Student Image Challenge 99
November 16, 2023
Student Image Challenge 100
December 5, 2023SUBMIT YOUR CASE
EFSUMB invites submission of interesting cases for the website section 'Case of the Month'. All CoM submissions are eligible for selection for free registration at the next Euroson congress. Two cases that receive the most 'likes' in a year will receive free registration for the next EUROSON congress and the third most liked liked case will receive a cash prize of 100 EUR.
Giant cell tumor with additional synovial proliferations
Authors: Ulrich Kaiser; Prof. Dr. Ernst Michael Jung, MHBA [1]
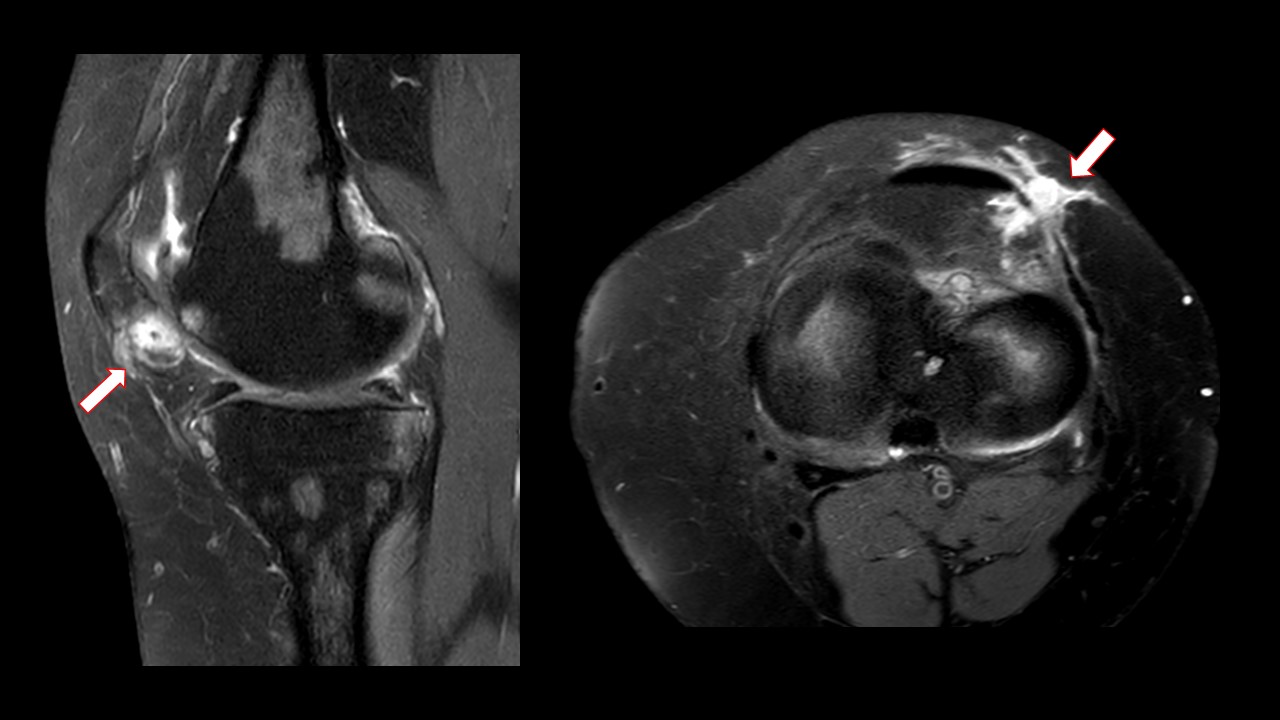
[1] Ultrasound Center, University Hospital Regensburg, Regensburg, GermanyFigure 1. MRI reporting: Native T1 and T2 sequences, i.v. contrast administration of gadolinium with contrast-enhanced T1-VIBE 3 D sequence by subtraction technique. There was increased intra-articular fluid accumulation in the knee joint. Signal changes indicate chondral changes in the area of the patella. There was nodular contrast media accumulation at the medial patellar rim and irritation with hyperemia of the capsule.
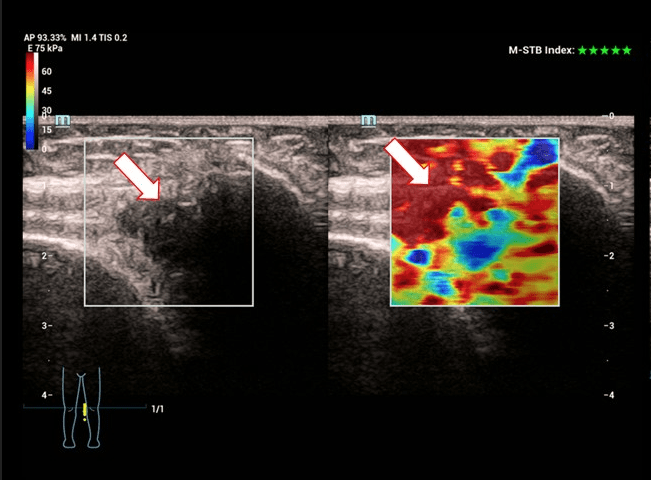
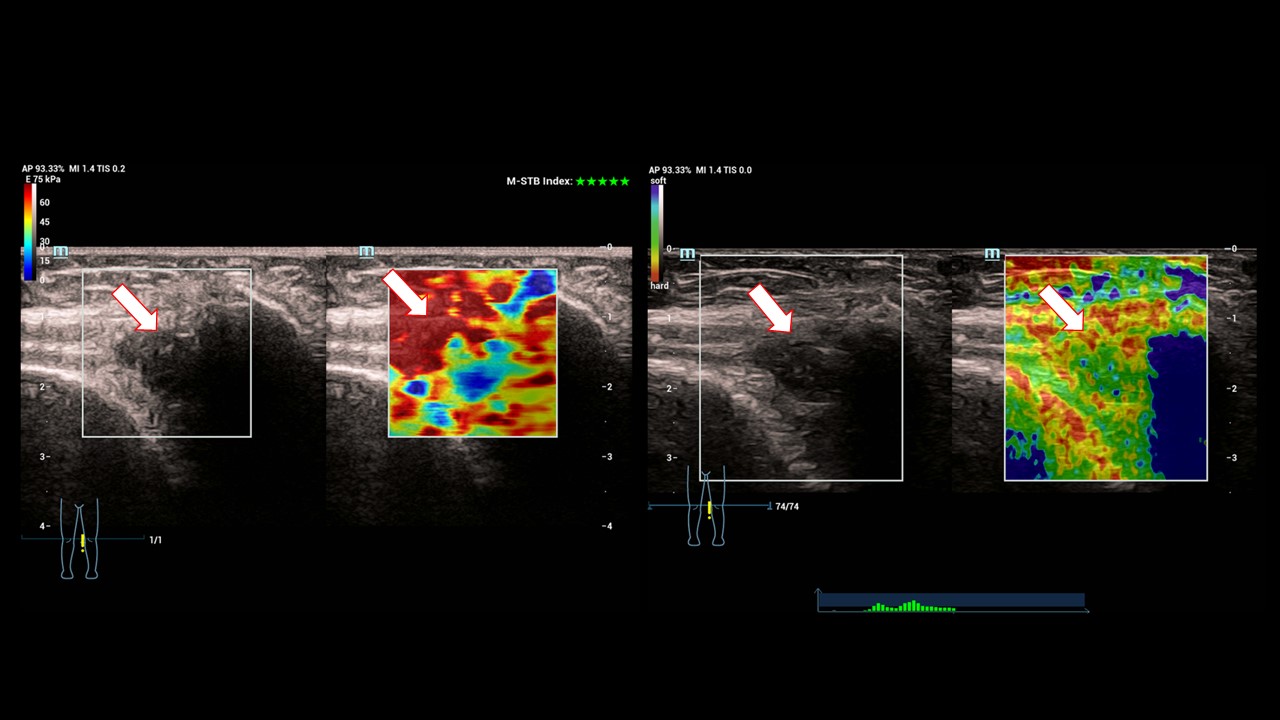
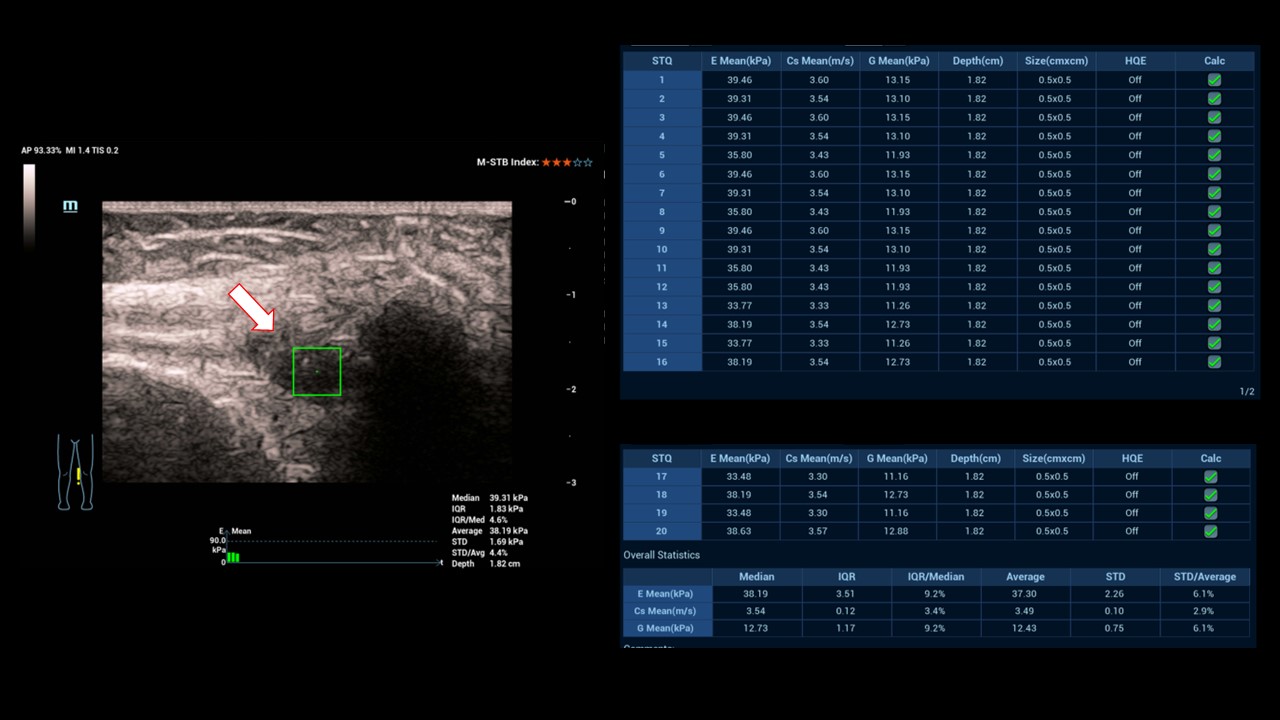
Figure 3. Strain and Share Wave elastography: The nodular changes at the medial patellar rim appeared inhomogeneous, clearly condensed with circumscribed measurable structural changes at elevated shear wave velocities of more than 2.5 m/s or more than 30 Kpa (Fig.3, 4). Thus, tumorous changes were also conceivable.
Figure 4. Strain and Share Wave elastography: The nodular changes at the medial patellar rim appeared inhomogeneous, clearly condensed with circumscribed measurable structural changes at elevated shear wave velocities of more than 2.5 m/s or more than 30 Kpa (Fig.3, 4). Thus, tumorous changes were also conceivable.
Magnetic resonance imaging (MRI) of the knee joint revealed unclear synovial changes suggestive of inflammation with reactive changes. Differential diagnosis includes unclear proliferating condensations in the sense of synovitis, pigmented nodular synovitis, bacterial synovitis or a giant cell tumor. A solid tumor could not be excluded.
The specific request of the treating colleagues was related to the performance of a US biopsy. For this purpose, the corresponding educational discussion on US-guided biopsy was conducted with written consent and an appointment was made immediately.
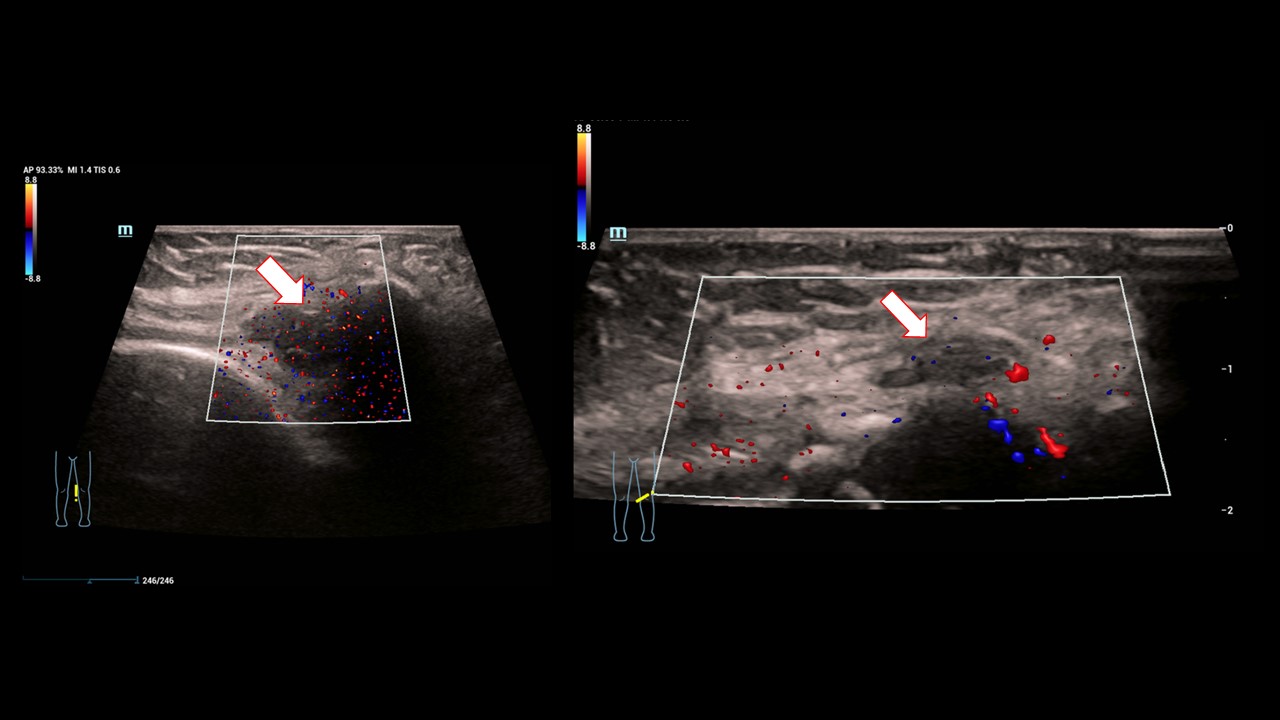
Diagnostic US examination was performed with multiple multifrequency probes between 6 and 18 MHz with B-mode, Color Doppler ultrasonography (CCDS), and elastography, and digitally documented. The laboratory constellation showed a mild inflammatory reaction. There was no bleeding tendency.
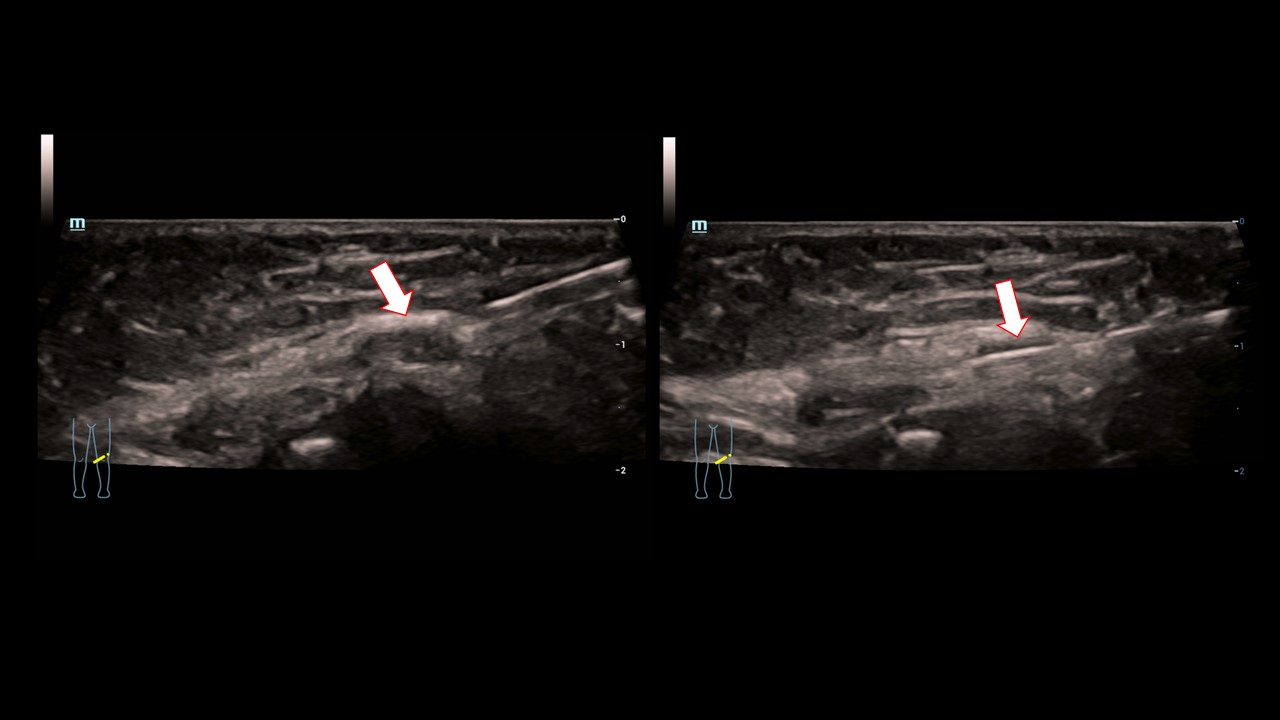
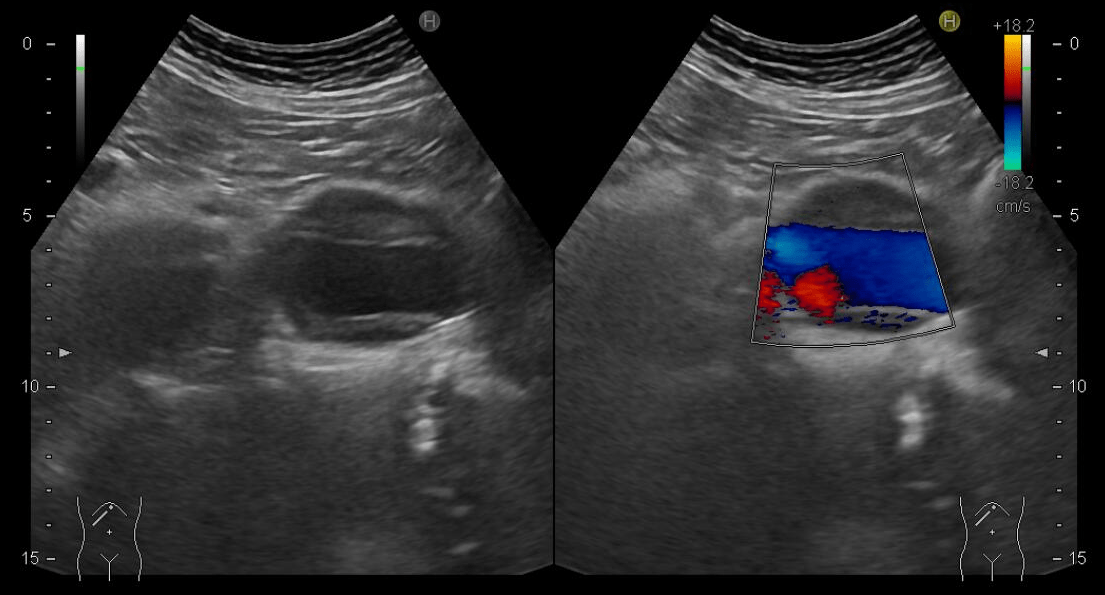
US findings B-mode and CCDS: Capsular thickening predominantly medial, increased intra-articular fluid. Low-echo nodular change up to 10 x 5 x 4 mm at the medial patellar rim. Marginal hypervascularization (Fig.2).
Strain and Share Wave elastography: The nodular changes at the medial patellar rim appeared inhomogeneous, clearly condensed with circumscribed measurable structural changes at elevated shear wave velocities of more than 2.5 m/s or more than 30 Kpa (Fig.3, 4). Thus, tumorous changes were also conceivable.
US biopsy with 18-G needle: With a possible suspicious diagnosis of tumor, a 18-G needle biopsy was performed under trocar protection (Fig.5). Representative whitish cylinders were obtained from the nodular changes. Complications did not occur.
The literature describes that in addition to synovitis, which can be actively inflammatory, a giant cell tumor of the knee joint should always be considered, especially in young people up to 45 years of age. Typical findings are small-nodular, partially hypervascularized changes in the area of the capsule-ligament apparatus. A difficult differential diagnosis to distinguish is pigmented veno-nodular synovitis. The giant cell tumor may also lead to intraosseous changes. In the present case, the patella was partially affected. It is still a rare constellation of findings that should be considered especially in the absence of bacterial inflammation and trauma to the knee joint. US-guided punch biopsy provides a very good opportunity for immediate histologic confirmation.
According to the World Health Organization (WHO) 2020 classification, tenosynovial giant cell tumor (TGCT) comprises a group of lesions that most commonly arise from the synovium of joints, bursae, and tendon sheaths and exhibit synovial differentiation. The vast majority are benign but locally aggressive tumors. TGCTs are usually differentiated according to their growth pattern (diffuse or localized) and location (intra- or extraarticular). Previously called pigmented villonodular synovitis (PVNS), diffuse TGCT is rare, with only four cases per million people per year.
Giant cell tumor of bone (GCTB) is a locally aggressive tumor that occurs preferentially in the metaphysis/epiphysis of long bones and accounts for 4-5% of primary bone tumors. GCTB shows two main cell populations: mononuclear cells and non-neoplastic giant cells with multiple nuclei, with or without fibrous background. On the other hand, giant cell-poor GCTB are rare and there are few reports in the literature. These cases present a diagnostic challenge due to the absence of giant cells and the consistent detection of the H3F3A gene mutation by sequencing in these cases.
CLINICAL PERSPECTIVE:
Giant cell tumor of bone (GCTB) and tenosynovial giant cell tumor (TGCT) have misleadingly similar names, macroscopically a soft texture and brown color, microscopically osteoclast-like multinucleated giant cells and localization in the musculoskeletal system. However, these two tumor types are two biologically and clinically distinct entities with different natural histories and significantly different surgical and medical treatments. GCTB usually occurs as a solitary lesion in the meta-epiphyseal region of the long bones. Diagnosis can be made using plain radiographs, CT x-rays, MRI, or ultrasound techniques to assess the extent of the tumor and soft tissue and joint involvement.
THERAPY PLANNING:
The only curative treatment is adequate surgical care. However, this can be significantly complicated by e.g. difficult anatomical localizations or only possible to a limited extent. Regarding effective systemic therapies, corresponding investigations are currently taking place.
OUTCOME & PROGNOSIS:
The case was presented and discussed in a tumor conference. Here, the recommendation was made to perform surgical treatment. This is now planned in the further course and has not yet taken place.
2) Formica VM, Bruno V, Scotto Di, et al. The giant cell tumor during pregnancy: A review of literature. Orthop Traumatol Surg Res 2023; 109(3): 103396.
3) Rekhi B, Dave V. Giant cell tumor of bone: An update, including spectrum of pathological features, pathogenesis, molecular profile and the differential diagnoses. Histol Histopathol 2023; 38(2): 139-153.
4) Yakoub MA, Torrence D, Hwang S, Bartelstein M, Healey JH, Hameed M. Giant-cell-poor giant cell tumor of bone: report of two cases and literature review. Skeletal Radiol 2023 ;52(9): 1791-1798.
5) Kropivšek L, Pižem J, Mavčič B. Giant cell tumor of bone versus tenosynovial giant cell tumor - similarities and differences. Int J Surg Pathol 2022; 30(6): 596-605.
6) Tahir I, Andrei V, Pollock R, Saifuddin A. Malignant giant cell tumour of bone: a review of clinical, pathological and imaging features. Skeletal Radiol 2022; 51(5): 957-970.
7) Jung EM, Dong Y, Jung F. Current aspects of multimodal ultrasound liver diagnostics using contrast-enhanced ultrasonography (CEUS), fat evaluation, fibrosis assessment, and perfusion analysis - An update. Clin Hemorheol Microcirc 2023; 83(2): 181-193.