Contrast Enhanced Ultrasound (CEUS)
May 9, 2018
Myotendinous rupture of the distal biceps [Jun 2018]
June 13, 2018Epiploic Appendagitis or Localised Omental Infarct?
Christoph F Dietrich, Yi Dong, Ulrich Baum, Uwe Gottschalk
Correspondence: Prof. Dr. med. Christoph F. Dietrich, Medizinische Klinik 2, Caritas-Krankenhaus, Uhlandstr. 7, 97980 Bad Mergentheim, Tel:+49 7931 58 2201, Email: christoph.dietrich@ckbm.de
Correspondence: Prof. Dr. med. Christoph F. Dietrich, Medizinische Klinik 2, Caritas-Krankenhaus, Uhlandstr. 7, 97980 Bad Mergentheim, Tel:+49 7931 58 2201, Email: christoph.dietrich@ckbm.de
1Case Report
A 45-year-old female presents with acute abdominal pain localised to the right upper abdo-men. Ultrasound delineated a mass of 50 x 45 x 30 mm at the site of tenderness. The appar-ent mass was of fat texture but appeared inflamed. The lesion was neither fixed to the colon nor to the parietal peritoneum during inspiration and expiration. Computed tomography showed features of an appendagitis and a focal segment of infarcted mesentery. The patient´s symptoms responded to therapy with non-steroidal anti-inflammatory agents, which were continued for six weeks.
2Discussion
Segmental or focal omental infarction with or without mesenteritis is a rare, benign, and acute and sometimes chronic fibrosing inflammation disease of the mesenteric fatty tissue. The pathophysiological process may be similar to that of epiploic appendagitis [(1-5)], with the infarcted fatty tissue being part of the omentum. It can occur at any age but most com-monly in the fifth decades with a mean age at diagnosis of about 40 years similar to epiploic appendagitis [(6-8)].
3Etiology and pathophysiology
Its etiology is unknown. Predisposing factors have been described including congenital abnor-malities of the omentum, focal inflammation with or without thrombosis, in association with neoplasia, after interventions including laparotomy with damage of blood vessels and after strenuous exercise [(6, 9)]. In addition obesity, trauma and other factors have been discussed. Partial omental infarction is a complication of omental transection while performing the an-tecolic approach to the laparoscopic Roux-en-Y gastric bypass.
It can result from the following predisposing factors: structural anomalies in the omentum and its veins (particularly of the right side), thrombophilia, circulatory insufficiency and vascu-litis as well as obesity, cough, excessive physical exertion and an abrupt change of the position of the torso [(10)]. The secondary nature of this pathology is a consequence of abdominal surgery, trauma, inflammation, presence of a cyst and abdominal hernia. In these cases, lesions can be located at various sites in the abdominal cavity [(11, 12)].
4Location
To our experience it can occur at any location of the omentum but the right upper abdominal regions are more often involved compared to the left lower side, which is typical for diverticu-litis and epiploic appendagitis (which can occur left or right sided) [(13, 14)].
5Clinical presentation and symptoms
The symptoms and imaging features are similar to epiploic appendagitis [(15)] with acute or subacute upper (mid) abdominal pain and variably rebound tenderness and palpable mass (both up to 30 %) using physical examination [(16-18)]. Typically ultrasound supports physical examination with more frequently observed rebound tenderness and palpable masses. The right and left lower abdomen is a typical location for appendagitis. Less frequently observed symptoms include fever, vomiting, diarrhea or constipation. The white blood cell count, eryth-rocyte sedimentation rate, and C-reactive protein are mildly elevated or normal [(9, 19)]. The differential diagnosis of segmental or focal omental infarction include epiploic appendagitis, acute diverticulitis and acute appendicitis and many other inflammatory gastrointestinal dis-eases [(20-26)].
6Imaging findings
Transabdominal ultrasound typically shows a focal solid and non-compressible, solid, hy-perechoic ovoid lesion sometimes with a peripherally located hypoechoic (inflammatory) rim [(1-3, 9)]. A typical ultrasound image of omental infarction is characterized by: a slightly or moderately hyperechoic plaque-like mass greater than 35 - 50 mm located under the ab-dominal integuments to the right of the navel. Appendagitis tends to be smaller. The mass is sensitive to compression but with no visible compressibility [(10)]. Sometimes, the lesion is surrounded with a hypoechoic rim, or slight amounts of fluid are found in the vicinity. Colour Doppler Imaging (CDI) typically reveals absence of blood flow in the mass lesion similar to appendagitis and other ischemic diseases [(15, 27-30)] but contrast enhanced ultrasound is much more sensitive [(26, 31-39)]. However, vessels on the periphery of a central hypoechoic necrotic area have been observed in children with this pathology [(10)]. The pathological mass gives a similar US image to that of necrotic fat tissue at other abdominal sites. Most often isoechoic to the surrounding tissue the appearance varies from slightly hyperechoic to more often centrally located hypoechogenicity [(15, 40, 41)]. The echogenicity depends on the in-flammatory process and inflammatory vessels or infarct. It is typically iso- or hyperechoic, non-vascularized, sensitive and shows no compressibility [(11)]. Strain elastography and shear wave elastography [(42-51)] may reveal stiffer tissue than the surrounding. Ultrasound typi-cally shows an oval shaped and non-compressible painful mass directly under the abdominal wall.
Magnetic resonance imaging (MRI) findings may be similar to the described CT findings [(52)].
7Differential diagnosis
Omental infarction should be part of the differential diagnosis, including anastomotic leak, in patients who develop abdominal pain 3-4 days after laparoscopic Roux-en-Y gastric bypass [(53)]. In approximately 90% of cases, the site of primary infarction (torsion) of the greater omentum is the right side. It can be mistaken for an exophytic tumor of the pancreas [(54)]. Omental infarction should be considered as a differential diagnosis for acute right-sided ab-dominal pain, especially in obese children [(55)]. In the absence of inflammation imaging is more difficult. In contrast epiploic appendagitis is a 20 to 30 mm, oval-shaped, fat density,
paracolic mass with thickened peritoneal lining and peri-appendageal stranding [(9, 28, 56-61)]. Appendagitis often shows an inflammatory perilesional inflammatory reaction, which is less pronounced in omental infarction. The course of the disease is more prolonged in omental infarction compared to appendagitis as shown in our case. However, since both enti-ties present with the same symptoms, clinical and imaging findings and both are treated by symptomatic anti-inflammatory devices the differential diagnosis has no practical conse-quence [(9, 62-65)]. This is mainly true due to the benign course of the diseases.
Infarction of the lesser omentum is rare and a diagnostic challenge. The clinical picture of this pathology, including its spontaneous resolution, resembles infarction of the greater omentum. The only difference is the site, i.e. the position of a lesion between the left liver lobe, pancreas and stomach.
Infarction of the lesser omentum is rare and a diagnostic challenge. The clinical picture of this pathology, including its spontaneous resolution, resembles infarction of the greater omentum. The only difference is the site, i.e. the position of a lesion between the left liver lobe, pancreas and stomach.
8Treatment
Because infarction of the greater omentum clinically resembles appendagitis and appendici-tis, its assessment is very important from the point of view of adequate patient management since the thickened omentum can at times conceal an underlying pathology. In the considera-ble majority of cases, omental infarction resolves spontaneously without specific treatment [(10)]. Inaccurate diagnosis can lead to unnecessary hospitalizations, antibiotic therapy, and surgical intervention [(56, 57, 66-69)]. If the disease is diagnosed in an ambulatory setting they usually do not require hospitalization, antibiotics [(70)] or surgery [(71)]. Surgery should be omitted whenever possible but intestinal obstruction and intussusception have been de-scribe in similar diseases [(71)].
9Conclusion
In conclusion, local omental infarct with or without inflammatory changes is a benign and self-limiting condition. Complete resolution without surgical intervention usually occurs within weeks. The time to recover is generally longer than in an appendagitis [(9, 29, 62, 63)]. The lesion undergoes involution, mainly with fibrosis, sometimes with calcifications or adhesions between adjacent tissues. At times, a necrotic fragment detaches to the peritoneal cavity and behaves as a loose body [(10, 72)]. The risk of recurrence is probably low. Complications in-cluding abscess formation have been described, especially after surgery [(72)].
10References
1. Dietrich CF, Lembcke B, Jenssen C, Hocke M, Ignee A, Hollerweger A. Intestinal ultrasound in rare gastrointestinal diseases, update, part 1. Ultraschall Med 2014;35:400-421.
2. Dietrich CF, Lembcke B, Jenssen C, Hocke M, Ignee A, Hollerweger A. Intestinal Ultrasound in Rare Gastrointestinal Diseases, Update, Part 2. Ultraschall Med 2015;36:428-456.
3. Dietrich CF, Brunner V, Lembcke B. [Intestinal ultrasound in rare small and large intestinal diseases]. Z.Gastroenterol. 1998;36:955-970.
4. Pines BR, Beller J. Primary torsion and infarction of the appendices epiploicae. Arch Surg 1941;42:775.
5. Dockerty MB, Lynn TE, Waugh JM. A clinicopathologic study of the epiploic appendages. Surg Gynecol Obstet 1956;103:423.
6. Schnedl WJ, Krause R, Tafeit E, Tillich M, Lipp RW, Wallner-Liebmann SJ. Insights into epiploic appendagitis. Nat Rev Gastroenterol Hepatol 2011;8:45-49.
7. Ozdemir S, Gulpinar K, Leventoglu S, Uslu HY, Turkoz E, Ozcay N, Korkmaz A. Torsion of the primary epiploic appendagitis: a case series and review of the literature. Am J Surg 2010;199:453-458.
8. Sand M, Gelos M, Bechara FG, Sand D, Wiese TH, Steinstraesser L, Mann B. Epiploic appendagitis--clinical characteristics of an uncommon surgical diagnosis. BMC Surg 2007;7:11.
9. Rioux M, Langis P. Primary epiploic appendagitis: clinical, US, and CT findings in 14 cases. Radiology 1994;191:523-526.
10. Smereczynski A, Kolaczyk K, Bernatowicz E. Intra-abdominal fat. Part II: Non-cancerous lesions of the adipose tissue localized beyond organs. J Ultrason 2016;16:32-43.
11. Coulier B. Contribution of US and CT for diagnosis of intraperitoneal focal fat infarction (IFFI): a pictorial review. JBR-BTR 2010;93:171-185.
12. Kamaya A, Federle MP, Desser TS. Imaging manifestations of abdominal fat necrosis and its mimics. Radiographics 2011;31:2021-2034.
13. Atkinson NSS, Bryant RV, Dong Y, Maaser C, Kucharzik T, Maconi G, Asthana AK, et al. How to perform gastrointestinal ultrasound: Anatomy and normal findings. World J Gastroenterol 2017;23:6931-6941.
14. Atkinson NS, Bryant RV, Dong Y, Maaser C, Kucharzik T, Maconi G, Asthana AK, et al. WFUMB Position Paper. Learning Gastrointestinal Ultrasound: Theory and Practice. Ultrasound Med Biol 2016;42:2732-2742.
15. van Breda Vriesman AC, Puylaert JB. Epiploic appendagitis and omental infarction: pitfalls and look-alikes. Abdom Imaging 2002;27:20-28.
16. Sandrasegaran K, Maglinte DD, Rajesh A, Akisik FM. Primary epiploic appendagitis: CT diagnosis. Emerg Radiol 2004;11:9-14.
17. McGeer PL, McKenzie AD. Strangulation of the appendix epiploica: A series of 11 cases. Can J Surg 1960;3:252.
18. Shehan JJ, Organ C, Sullivan JF. Infarction of the appendices epiploicae. Am J Gastroenterol 1966;46:469-476.
19. Carmichael DH, Organ CH, Jr. Epiploic disorders. Conditions of the epiploic appendages. Arch Surg 1985;120:1167-1172.
20. Dietrich CF, Goudie A, Chiorean L, Cui XW, Gilja OH, Dong Y, Abramowicz JS, et al. Point of Care Ultrasound: A WFUMB Position Paper. Ultrasound Med Biol 2017;43:49-58.
21. Chiorean L, Barr RG, Braden B, Jenssen C, Cui XW, Hocke M, Schuler A, et al. Transcutaneous Ultrasound: Elastographic Lymph Node Evaluation. Current Clinical Applications and Literature Review. Ultrasound Med Biol 2016;42:16-30.
22. Chiorean L, Cui XW, Klein SA, Budjan J, Sparchez Z, Radzina M, Jenssen C, et al. Clinical value of imaging for lymph nodes evaluation with particular emphasis on ultrasonography. Z Gastroenterol 2016;54:774-790.
23. Schreiber-Dietrich D, Chiorean L, Cui XW, Braden B, Kucharzik T, Jungert J, Kosiak W, et al. Particularities of Crohn's disease in pediatric patients: current status and perspectives regarding imaging modalities. Expert Rev Gastroenterol Hepatol 2015;9:1313-1325.
24. Dietrich CF, Jenssen C, Arcidiacono PG, Cui XW, Giovannini M, Hocke M, Iglesias-Garcia J, et al. Endoscopic ultrasound: Elastographic lymph node evaluation. Endosc Ultrasound 2015;4:176-190.
25. Chiorean L, Schreiber-Dietrich D, Braden B, Cui XW, Buchhorn R, Chang JM, Dietrich CF. Ultrasonographic imaging of inflammatory bowel disease in pediatric patients. World J Gastroenterol 2015;21:5231-5241.
26. Chiorean L, Schreiber-Dietrich D, Braden B, Cui X, Dietrich CF. Transabdominal ultrasound for standardized measurement of bowel wall thickness in normal children and those with Crohn's disease. Med Ultrason 2014;16:319-324.
27. Dietrich CF, Jedrzejczyk M, Ignee A. Sonographic assessment of splanchnic arteries and the bowel wall. Eur.J.Radiol. 2007;64:202-212.
28. Deceuninck A, Danse E. Primary epiploic appendagitis: US and CT findings. JBR-BTR 2006;89:225.
29. Lee YC, Wang HP, Huang SP, Chen YF, Wu MS, Lin JT. Gray-scale and color Doppler sonographic diagnosis of epiploic appendagitis. J Clin Ultrasound 2001;29:197-199.
30. Danse EM, Van Beers BE, Baudrez V, Pauls C, Baudrez Y, Kartheuser A, Thys F, et al. Epiploic appendagitis: color Doppler sonographic findings. Eur Radiol 2001;11:183-186.
31. Dietrich CF, Averkiou M, Nielsen MB, Barr RG, Burns PN, Calliada F, Cantisani V, et al. How to perform Contrast-Enhanced Ultrasound (CEUS). Ultrasound Int Open 2018;4:E2-E15.
32. Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsoe CP, Piscaglia F, et al. Guidelines and good clinical practice recommendations for Contrast Enhanced Ultrasound (CEUS) in the liver - update 2012: A WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultrasound Med Biol 2013;39:187-210.
33. Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsoe CP, Piscaglia F, et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver--update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultraschall Med 2013;34:11-29.
34. Piscaglia F, Nolsoe C, Dietrich CF, Cosgrove DO, Gilja OH, Bachmann NM, Albrecht T, et al. The EFSUMB Guidelines and Recommendations on the Clinical Practice of Contrast Enhanced Ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med. 2012;33:33-59.
35. Claudon M, Cosgrove D, Albrecht T, Bolondi L, Bosio M, Calliada F, Correas JM, et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) - update 2008. Ultraschall Med 2008;29:28-44.
36. Nylund K, Maconi G, Hollerweger A, Ripolles T, Pallotta N, Higginson A, Serra C, et al. EFSUMB Recommendations and Guidelines for Gastrointestinal Ultrasound. Ultraschall Med 2017;38:e1-e15.
37. Nylund K, Maconi G, Hollerweger A, Ripolles T, Pallotta N, Higginson A, Serra C, et al. EFSUMB Recommendations and Guidelines for Gastrointestinal Ultrasound - Part 1: Examination Techniques and Normal Findings (Long version). Ultraschall Med 2016.
38. Allgayer H, Braden B, Dietrich CF. Transabdominal ultrasound in inflammatory bowel disease. Conventional and recently developed techniques--update. Med.Ultrason. 2011;13:302-313.
39. Gorg C, Egbring J, Bert T. Contrast-enhanced ultrasound of epiploic appendagitis. Ultraschall Med 2009;30:163-167.
40. Puylaert JB. Right-sided segmental infarction of the omentum: clinical, US, and CT findings. Radiology 1992;185:169-172.
41. Miguel A, Ripollés T, Martínez MJ. Apendicitis epiploica e infarto omental: hallazgos en ecografía y tomografía computarizada. Radiología 2001;43:395-401.
42. Shiina T, Nightingale KR, Palmeri ML, Hall TJ, Bamber JC, Barr RG, Castera L, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 1: basic principles and terminology. Ultrasound Med Biol 2015;41:1126-1147.
43. Ferraioli G, Filice C, Castera L, Choi BI, Sporea I, Wilson SR, Cosgrove D, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 3: liver. Ultrasound Med Biol 2015;41:1161-1179.
44. Barr RG, Nakashima K, Amy D, Cosgrove D, Farrokh A, Schafer F, Bamber JC, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 2: breast. Ultrasound Med Biol 2015;41:1148-1160.
45. Cosgrove D, Barr R, Bojunga J, Cantisani V, Chammas MC, Dighe M, Vinayak S, et al. WFUMB Guidelines and Recommendations on the Clinical Use of Ultrasound Elastography: Part 4. Thyroid. Ultrasound Med Biol 2017;43:4-26.
46. Barr RG, Cosgrove D, Brock M, Cantisani V, Correas JM, Postema AW, Salomon G, et al. WFUMB Guidelines and Recommendations on the Clinical Use of Ultrasound Elastography: Part 5. Prostate. Ultrasound Med Biol 2017;43:27-48.
47. Trenker C, Gorg C, Jenssen C, Klein S, Neubauer A, Wagner U, Dietrich CF. [Ultrasound in oncology, current perspectives]. Z Gastroenterol 2017;55:1021-1037.
48. Dong Y, Sirli R, Ferraioli G, Sporea I, Chiorean L, Cui X, Fan M, et al. Shear wave elastography of the liver - review on normal values. Z Gastroenterol 2017;55:153-166.
49. Dietrich CF, Rudd L, Saftiou A, Gilja OH. The EFSUMB website, a great source for ultrasound information and education. Med Ultrason 2017;19:102-110.
50. Dietrich CF, Bamber J, Berzigotti A, Bota S, Cantisani V, Castera L, Cosgrove D, et al. EFSUMB Guidelines and Recommendations on the Clinical Use of Liver Ultrasound Elastography, Update 2017 (Short Version). Ultraschall Med 2017;38:377-394.
51. Dietrich CF, Bamber J, Berzigotti A, Bota S, Cantisani V, Castera L, Cosgrove D, et al. EFSUMB Guidelines and Recommendations on the Clinical Use of Liver Ultrasound Elastography, Update 2017 (Long Version). Ultraschall Med 2017;38:e16-e47.
52. Sirvanci M, Balci NC, Karaman K, Duran C, Karakas E. Primary epiploic appendagitis: MRI findings. Magn Reson Imaging 2002;20:137-139.
53. Dallal RM, Bailey LA. Omental infarction: a cause of acute abdominal pain after antecolic gastric bypass. Surg Obes Relat Dis 2006;2:451-454.
54. Kim HC, Yang DM, Jin W, Joh JH. Infarction of lesser omental fat mimicking an exophytic pancreatic tumor by sonography. J Clin Ultrasound 2011;39:412-414.
55. Tsunoda T, Sogo T, Komatsu H, Inui A, Fujisawa T. A case report of idiopathic omental infarction in an obese child. Case Rep Pediatr 2012;2012:513634.
56. Rao PM, Wittenberg J, Lawrason JN. Primary epiploic appendagitis: evolutionary changes in CT appearance. Radiology 1997;204:713-717. 57. Horton KM, Corl FM, Fishman EK. CT evaluation of the colon: inflammatory disease. Radiographics 2000;20:399-418.
58. Rao PM. CT of diverticulitis and alternative conditions. Semin Ultrasound CT MR 1999;20:86-93.
59. Singh AK, Gervais DA, Hahn PF, Rhea J, Mueller PR. CT appearance of acute appendagitis. AJR Am J Roentgenol 2004;183:1303-1307.
60. Ng KS, Tan AG, Chen KK, Wong SK, Tan HM. CT features of primary epiploic appendagitis. Eur J Radiol 2006;59:284-288.
61. Subramaniam R. Acute appendagitis: emergency presentation and computed tomographic appearances. Emerg Med J 2006;23:e53.
62. Desai HP, Tripodi J, Gold BM, Burakoff R. Infarction of an epiploic appendage. Review of the literature. J Clin Gastroenterol 1993;16:323-325.
63. Legome EL, Belton AL, Murray RE, Rao PM, Novelline RA. Epiploic appendagitis: the emergency department presentation. J Emerg Med 2002;22:9-13.
64. Legome EL, Sims C, Rao PM. Epiploic appendagitis: adding to the differential of acute abdominal pain. J Emerg Med 1999;17:823-826.
65. Vinson DR. Epiploic appendagitis: a new diagnosis for the emergency physician. Two case reports and a review. J Emerg Med 1999;17:827-832.
66. Molla E, Ripolles T, Martinez MJ, Morote V, Rosello-Sastre E. Primary epiploic appendagitis: US and CT findings. Eur Radiol 1998;8:435-438.
67. Rao PM, Rhea JT, Novelline RA, Mostafavi AA, McCabe CJ. Effect of computed tomography of the appendix on treatment of patients and use of hospital resources. N Engl J Med 1998;338:141-146.
68. Rao PM, Rhea JT, Wittenberg J, Warshaw AL. Misdiagnosis of primary epiploic appendagitis. Am J Surg 1998;176:81-85.
69. Klingenstein P. Some phases of the pathology of the appendices epiploicae. Surg Gynecol Obstet 1924;38:376.
70. Sangha S, Soto JA, Becker JM, Farraye FA. Primary epiploic appendagitis: an underappreciated diagnosis. A case series and review of the literature. Dig Dis Sci 2004;49:347-350.
71. Puppala AR, Mustafa SG, Moorman RH, Howard CH. Small bowel obstruction due to disease of epiploic appendage. Am J Gastroenterol 1981;75:382-383.
72. Balthazar EJ, Lefkowitz RA. Left-sided omental infarction with associated omental abscess: CT diagnosis. J Comput Assist Tomogr 1993;17:379-381.
2. Dietrich CF, Lembcke B, Jenssen C, Hocke M, Ignee A, Hollerweger A. Intestinal Ultrasound in Rare Gastrointestinal Diseases, Update, Part 2. Ultraschall Med 2015;36:428-456.
3. Dietrich CF, Brunner V, Lembcke B. [Intestinal ultrasound in rare small and large intestinal diseases]. Z.Gastroenterol. 1998;36:955-970.
4. Pines BR, Beller J. Primary torsion and infarction of the appendices epiploicae. Arch Surg 1941;42:775.
5. Dockerty MB, Lynn TE, Waugh JM. A clinicopathologic study of the epiploic appendages. Surg Gynecol Obstet 1956;103:423.
6. Schnedl WJ, Krause R, Tafeit E, Tillich M, Lipp RW, Wallner-Liebmann SJ. Insights into epiploic appendagitis. Nat Rev Gastroenterol Hepatol 2011;8:45-49.
7. Ozdemir S, Gulpinar K, Leventoglu S, Uslu HY, Turkoz E, Ozcay N, Korkmaz A. Torsion of the primary epiploic appendagitis: a case series and review of the literature. Am J Surg 2010;199:453-458.
8. Sand M, Gelos M, Bechara FG, Sand D, Wiese TH, Steinstraesser L, Mann B. Epiploic appendagitis--clinical characteristics of an uncommon surgical diagnosis. BMC Surg 2007;7:11.
9. Rioux M, Langis P. Primary epiploic appendagitis: clinical, US, and CT findings in 14 cases. Radiology 1994;191:523-526.
10. Smereczynski A, Kolaczyk K, Bernatowicz E. Intra-abdominal fat. Part II: Non-cancerous lesions of the adipose tissue localized beyond organs. J Ultrason 2016;16:32-43.
11. Coulier B. Contribution of US and CT for diagnosis of intraperitoneal focal fat infarction (IFFI): a pictorial review. JBR-BTR 2010;93:171-185.
12. Kamaya A, Federle MP, Desser TS. Imaging manifestations of abdominal fat necrosis and its mimics. Radiographics 2011;31:2021-2034.
13. Atkinson NSS, Bryant RV, Dong Y, Maaser C, Kucharzik T, Maconi G, Asthana AK, et al. How to perform gastrointestinal ultrasound: Anatomy and normal findings. World J Gastroenterol 2017;23:6931-6941.
14. Atkinson NS, Bryant RV, Dong Y, Maaser C, Kucharzik T, Maconi G, Asthana AK, et al. WFUMB Position Paper. Learning Gastrointestinal Ultrasound: Theory and Practice. Ultrasound Med Biol 2016;42:2732-2742.
15. van Breda Vriesman AC, Puylaert JB. Epiploic appendagitis and omental infarction: pitfalls and look-alikes. Abdom Imaging 2002;27:20-28.
16. Sandrasegaran K, Maglinte DD, Rajesh A, Akisik FM. Primary epiploic appendagitis: CT diagnosis. Emerg Radiol 2004;11:9-14.
17. McGeer PL, McKenzie AD. Strangulation of the appendix epiploica: A series of 11 cases. Can J Surg 1960;3:252.
18. Shehan JJ, Organ C, Sullivan JF. Infarction of the appendices epiploicae. Am J Gastroenterol 1966;46:469-476.
19. Carmichael DH, Organ CH, Jr. Epiploic disorders. Conditions of the epiploic appendages. Arch Surg 1985;120:1167-1172.
20. Dietrich CF, Goudie A, Chiorean L, Cui XW, Gilja OH, Dong Y, Abramowicz JS, et al. Point of Care Ultrasound: A WFUMB Position Paper. Ultrasound Med Biol 2017;43:49-58.
21. Chiorean L, Barr RG, Braden B, Jenssen C, Cui XW, Hocke M, Schuler A, et al. Transcutaneous Ultrasound: Elastographic Lymph Node Evaluation. Current Clinical Applications and Literature Review. Ultrasound Med Biol 2016;42:16-30.
22. Chiorean L, Cui XW, Klein SA, Budjan J, Sparchez Z, Radzina M, Jenssen C, et al. Clinical value of imaging for lymph nodes evaluation with particular emphasis on ultrasonography. Z Gastroenterol 2016;54:774-790.
23. Schreiber-Dietrich D, Chiorean L, Cui XW, Braden B, Kucharzik T, Jungert J, Kosiak W, et al. Particularities of Crohn's disease in pediatric patients: current status and perspectives regarding imaging modalities. Expert Rev Gastroenterol Hepatol 2015;9:1313-1325.
24. Dietrich CF, Jenssen C, Arcidiacono PG, Cui XW, Giovannini M, Hocke M, Iglesias-Garcia J, et al. Endoscopic ultrasound: Elastographic lymph node evaluation. Endosc Ultrasound 2015;4:176-190.
25. Chiorean L, Schreiber-Dietrich D, Braden B, Cui XW, Buchhorn R, Chang JM, Dietrich CF. Ultrasonographic imaging of inflammatory bowel disease in pediatric patients. World J Gastroenterol 2015;21:5231-5241.
26. Chiorean L, Schreiber-Dietrich D, Braden B, Cui X, Dietrich CF. Transabdominal ultrasound for standardized measurement of bowel wall thickness in normal children and those with Crohn's disease. Med Ultrason 2014;16:319-324.
27. Dietrich CF, Jedrzejczyk M, Ignee A. Sonographic assessment of splanchnic arteries and the bowel wall. Eur.J.Radiol. 2007;64:202-212.
28. Deceuninck A, Danse E. Primary epiploic appendagitis: US and CT findings. JBR-BTR 2006;89:225.
29. Lee YC, Wang HP, Huang SP, Chen YF, Wu MS, Lin JT. Gray-scale and color Doppler sonographic diagnosis of epiploic appendagitis. J Clin Ultrasound 2001;29:197-199.
30. Danse EM, Van Beers BE, Baudrez V, Pauls C, Baudrez Y, Kartheuser A, Thys F, et al. Epiploic appendagitis: color Doppler sonographic findings. Eur Radiol 2001;11:183-186.
31. Dietrich CF, Averkiou M, Nielsen MB, Barr RG, Burns PN, Calliada F, Cantisani V, et al. How to perform Contrast-Enhanced Ultrasound (CEUS). Ultrasound Int Open 2018;4:E2-E15.
32. Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsoe CP, Piscaglia F, et al. Guidelines and good clinical practice recommendations for Contrast Enhanced Ultrasound (CEUS) in the liver - update 2012: A WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultrasound Med Biol 2013;39:187-210.
33. Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsoe CP, Piscaglia F, et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver--update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultraschall Med 2013;34:11-29.
34. Piscaglia F, Nolsoe C, Dietrich CF, Cosgrove DO, Gilja OH, Bachmann NM, Albrecht T, et al. The EFSUMB Guidelines and Recommendations on the Clinical Practice of Contrast Enhanced Ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med. 2012;33:33-59.
35. Claudon M, Cosgrove D, Albrecht T, Bolondi L, Bosio M, Calliada F, Correas JM, et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) - update 2008. Ultraschall Med 2008;29:28-44.
36. Nylund K, Maconi G, Hollerweger A, Ripolles T, Pallotta N, Higginson A, Serra C, et al. EFSUMB Recommendations and Guidelines for Gastrointestinal Ultrasound. Ultraschall Med 2017;38:e1-e15.
37. Nylund K, Maconi G, Hollerweger A, Ripolles T, Pallotta N, Higginson A, Serra C, et al. EFSUMB Recommendations and Guidelines for Gastrointestinal Ultrasound - Part 1: Examination Techniques and Normal Findings (Long version). Ultraschall Med 2016.
38. Allgayer H, Braden B, Dietrich CF. Transabdominal ultrasound in inflammatory bowel disease. Conventional and recently developed techniques--update. Med.Ultrason. 2011;13:302-313.
39. Gorg C, Egbring J, Bert T. Contrast-enhanced ultrasound of epiploic appendagitis. Ultraschall Med 2009;30:163-167.
40. Puylaert JB. Right-sided segmental infarction of the omentum: clinical, US, and CT findings. Radiology 1992;185:169-172.
41. Miguel A, Ripollés T, Martínez MJ. Apendicitis epiploica e infarto omental: hallazgos en ecografía y tomografía computarizada. Radiología 2001;43:395-401.
42. Shiina T, Nightingale KR, Palmeri ML, Hall TJ, Bamber JC, Barr RG, Castera L, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 1: basic principles and terminology. Ultrasound Med Biol 2015;41:1126-1147.
43. Ferraioli G, Filice C, Castera L, Choi BI, Sporea I, Wilson SR, Cosgrove D, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 3: liver. Ultrasound Med Biol 2015;41:1161-1179.
44. Barr RG, Nakashima K, Amy D, Cosgrove D, Farrokh A, Schafer F, Bamber JC, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 2: breast. Ultrasound Med Biol 2015;41:1148-1160.
45. Cosgrove D, Barr R, Bojunga J, Cantisani V, Chammas MC, Dighe M, Vinayak S, et al. WFUMB Guidelines and Recommendations on the Clinical Use of Ultrasound Elastography: Part 4. Thyroid. Ultrasound Med Biol 2017;43:4-26.
46. Barr RG, Cosgrove D, Brock M, Cantisani V, Correas JM, Postema AW, Salomon G, et al. WFUMB Guidelines and Recommendations on the Clinical Use of Ultrasound Elastography: Part 5. Prostate. Ultrasound Med Biol 2017;43:27-48.
47. Trenker C, Gorg C, Jenssen C, Klein S, Neubauer A, Wagner U, Dietrich CF. [Ultrasound in oncology, current perspectives]. Z Gastroenterol 2017;55:1021-1037.
48. Dong Y, Sirli R, Ferraioli G, Sporea I, Chiorean L, Cui X, Fan M, et al. Shear wave elastography of the liver - review on normal values. Z Gastroenterol 2017;55:153-166.
49. Dietrich CF, Rudd L, Saftiou A, Gilja OH. The EFSUMB website, a great source for ultrasound information and education. Med Ultrason 2017;19:102-110.
50. Dietrich CF, Bamber J, Berzigotti A, Bota S, Cantisani V, Castera L, Cosgrove D, et al. EFSUMB Guidelines and Recommendations on the Clinical Use of Liver Ultrasound Elastography, Update 2017 (Short Version). Ultraschall Med 2017;38:377-394.
51. Dietrich CF, Bamber J, Berzigotti A, Bota S, Cantisani V, Castera L, Cosgrove D, et al. EFSUMB Guidelines and Recommendations on the Clinical Use of Liver Ultrasound Elastography, Update 2017 (Long Version). Ultraschall Med 2017;38:e16-e47.
52. Sirvanci M, Balci NC, Karaman K, Duran C, Karakas E. Primary epiploic appendagitis: MRI findings. Magn Reson Imaging 2002;20:137-139.
53. Dallal RM, Bailey LA. Omental infarction: a cause of acute abdominal pain after antecolic gastric bypass. Surg Obes Relat Dis 2006;2:451-454.
54. Kim HC, Yang DM, Jin W, Joh JH. Infarction of lesser omental fat mimicking an exophytic pancreatic tumor by sonography. J Clin Ultrasound 2011;39:412-414.
55. Tsunoda T, Sogo T, Komatsu H, Inui A, Fujisawa T. A case report of idiopathic omental infarction in an obese child. Case Rep Pediatr 2012;2012:513634.
56. Rao PM, Wittenberg J, Lawrason JN. Primary epiploic appendagitis: evolutionary changes in CT appearance. Radiology 1997;204:713-717. 57. Horton KM, Corl FM, Fishman EK. CT evaluation of the colon: inflammatory disease. Radiographics 2000;20:399-418.
58. Rao PM. CT of diverticulitis and alternative conditions. Semin Ultrasound CT MR 1999;20:86-93.
59. Singh AK, Gervais DA, Hahn PF, Rhea J, Mueller PR. CT appearance of acute appendagitis. AJR Am J Roentgenol 2004;183:1303-1307.
60. Ng KS, Tan AG, Chen KK, Wong SK, Tan HM. CT features of primary epiploic appendagitis. Eur J Radiol 2006;59:284-288.
61. Subramaniam R. Acute appendagitis: emergency presentation and computed tomographic appearances. Emerg Med J 2006;23:e53.
62. Desai HP, Tripodi J, Gold BM, Burakoff R. Infarction of an epiploic appendage. Review of the literature. J Clin Gastroenterol 1993;16:323-325.
63. Legome EL, Belton AL, Murray RE, Rao PM, Novelline RA. Epiploic appendagitis: the emergency department presentation. J Emerg Med 2002;22:9-13.
64. Legome EL, Sims C, Rao PM. Epiploic appendagitis: adding to the differential of acute abdominal pain. J Emerg Med 1999;17:823-826.
65. Vinson DR. Epiploic appendagitis: a new diagnosis for the emergency physician. Two case reports and a review. J Emerg Med 1999;17:827-832.
66. Molla E, Ripolles T, Martinez MJ, Morote V, Rosello-Sastre E. Primary epiploic appendagitis: US and CT findings. Eur Radiol 1998;8:435-438.
67. Rao PM, Rhea JT, Novelline RA, Mostafavi AA, McCabe CJ. Effect of computed tomography of the appendix on treatment of patients and use of hospital resources. N Engl J Med 1998;338:141-146.
68. Rao PM, Rhea JT, Wittenberg J, Warshaw AL. Misdiagnosis of primary epiploic appendagitis. Am J Surg 1998;176:81-85.
69. Klingenstein P. Some phases of the pathology of the appendices epiploicae. Surg Gynecol Obstet 1924;38:376.
70. Sangha S, Soto JA, Becker JM, Farraye FA. Primary epiploic appendagitis: an underappreciated diagnosis. A case series and review of the literature. Dig Dis Sci 2004;49:347-350.
71. Puppala AR, Mustafa SG, Moorman RH, Howard CH. Small bowel obstruction due to disease of epiploic appendage. Am J Gastroenterol 1981;75:382-383.
72. Balthazar EJ, Lefkowitz RA. Left-sided omental infarction with associated omental abscess: CT diagnosis. J Comput Assist Tomogr 1993;17:379-381.
11Figures
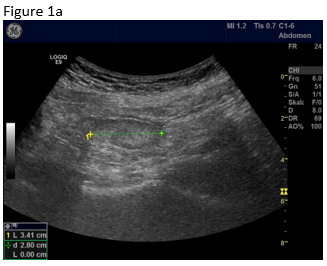
Figure 1: B-mode ultrasound using low frequency (a) and high frequency (b) revealed an isoechoic mass with a hypoechoic circumference. The mass was not adher-ent to the colon. Contrast enhanced ultrasound using low frequency (c) and high frequency (d) revealed that it was a non-enhancing segment of the omentum. Strain elastography showed that the lesion was stiffer than its sur-rounding tissue.
Figure 2: Computed tomography confirmed the finding of a partially infarcted omentum.
Figure 3: A follow up examination few weeks later revealed partially revascularised omental tissue in a now asymptomatic patient (a,b). Shear wave elastography is shown where there is now only relatively soft (inflammatory) tissue (c).
Figure 2: Computed tomography confirmed the finding of a partially infarcted omentum.
Figure 3: A follow up examination few weeks later revealed partially revascularised omental tissue in a now asymptomatic patient (a,b). Shear wave elastography is shown where there is now only relatively soft (inflammatory) tissue (c).


![Epiploic Appendagitis or Localised Omental Infarct?</br> [May 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm-may2018_fig1b.png)
![Epiploic Appendagitis or Localised Omental Infarct?</br> [May 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm-may2018_fig1c.png)
![Epiploic Appendagitis or Localised Omental Infarct?</br> [May 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm-may2018_fig1d.png)
![Epiploic Appendagitis or Localised Omental Infarct?</br> [May 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm-may2018_fig1e.png)
![Epiploic Appendagitis or Localised Omental Infarct?</br> [May 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm-may2018_fig2.png)
![Epiploic Appendagitis or Localised Omental Infarct?</br> [May 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm-may2018_fig3a.png)
![Epiploic Appendagitis or Localised Omental Infarct?</br> [May 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm-may2018_fig3b.png)
![Epiploic Appendagitis or Localised Omental Infarct?</br> [May 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm-may2018_fig3c.png)
