of ultrasound in the understanding and management of vasculitis. Ther Adv Musculoskelet Dis. 2014; 6: 39-47.
(7.)Schmidt WA: Imaging in vasculitis. Best Pract Res Clin Rheumatol 2013; 27: 107-118.
(8.) Leupold D, Felbecker A, Tettenborn B, Hundsberger T: Nerve Ultrasound as a Decisive Tool in Nonsystemic Vasculitic Neuropathy - case report. Case Rep Neurol. 2016; 8: 108-114.