Ischemic Colitis as Complication of SARS-CoV-2 Infection [June 2022]
July 4, 2022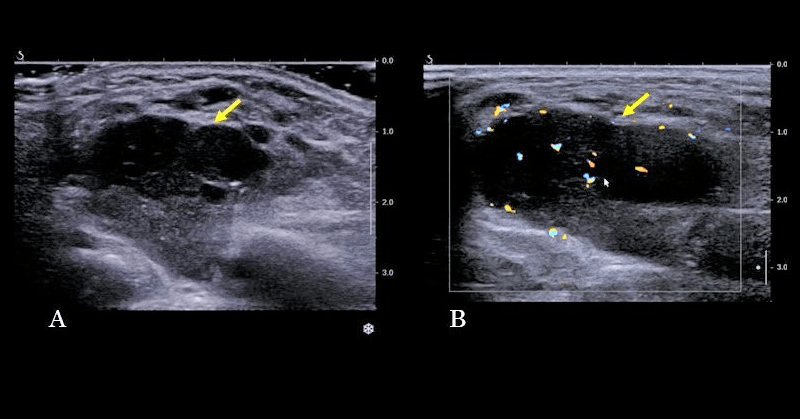
MALT Lymphoma developed on a Sjogren Syndrome [Aug 2022]
October 31, 2022Sonographic Diagnosis of a Pott’s Puffy Tumor in a 5-year-old-girl
AUTHORS
M. Brandt [1]
K. Schebesch [2]
T Araceli [2]
E. Kuhn [3]
Ch. Bohr [1]
J. Künzel [1]
[1] Department of Otorhinolaryngology, Head and Neck Surgery, University Hospital of Regensburg, Germany
[2] Department for Neurosurgery, University Hospital of Regensburg, Germany
[3] Department of Pediatrics, University Hospital of Regensburg, Germany
M. Brandt [1]
K. Schebesch [2]
T Araceli [2]
E. Kuhn [3]
Ch. Bohr [1]
J. Künzel [1]
[1] Department of Otorhinolaryngology, Head and Neck Surgery, University Hospital of Regensburg, Germany
[2] Department for Neurosurgery, University Hospital of Regensburg, Germany
[3] Department of Pediatrics, University Hospital of Regensburg, Germany
1Clinical History
A 5-year-old girl was referred to our ENT-Department with an expanding fluctuant and tender swelling of the forehead and a left-dominant eyelid swelling (Figure 1). Her main complaint was an increasing headache and deterioration in general condition, accompanied by fever. There was no history of trauma.
Taking her history showed that the patient had had an upper-airway infection four weeks ago. About two weeks later she already has been admitted to a pediatric ward with a non-tender swelling of the forehead, headache and fever. There she has been seen by an otolaryngologist, who suspected a frontal sinusitis. Therefore, the girl was treated with intravenous amoxicillin for three days, decongestant and antipyretic. The symptoms were declining, but the swelling didn’t disappear completely after discharge. After one week at home, symptoms reoccurred.
Physical examination revealed a doughy, tender swelling located in the center of the forehead. Both eyelids were swollen, but the eye motility and vision wasn’t affected. The left side of the nose wasn’t possible to be seen completely due to a septum deviation, but so far no pus or polyps were detected.
Laboratory results showed an elevated C-reactive protein (CRP) level of 44.1 mg/l (normal range: 0.0–5.0 mg/l) and white blood cells (WBC) of 16.36/nl (normal range: 5–14.5).
Taking her history showed that the patient had had an upper-airway infection four weeks ago. About two weeks later she already has been admitted to a pediatric ward with a non-tender swelling of the forehead, headache and fever. There she has been seen by an otolaryngologist, who suspected a frontal sinusitis. Therefore, the girl was treated with intravenous amoxicillin for three days, decongestant and antipyretic. The symptoms were declining, but the swelling didn’t disappear completely after discharge. After one week at home, symptoms reoccurred.
Physical examination revealed a doughy, tender swelling located in the center of the forehead. Both eyelids were swollen, but the eye motility and vision wasn’t affected. The left side of the nose wasn’t possible to be seen completely due to a septum deviation, but so far no pus or polyps were detected.
Laboratory results showed an elevated C-reactive protein (CRP) level of 44.1 mg/l (normal range: 0.0–5.0 mg/l) and white blood cells (WBC) of 16.36/nl (normal range: 5–14.5).
2Image findings
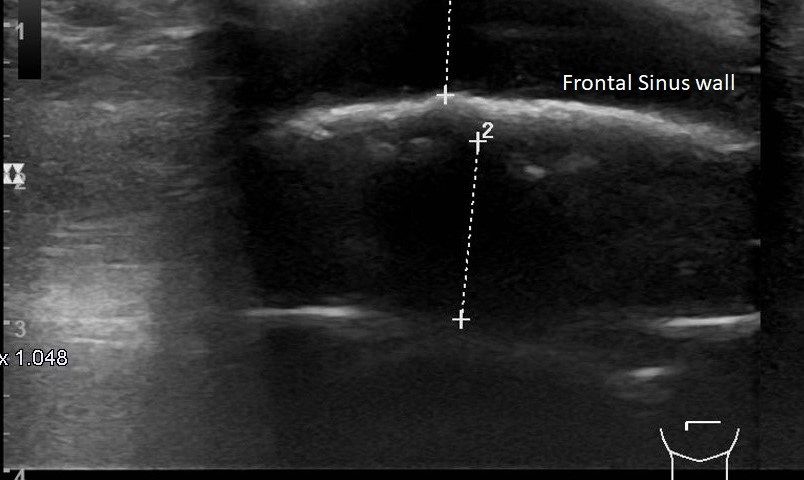
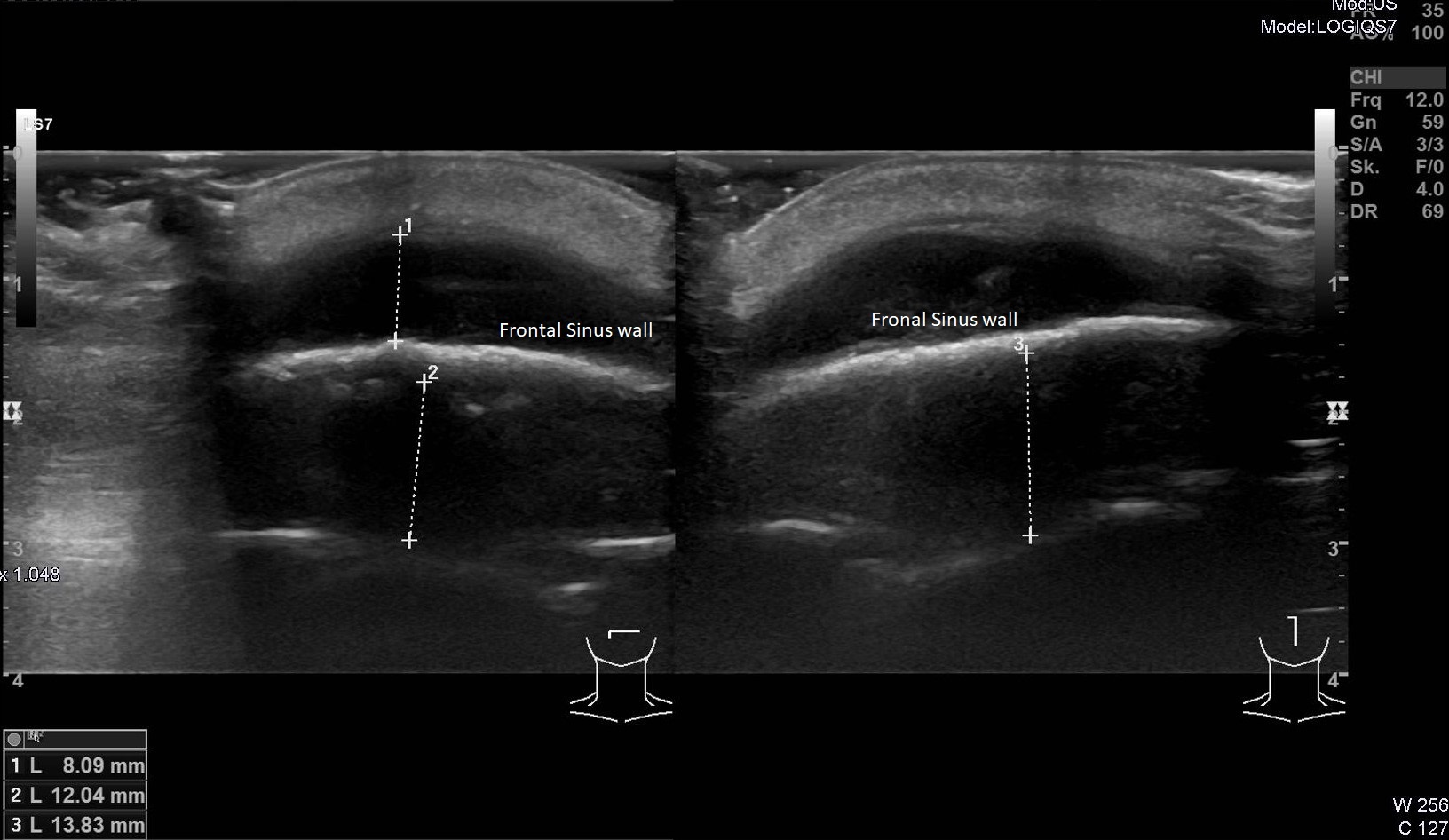
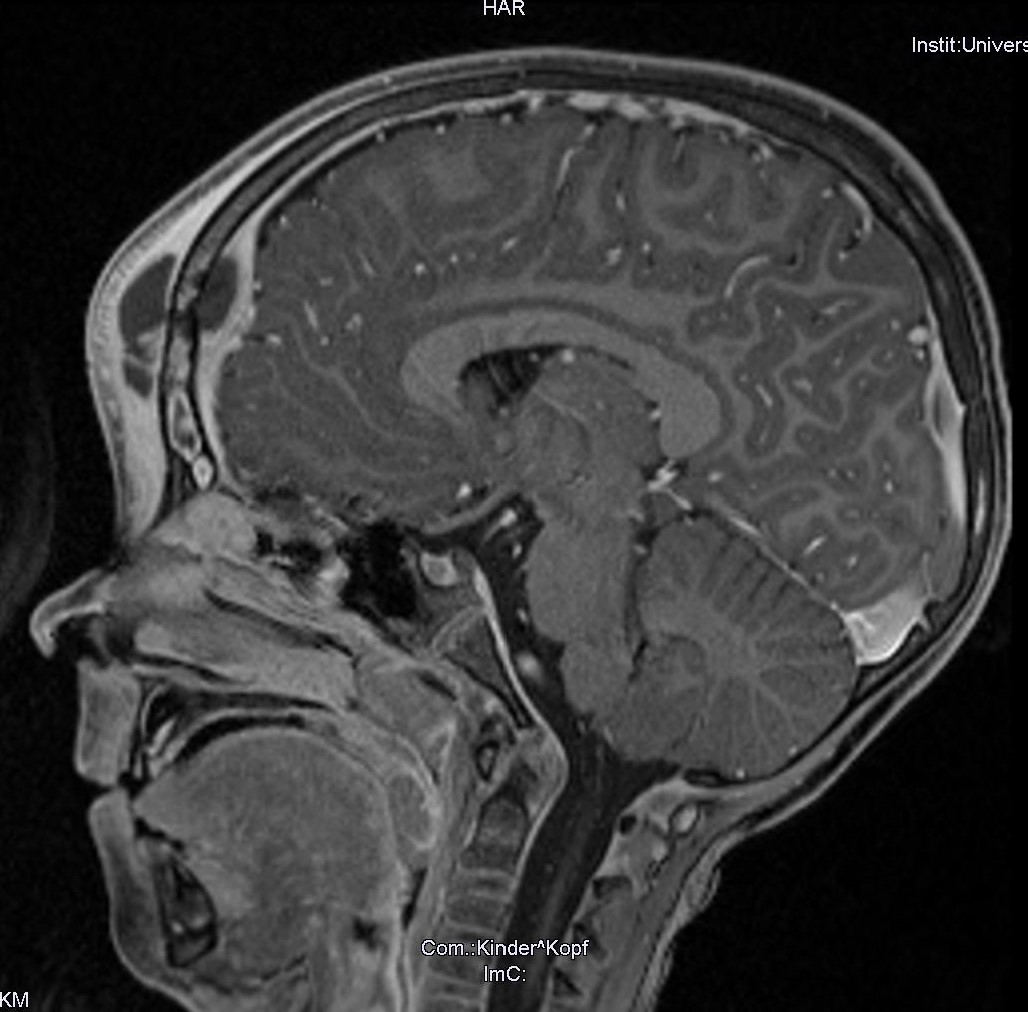
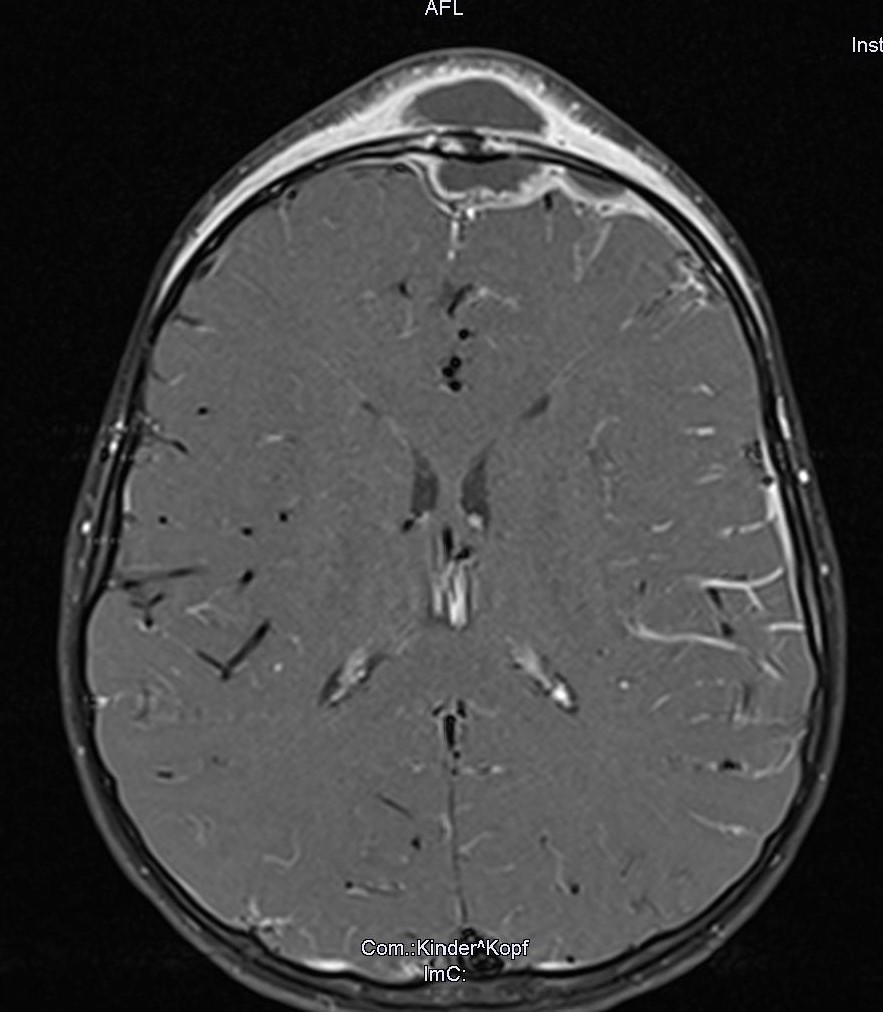
An ultrasound of the forehead revealed a hypoechoic mass, with thickening of the overlying tissue toward the skin. As far as the investigator could evaluate, the underlying bone was intact without any defect of the corticalis. However, another liquid hypoechoic mass was present posterior to the frontal bone (Figure 2). On suspicion of a Pott’s puffy tumor with intracranial complications, a MRI scan was initiated immediately. The scan confirmed our ultrasound findings. It showed a liquid subgaleal abscess accompanied by an osteomyelitis of the frontal bone. In addition, there was a bone erosion with an epidural empyema underneath, that was in contact to the superior sagittal sinus (Figure 3 and 4).
The girl was admitted to our clinic. We started an intravenous antibiotic (ceftriaxone) and analgesic. Due to the extension of cerebral complications, the patient underwent an emergency surgery by otorhinolaryngology and neurosurgery at the same session:
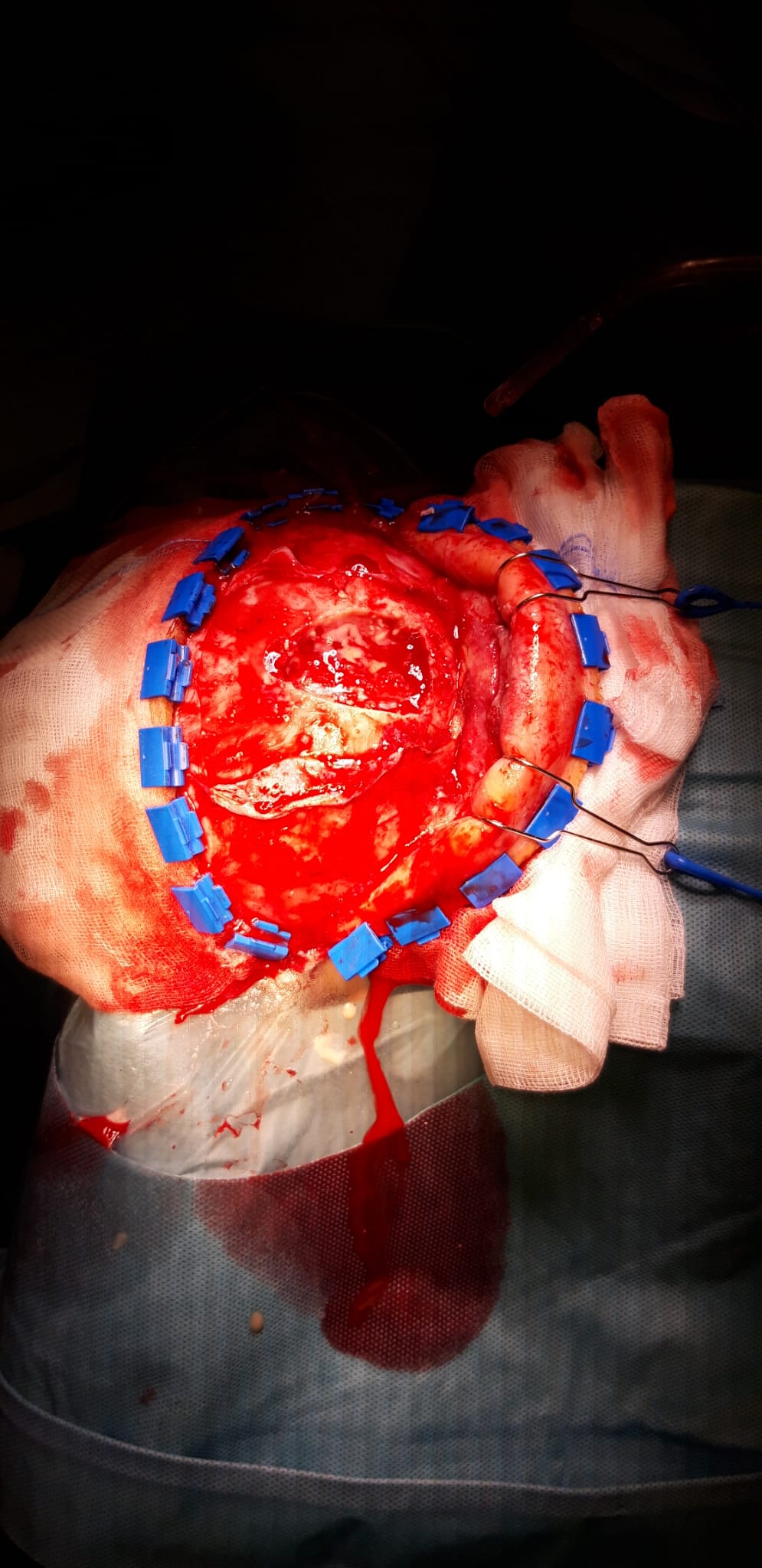
The neurosurgeons started the operation with the preparation of a bicoronal flap for craniofacial access. Here they opened and drained an encapsulated subgaleal abscess. A bifrontal craniotomy was performed to drain the epidural empyema (Figure 5) .The otolaryngologist completed the drainage of the Pott’s puffy tumor by an anterior ethmoidectomy and clearing of agger nasi cells within the frontal recess. Moreover, enlarged adenoids were found and removed.
The microbiological result of the intraoperatively taken smears showed an infection with streptococcus anginosus.
We continued the intravenous antibiotic for two weeks in the hospital and prescribed an oral therapy with cotrimoxazole for four more weeks. The patient had a good recovery and was discharged without further complications. Since this case is a very recent one, there is no longer follow-up result that we can report of.
The girl was admitted to our clinic. We started an intravenous antibiotic (ceftriaxone) and analgesic. Due to the extension of cerebral complications, the patient underwent an emergency surgery by otorhinolaryngology and neurosurgery at the same session:
The neurosurgeons started the operation with the preparation of a bicoronal flap for craniofacial access. Here they opened and drained an encapsulated subgaleal abscess. A bifrontal craniotomy was performed to drain the epidural empyema (Figure 5) .The otolaryngologist completed the drainage of the Pott’s puffy tumor by an anterior ethmoidectomy and clearing of agger nasi cells within the frontal recess. Moreover, enlarged adenoids were found and removed.
The microbiological result of the intraoperatively taken smears showed an infection with streptococcus anginosus.
We continued the intravenous antibiotic for two weeks in the hospital and prescribed an oral therapy with cotrimoxazole for four more weeks. The patient had a good recovery and was discharged without further complications. Since this case is a very recent one, there is no longer follow-up result that we can report of.
3Diagnosis
Pott’s puffy tumor (PPT) with epidural empyema.
4Discussion
BACKGROUND
PPT is a rare medical condition defined by a subperiosteal abscess of the anterior wall of the frontal sinus accompanied by an underlying frontal osteomyelitis (1). The most common etiology is an acute frontal sinusitis or infected frontal sinus mucocele, but can also occur as a result of a head trauma, acupuncture, insect bite, intranasal cocaine use, fungal infection or prior cranioplasty (2, 3).
This clinical entity has been found in all ages, although it is more often seen in adolescents. This is most likely the result of a higher flow rate of the diploic veins in that age group. It is less common and there are only few reports of patients under the age of ten, since the frontal sinuses can often not be visualised radiographically before the age of six (4).
The causative bacteria are similar to those in acute bacterial rhinosinusitis. The most frequent ones which were also found in our case are streptococcus species. Others could be staphylococcus sp., anaerobes and hemophilus influenzae (5).
CLINICAL PERSPECTIVE
The clinical presentation includes fluctuant swelling of the forehead, headache, periorbital edema and fever (6). Differential diagnosis are neoplasms, skin and soft-tissue infections, and infected hematoma.
Therapy Planning:
This case report is a good example to show that conservative therapy only is not a sufficient treatment. To prevent patients from complications, they need a rapid surgical drainage and a long-term antibiotic (7).
Outcome and Prognosis:
Without an adequate treatment a PPT can have severe sequelae like an epidural or subdural empyema, meningitis, cerebritis, brain abscess, and cavernous or superior sagittal sinus thrombosis (8).
The overall prognosis is often good. A recent review of the literature showed a mortality rate of 3.7% (9). Long-term consequences, like residual neurological deficits such as epileptic seizures, aphasia or paralysis are rarely seen (7).
PPT is a rare medical condition defined by a subperiosteal abscess of the anterior wall of the frontal sinus accompanied by an underlying frontal osteomyelitis (1). The most common etiology is an acute frontal sinusitis or infected frontal sinus mucocele, but can also occur as a result of a head trauma, acupuncture, insect bite, intranasal cocaine use, fungal infection or prior cranioplasty (2, 3).
This clinical entity has been found in all ages, although it is more often seen in adolescents. This is most likely the result of a higher flow rate of the diploic veins in that age group. It is less common and there are only few reports of patients under the age of ten, since the frontal sinuses can often not be visualised radiographically before the age of six (4).
The causative bacteria are similar to those in acute bacterial rhinosinusitis. The most frequent ones which were also found in our case are streptococcus species. Others could be staphylococcus sp., anaerobes and hemophilus influenzae (5).
CLINICAL PERSPECTIVE
The clinical presentation includes fluctuant swelling of the forehead, headache, periorbital edema and fever (6). Differential diagnosis are neoplasms, skin and soft-tissue infections, and infected hematoma.
Therapy Planning:
This case report is a good example to show that conservative therapy only is not a sufficient treatment. To prevent patients from complications, they need a rapid surgical drainage and a long-term antibiotic (7).
Outcome and Prognosis:
Without an adequate treatment a PPT can have severe sequelae like an epidural or subdural empyema, meningitis, cerebritis, brain abscess, and cavernous or superior sagittal sinus thrombosis (8).
The overall prognosis is often good. A recent review of the literature showed a mortality rate of 3.7% (9). Long-term consequences, like residual neurological deficits such as epileptic seizures, aphasia or paralysis are rarely seen (7).
5Teaching Points
PPTs are an uncommon presentation, especially in younger children and might be inconclusive in clinical findings. A delayed diagnosis or insufficient conservative treatment can cause life-threatening complications. Therefore, ultrasound plays a crucial role in the first line clinical investigation especially in children to identify this condition. It is an easily accessible, harmless device that can also prevent paediatric patients from radiation through a CT-scan (10).
6CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
7References
1. Flamm ES. Percivall Pott: an 18th century neurosurgeon. J Neurosurg 1992; 76:319–326.
2. Blackshaw G, Thomson N. Pott's puffy tumour reviewed. J Laryngol Otol. 1990; 104: 574–7.
3. Akiyama K, Karaki M, Mori N. Evaluation of adult Pott's puffy tumor: our five cases and 27 literature cases. Laryngoscope. 2012; 122: 2382-8.
4. Moore K, Ross A. Frontal sinus development and juvenile age estimation. Anat Rec (Hoboken). 2017; 300: 1609-1617.
5. Forgie SE, Marrie TJ. Pott’s puffy tumor. Am. J. Med. 2008; 121: 1041–2.
6. Kalkan H, Eryılmaz MA, Kıresi D, Arbag H, Yesildag A. Pott's Puffy tumor: The role of ultrasound, computed tomography and magnetic resonance imaging in diagnosis. Eur J Gen Med. 2017; 14: 51-3.
7. Koltsidopoulos P, Papageorgiou E, Skoulakis C. Pott's puffy tumor in children: A review of the literature. Laryngoscope. 2020; 130: 225-231.
8. Blumfield E, Misra M. Pott’s puffy tumor, intracranial, and orbital complications as the initial presentation of sinusitis in healthy adolescents, a case series. Emerg Radiol 2011; 18: 203–210.
9. Tsai BY, Lin KL, Lin TY, et al. Pott’s puffy tumor in children. Childs Nerv Syst 2010; 26: 53–60.
10. Reddan T, Connor P. Not just a bump on the head: ultrasound as first-line imaging in a boy with Pott's puffy tumour. J Med Radiat Sci. 2018; 65: 71-73.
2. Blackshaw G, Thomson N. Pott's puffy tumour reviewed. J Laryngol Otol. 1990; 104: 574–7.
3. Akiyama K, Karaki M, Mori N. Evaluation of adult Pott's puffy tumor: our five cases and 27 literature cases. Laryngoscope. 2012; 122: 2382-8.
4. Moore K, Ross A. Frontal sinus development and juvenile age estimation. Anat Rec (Hoboken). 2017; 300: 1609-1617.
5. Forgie SE, Marrie TJ. Pott’s puffy tumor. Am. J. Med. 2008; 121: 1041–2.
6. Kalkan H, Eryılmaz MA, Kıresi D, Arbag H, Yesildag A. Pott's Puffy tumor: The role of ultrasound, computed tomography and magnetic resonance imaging in diagnosis. Eur J Gen Med. 2017; 14: 51-3.
7. Koltsidopoulos P, Papageorgiou E, Skoulakis C. Pott's puffy tumor in children: A review of the literature. Laryngoscope. 2020; 130: 225-231.
8. Blumfield E, Misra M. Pott’s puffy tumor, intracranial, and orbital complications as the initial presentation of sinusitis in healthy adolescents, a case series. Emerg Radiol 2011; 18: 203–210.
9. Tsai BY, Lin KL, Lin TY, et al. Pott’s puffy tumor in children. Childs Nerv Syst 2010; 26: 53–60.
10. Reddan T, Connor P. Not just a bump on the head: ultrasound as first-line imaging in a boy with Pott's puffy tumour. J Med Radiat Sci. 2018; 65: 71-73.