Ultrasonography in the diagnosis of vasculitic neuropathy – a case report [May 2022]
June 10, 2022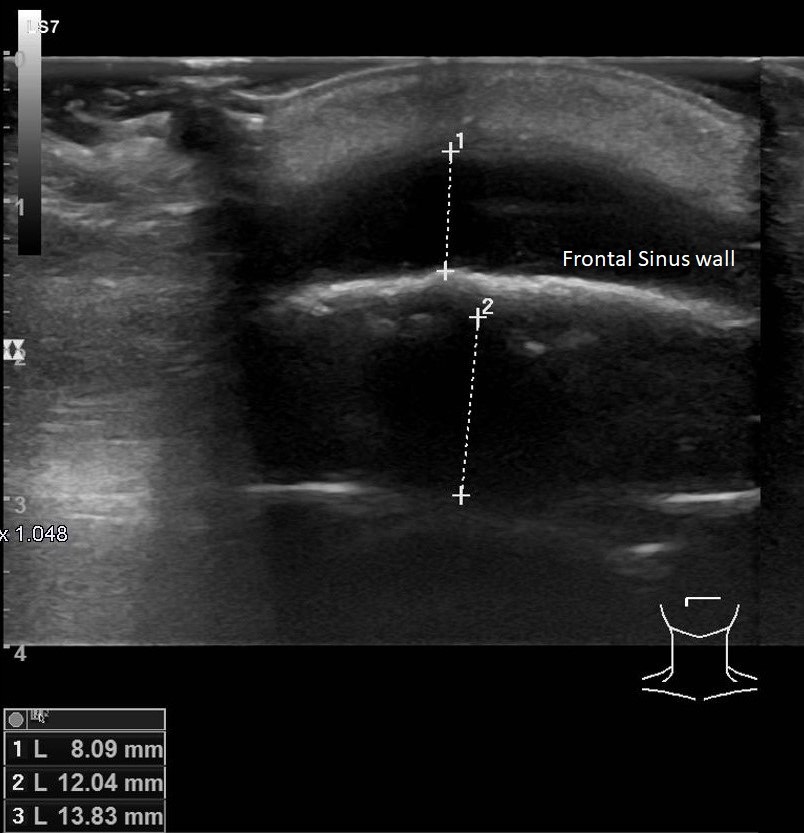
Sonographic Diagnosis of a Pott’s Puffy Tumor in a 5-year-old-girl [Jul 2022]
August 4, 2022Ischemic Colitis as Complication of SARS-CoV-2 Infection
AUTHORS
Federica Lepore [1]
Manuela Nebuloni [2]
Giovanni Maconi [3]
1 Department of Internal Medicine, San Matteo Hospital Foundation, University of Pavia, Italy
2 Pathology Unit, Luigi Sacco Hospital and Department of Biomedical and Clinical Sciences, University of Milan, Milano, Italy
3Gastrointestinal Unit, Department of Biomedical and Clinical Sciences “Luigi Sacco” University Hospital, Milan, Italy
Federica Lepore [1]
Manuela Nebuloni [2]
Giovanni Maconi [3]
1 Department of Internal Medicine, San Matteo Hospital Foundation, University of Pavia, Italy
2 Pathology Unit, Luigi Sacco Hospital and Department of Biomedical and Clinical Sciences, University of Milan, Milano, Italy
3Gastrointestinal Unit, Department of Biomedical and Clinical Sciences “Luigi Sacco” University Hospital, Milan, Italy
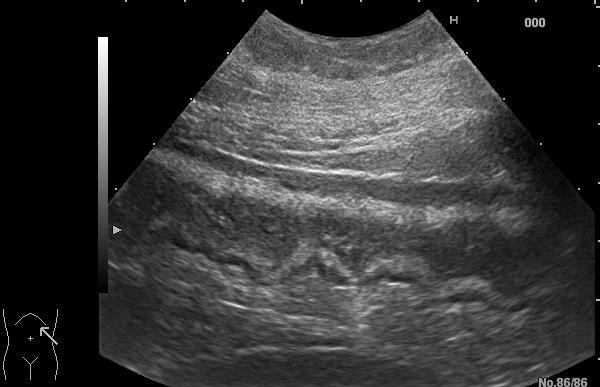
Video 1: IUS scan of the colon starting form splenic flexure up to sigmoid colon. Proximal segment of the bowel showed a homogenous wall thickening, with preserved wall stratification and loss of haustration, and pericolic fat tissue hyperechogenicity
Video 2: IUS scan of the left colon 3 weeks later, showing normal colonic walls, with preserved stratification and solid fecal content
1Clinical History
A 49-year-old man was referred to emergency department complaining of crampy abdominal pain, vomiting, erratic bowel movements with multiple episodes of hematochezia since 7 days. There was no relevant occurrence in his past medical history, except a paucisymptomatic COVID-19, 3 weeks prior to presentation. Laboratory data revealed WBC 16410/mm3, Hb 13.5 g/dL, Hct 42,5%. Stool culture, C difficile PCR and SARS-CoV-2 PCR were negative.
2Image findings
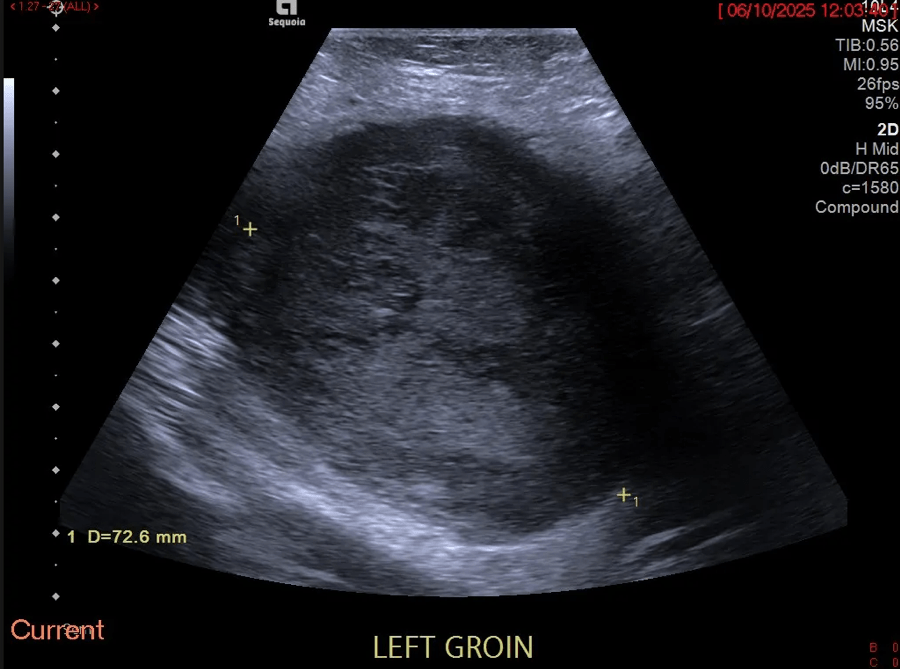
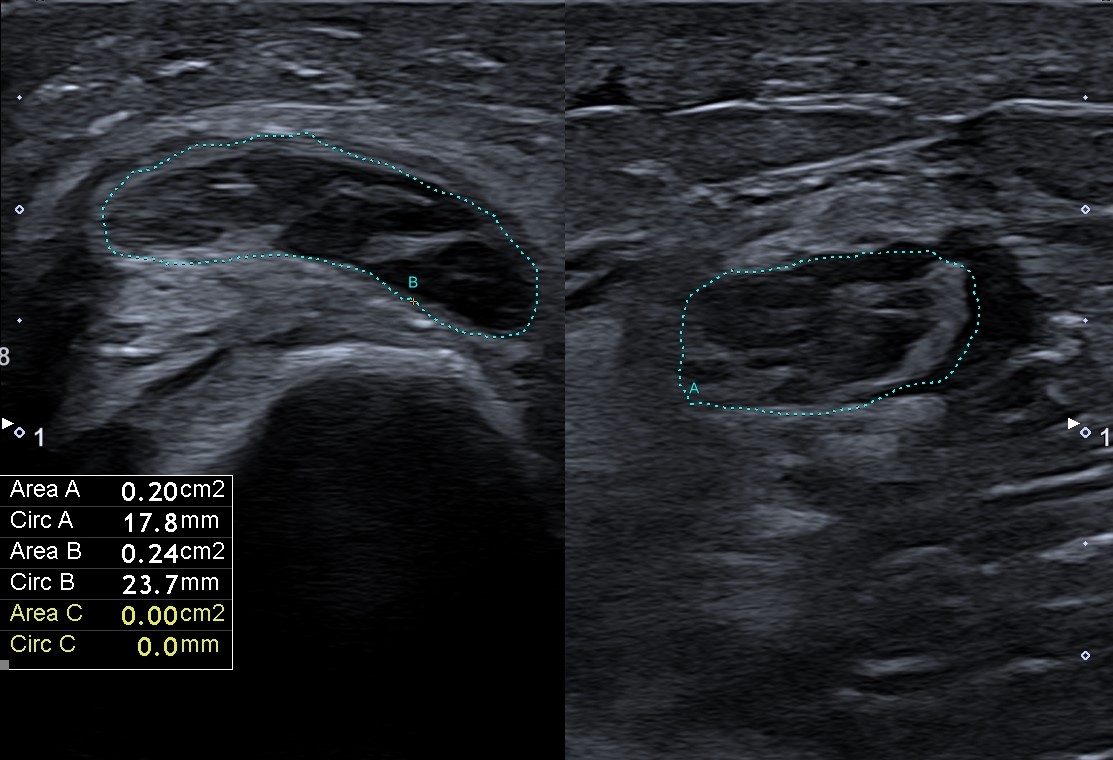
Intestinal ultrasound (IUS) showed an homogenous and circumferential wall thickening of descending colon (up to 6mm) from splenic flexure to sigmoid colon, with preserved wall stratification and without significant vascularization at color Doppler, but with loss of colonic haustration and with pericolic fat tissue hyperechogenicity (Figure 1, Video 1).
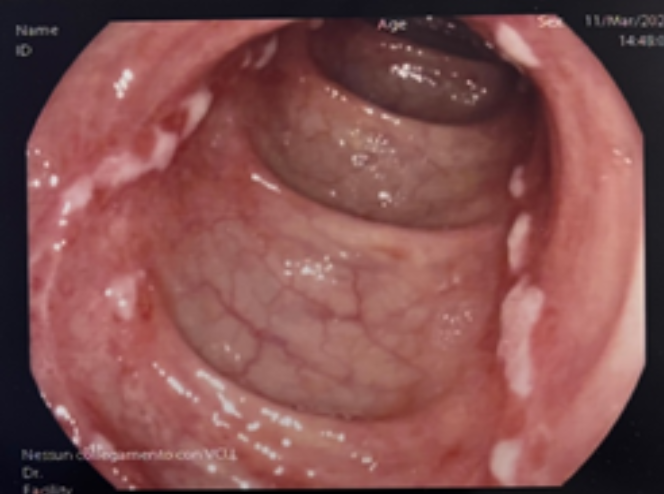
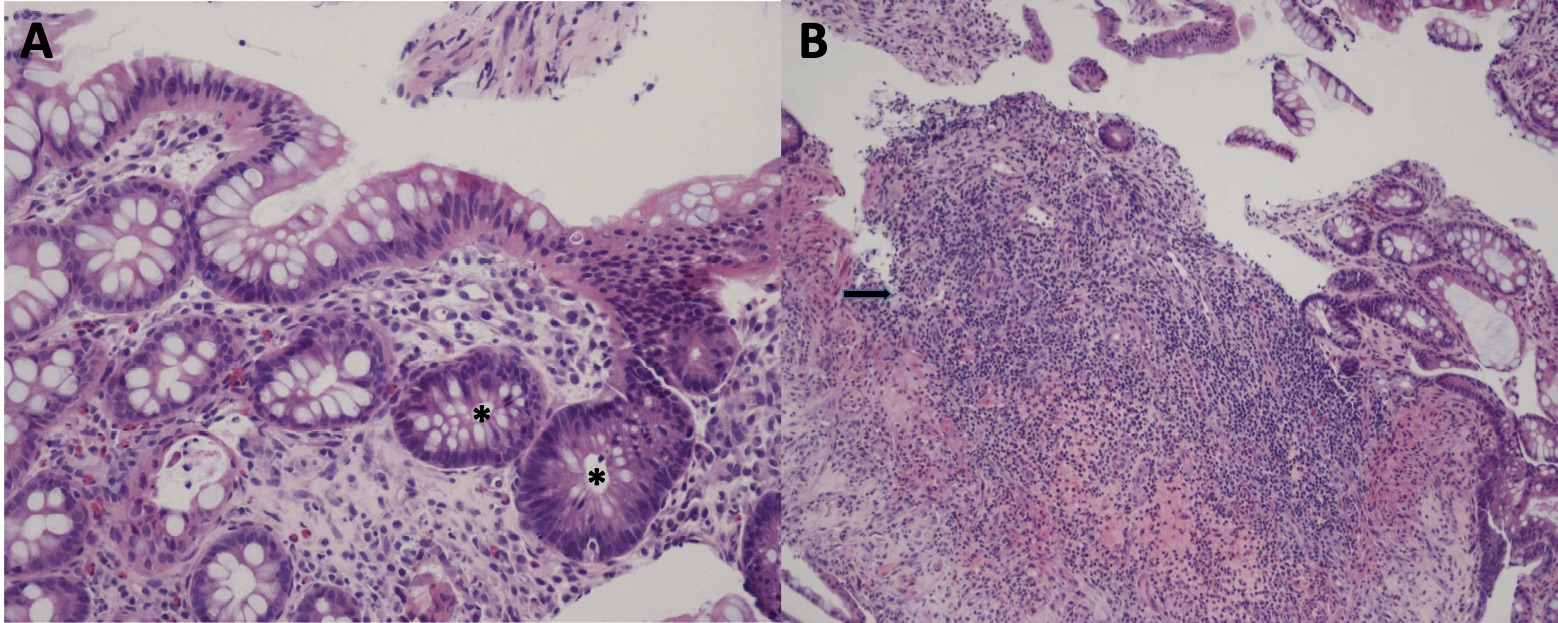
Colonoscopy revealed superficial, nonbleeding ulcers with surrounding mucosal erythema involving the proximal sigmoid and descending colon (Figure 2). Colonic biopsies demonstrated focal glandular reactive-regenerative aspects associated with area characterized by tissue of granulation, hyalinization of lamina propria and aspects of re-epithelialization (Figure 3).
The patient was discharged without therapy, with clinical and IUS follow-up. The following weeks were uneventful with persistent good clinical conditions. The IUS performed 3 weeks later showed the complete disappearance of the wall thickening and restoration of haustra of the left colon (Video 2).
Colonoscopy revealed superficial, nonbleeding ulcers with surrounding mucosal erythema involving the proximal sigmoid and descending colon (Figure 2). Colonic biopsies demonstrated focal glandular reactive-regenerative aspects associated with area characterized by tissue of granulation, hyalinization of lamina propria and aspects of re-epithelialization (Figure 3).
The patient was discharged without therapy, with clinical and IUS follow-up. The following weeks were uneventful with persistent good clinical conditions. The IUS performed 3 weeks later showed the complete disappearance of the wall thickening and restoration of haustra of the left colon (Video 2).
3Diagnosis
COVID-19-associated ischemic colitis.
4Discussion
BACKGROUND
Patients with COVID-19 predominantly have respiratory symptoms, but gastrointestinal (GI) symptoms have been reported in up to 60% of these patients 1-3. One of the GI manifestations of COVID-19 infection is ischemic colitis (IC), a condition resulting from a decreased blood supply to the colon leading to mucosal injury, cellular ischemia and necrosis. The hypercoagulable state observed in COVID-19 could be related to the high inflammatory state associated with a “cytokine storm”[3]. Systemic endothelial damage and consequent disseminated microvascular thrombosis might act as a primer for many organs’ damage, including the GI tract, where the vasoconstriction and microthrombi may lead to ischaemia. In the literature, SARS-CoV-2- induced IC has been reported in only few case reports so far [4], in none detected by IUS.
CLINICAL PERSPECTIVE
The typical clinical presentation of IC is cramping, mild, left lower abdominal pain associated with an urgent desire to defecate, rectal bleeding or bloody diarrhea, nausea and/or vomiting. Pain typically precedes bleeding, and abdominal tenderness is usually present. The “watershed” areas of the colon (rectosigmoid junction and splenic flexure) are particularly prone to ischemia with limited collateral blood circulation [5]. Early colonoscopy (<48 hours) with minimum insufflation is recommended in suspected cases to confirm the diagnosis.
Therapy Planning:
Most cases of IC resolve spontaneously and do not require specific therapy. Patients with significant symptoms require hospitalization. Initial medical management most commonly includes general supportive measures, bowel rest, intravenous hydration, and correction of possible precipitating conditions. Antimicrobial therapy should be considered for patients with moderate or severe disease. Surgical intervention should be considered in selected cases [5].
Outcome and Prognosis:
Most episodes of IC are benign and self-limited. Symptoms generally resolve within 2–3 days and the colon heals in 1–2 weeks. Severe injuries, may take up to 6 months to heal; however, during this time the patient is usually asymptomatic [5].
Patients with COVID-19 predominantly have respiratory symptoms, but gastrointestinal (GI) symptoms have been reported in up to 60% of these patients 1-3. One of the GI manifestations of COVID-19 infection is ischemic colitis (IC), a condition resulting from a decreased blood supply to the colon leading to mucosal injury, cellular ischemia and necrosis. The hypercoagulable state observed in COVID-19 could be related to the high inflammatory state associated with a “cytokine storm”[3]. Systemic endothelial damage and consequent disseminated microvascular thrombosis might act as a primer for many organs’ damage, including the GI tract, where the vasoconstriction and microthrombi may lead to ischaemia. In the literature, SARS-CoV-2- induced IC has been reported in only few case reports so far [4], in none detected by IUS.
CLINICAL PERSPECTIVE
The typical clinical presentation of IC is cramping, mild, left lower abdominal pain associated with an urgent desire to defecate, rectal bleeding or bloody diarrhea, nausea and/or vomiting. Pain typically precedes bleeding, and abdominal tenderness is usually present. The “watershed” areas of the colon (rectosigmoid junction and splenic flexure) are particularly prone to ischemia with limited collateral blood circulation [5]. Early colonoscopy (<48 hours) with minimum insufflation is recommended in suspected cases to confirm the diagnosis.
Therapy Planning:
Most cases of IC resolve spontaneously and do not require specific therapy. Patients with significant symptoms require hospitalization. Initial medical management most commonly includes general supportive measures, bowel rest, intravenous hydration, and correction of possible precipitating conditions. Antimicrobial therapy should be considered for patients with moderate or severe disease. Surgical intervention should be considered in selected cases [5].
Outcome and Prognosis:
Most episodes of IC are benign and self-limited. Symptoms generally resolve within 2–3 days and the colon heals in 1–2 weeks. Severe injuries, may take up to 6 months to heal; however, during this time the patient is usually asymptomatic [5].
5Teaching Points
Ischemic colitis is a rare manifestation of COVID-19. Since IUS is a primary diagnostic tool, alternative to CT, in acute setting, IC should be suspected in patients presenting with wall thickening of a long left colon segment, particularly if with barely visible or no color Doppler signal. The main differential diagnoses of IC at IUS include neoplasm, inflammation and infection. Early colonoscopy (<48 hours) with minimum insufflation may be recommended in suspected selected cases. The early disappearance of bowel wall thickening at IUS corroborates the diagnosis excluding a chronic inflammatory bowel disease.
6References
1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223): 497-506.
2. D’Amico F, Baumgart DC, Danese S, Peyrin-Biroulet L. Diarrhea during COVID-19 infection: pathogenesis, epidemiology, prevention, and management. Clin Gastroenterol Hepatol. 2020; 18(8): 1663-1672.
3. Panigada M, Bottino N, Tagliabue P, et al. Hypercoagulability of COVID-19 patients in intensive care unit. A report of thromboelastography findings and other parameters of hemostasis. [published online ahead of print, 2020 Apr 17] J Thromb Haemost. 2020.
4. Uhlenhopp DJ, Ramachandran R, Then E, Parvataneni S, et al. COVID-19-associated ischemic colitis: A rare manifestation of COVID-19 infection—Case report and review. Journal of Investigative Medicine High Impact Case Reports 2021; 10: 1–6.
5. Brandt LJ, Feuerstadt P, Longstreth GF, Boley SJ, American College of Gastroenterology. ACG clinical guideline: epidemiology, risk factors, patterns of presentation, diagnosis, and management of colon ischemia (CI). Am J Gastroenterol. 2015; 110 (1): 18–45.
2. D’Amico F, Baumgart DC, Danese S, Peyrin-Biroulet L. Diarrhea during COVID-19 infection: pathogenesis, epidemiology, prevention, and management. Clin Gastroenterol Hepatol. 2020; 18(8): 1663-1672.
3. Panigada M, Bottino N, Tagliabue P, et al. Hypercoagulability of COVID-19 patients in intensive care unit. A report of thromboelastography findings and other parameters of hemostasis. [published online ahead of print, 2020 Apr 17] J Thromb Haemost. 2020.
4. Uhlenhopp DJ, Ramachandran R, Then E, Parvataneni S, et al. COVID-19-associated ischemic colitis: A rare manifestation of COVID-19 infection—Case report and review. Journal of Investigative Medicine High Impact Case Reports 2021; 10: 1–6.
5. Brandt LJ, Feuerstadt P, Longstreth GF, Boley SJ, American College of Gastroenterology. ACG clinical guideline: epidemiology, risk factors, patterns of presentation, diagnosis, and management of colon ischemia (CI). Am J Gastroenterol. 2015; 110 (1): 18–45.