Epiploic Appendagitis or Localised Omental Infarct? [May 2018]
May 13, 2018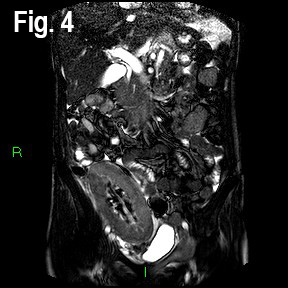
A rare cause for delayed renal transplant graft function [Jul 2018]
July 13, 2018Myotendinous rupture of the distal biceps
1 Clinic Hospital, Salamanca University, Salamanca, Spain
3 Sport Sciences Faculty, Leon University, Leon, Spain
2 Orthopedic Surgery Clínica Meds, Santiago de Chile, Chile
4 Sport Sciences Faculty, Castilla La Mancha University, Toledo, Spain
The biceps brachii is a muscle primarily supinator and secondarily flexor of the elbow. The distal tendon of the biceps is a flat tendon, which forms about 7 cm cranial to the elbow joint, from a central tendinous septum from the medial and lateral heads (Fig. 1). Once formed, superficial to the brachialis muscle, it has an oblique path from medial to lateral, and is directed in depth towards its insertion in the radial tuberosity. At the same time, it rotates 90º on its axis, so that its anterior face, faces laterally in its distal segment. Biomechanical studies have shown that the fibers of the short portion are inserted more distally in the bicipital tuberosity and contribute mainly to the flexion of the elbow and the long portion the fibres’ are inserted more proximally and they assist in supination of the forearm (1). The bicipital aponeurosis, originates, at the level of the distal myotendinous junction, of the most ventral and medial zone, crosses over the tendon and joins the superficial fascia of the forearm in the ulnar region (1,2).
Unlike avulsion of the distal tendon of the biceps brachii in the radial tuberosity, which is common, rupture of the distal myotendinous biceps junction is very rare and there are few references in the literature (3).
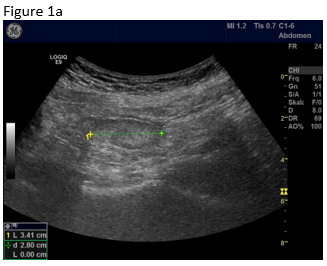
On the ultrasound study, in long axis (Fig. 3A), there was an interruption of the muscular fibrillary pattern and retraction of the central septum of the biceps. The superficial tendinous fibers and the bicipital aponeurosis were intact. In the more superficial segment (Fig. 3B), an echogenic, heterogeneous image of irregular morphology was observed between the bicipital aponeurosis and the muscle fibres of the anterior brachial muscle, which corresponds to fibrous scar. Some retraction of the superficial and deep fibro-fatty bundles and of the medial tendon septum of the biceps could also be appreciated.
In the axial or transverse section on the distal third of the forearm (Fig. 4A and B), a significant atrophy of the long (outermost) portion was observed. In the immediate deep plane, the hyperechogenic, stellate, retractable image corresponds to the fibrous scar.
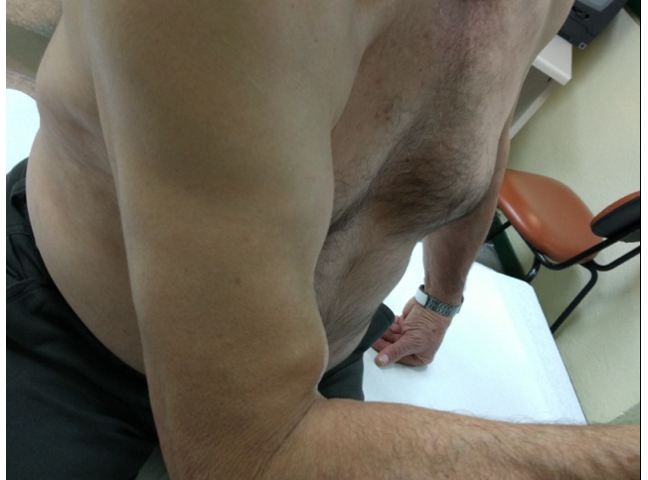
The muscle tears can be partial (only affects a part of the muscular belly), or total and affects the entire thickness of the muscle. In this case, if the muscle is superficial, a gap can be felt between the disrupted retracted end known as the "hack sign". Bruising typically appears a few hours after the injury as the blood dissects through the tissues with a tendency to distal migration. In chronic tears, moderate pain, retraction and muscular deformity can occur as in our patient (Fig. 2). The retracted muscle portions can also simulate a soft tissue mass. Palpation demonstrates a local induration that corresponds to the fibrous scar.
After the disruption of the connective septa in the muscle, haemorrhage Initially occurs, which fills the gap between the muscle ends, then the proliferation of inflammatory cells and finally the fibrous response (4). In case of complete rupture the retracted muscle ends appear inside a cavity, giving rise to an ultrasound image called the " bell clapper" sign. The blood component passes through different stages: initially, extravasated blood is a dense collection of hypoechogenic predominance, then it begins to organize, and a liquid-liquid level can appear. After several days it becomes uniform (collection of lower density, more hypoechoic and with posterior acoustic enhancement) that progressively gets reabsorbed. At approximately 48-72 hours, when the collection becomes anechoic, it is possible to determine its actual size (5). If there is a discontinuity of the fascia, the characteristic ultrasonographic finding is the presence of fluid in the epimysium surrounding the circumference of the muscle.
At the same time, the cavity begins to fill gradually from its periphery by formation of granulation tissue (confluent echogenic foci, with acoustic shadowing and attenuation), to completion (6). The muscle repair process lasts 3 to 16 weeks depending on the location and size of the lesion. This granulation tissue is sometimes very dense, causing a fibrous scar that alters the contractile function and motility of the muscle. The result is a muscle of smaller volume with echographic signs of myotendinous retraction, as in this case of the long portion of the biceps. The fibrous scar is not elastic and is mechanically less able to perform the functions of a normal muscle fibre, which predisposes to new pathology (4,7,8).
Thus, according to Jarvinen (4), to minimize disability and improve full functional recovery after skeletal muscle injuries, conservative treatment includes: compression to limit bleeding, local elevation and cooling, non-steroidal anti-inflammatory drugs (NSAIDs), and physical therapy. In case of breaks of the myotendinous distal junction of the biceps, the muscle suture is difficult and with complications. For this reason, in this type of injury, surgery is not advised, and directed rehabilitation treatment is recommended (3). The complete bicipital aponeurosis limits the proximal musculotendinous retraction, increasing the chances of a good functional recovery (3), as occured in our patient.
2.- Chew ML, Giuffré BM. Disorders of the Distal Biceps Brachii Tendon. Radiographics,2005,Vol.25:1227-1237.
3.- Schamblin ML, Safran MR. Injury of the distal biceps at the musculotendinous junction. Shoulder Elbow Surg 2007; 16:208-12.
4.- Järvinen TA, Järvinen M, Kalimo Hannu. Regeneration of injured skeletal muscle after the injury. Muscles Ligaments Tendons J. 2013;3(4):337-345.
5.- Takebayashi S, Takasawa H, Banzai Y, Miki H, Sasaki R, Itoh Y, Matsubara S. Sonographic Findings in Muscle Strain Injury: Clinical and MR Imaging Correlation. J Ultrasound Med 1995; 14: 899-905.
6.- Obaid, H.: Sonographic Appearance of Side Strain Injury, American Journal of Roentgenology 2008; 191: W264–W267.
7.- Cambell SE, Ronald A, Sofka C. Ultrasound of Muscle Abnormalities. Ultrasound Quarterly 2005; 2: 87-94.
8.- Slavotinek, J.: Muscle Injury: The Role of Imaging in Prognostic Assignment and Monitoring of Muscle Repair, Seminars in Musculoskeletal Radiology 2010;14:194–200
Axial section:
Long head (white circle). Short head (white triangle). Central tendinous septum (arrow). Bicipital aponeurosis (tick). Anterior brachial muscle (pointed square).
Longitudinal section:
Bicipital aponeurosis (tick). Central septum of the biceps tendon (arrow). Anterior brachial muscle (pointed square).
Figure 2: Clinical image to see the alteration of the shape in the biceps brachii, with two prominences (arrow), corresponding to the ends of the break.
Figure 3: Over the most distal portion of the biceps brachii muscle.
Internal longitudinal section. (A) Disruption of the distal fibers of the biceps (white circle). Retraction of the central tendinous septum (arrow). Persistence of fibers corresponding to the bicipital aponeurosis (tick). Anterior brachial muscle (pointed square).
External longitudinal section. The fibrous scar (star). Retraction of the central tendinous septum (arrow). Anterior brachial muscle (pointed square).
Figure 4: Over the most distal portion of the biceps brachii muscle
Axial incidence. Long head of the bíceps brachii muscle (white circle). The fibrous scar (star). Retraction of the central tendinous septum (arrow). Anterior brachial muscle (pointed square). The bicipital aponeurosis (tick).
In the most distal axial section. Fibrous scar (star). The distal myotendinous junction of both muscular portions (short (white circle) and long (white triangle)).


![Myotendinous rupture of the distal biceps</br> [Jun 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotmJune2018_fig1a-b.png)
![Myotendinous rupture of the distal biceps</br> [Jun 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotmJune2018_fig2.png)
![Myotendinous rupture of the distal biceps</br> [Jun 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotmJune2018_fig3a-b.png)
![Myotendinous rupture of the distal biceps</br> [Jun 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotmJune2018_fig4a-b.png)
