- European Federation of Societies for Ultrasound in Medicine and Biology ~ Educating all for competence to practice ultrasound safely
CEUS in the Evaluation of Treatment Procedures
July 15, 2016
Bilateral quadriceps muscles and suprapatellar recesses injuries: ultrasound evaluation [Sep 2016]
September 11, 2016Hepatic adenoma with focal hepatocellular carcinoma
Correspondence: Carmen Garre. Servicio Aparato Digestivo. 7ª Izda, Hospital “Virgen de la Arrixaca”.
Ctra Cartagena s/n. 30200, Murcia (Spain)
Garre.carmen@gmail.com
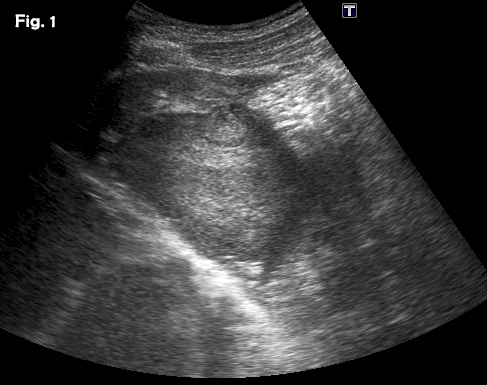
A previously healthy 39-year-old male was referred because of a hepatic mass, found incidentally He was a professional sportsman and regularly participated in competitions. He had taken anabolic steroids for 6-8 weeks two or three times per year from 24 – 32 years old approximately. The remainder of the medical history was unremarkable. Laboratory results showed a slight elevation of ALT and AST with normal bilirubin and alpha-fetoprotein levels. Physical examination was otherwise normal. An abdominal ultrasound showed a well-defined 8.5 x 7.7 cm heterogeneous mass with a hypoechoic peripheral halo in the left lobe of the liver, segments 2 and 3 (Fig 1). A small nodule-in-nodule appearance was evident within the mass as well as some vascularity on colour Doppler. Following the administration of an ultrasound contrast agent (SonoVueTM), the mass showed homogeneous hyper-enhancement in the arterial phase (Fig 2a) (video 1), with wash-out in the late phase in only part of the lesion (video 2), specifically, the nodule-in-nodule appearance area (Fig 2b). These appearances were suggestive of a hepatocellular adenoma with areas of malignant transformation and this was confirmed by both ultrasound guided fine-needle aspiration cytology (video 3) and subsequent histological examination of the surgically resected tumour.
Hepatic adenomas or hepatocellular adenomas (HCA) are uncommon benign epithelial liver tumours and are strongly associated with use of oral contraceptives , anabolic androgens and glycogen storage disease . The incidence has increased in the last few decades due to the use of oral contraceptives and anabolic steroids for the treatment of impotence and muscle mass development in body builders and in transsexuals2. They are also associated with malignant transformation to hepatocellular carcinoma (HCC), spontaneous haemorrhage and rupture. According to the literature, this risk of malignant transformation of HCA to HCC is not a rare occurrence, a recent systematic review of 1617 HCA reporting an overall malignant transformation rate of 4,2%, among all adenoma cases and 4,5% among all resected HCAs . HCA with mutations in beta-catenin have frequent cytologic abnormalities and pseudo-glandular formation and, therefore, they have an increased potential for malignant transformation - . The sonographic features of HCAs are nonspecific and may mimic other benign or malignant liver lesions. In B-mode ultrasound, they may appear well-demarcated and are usually isoechogenic with the surrounding liver tissue or hyperechogenic because of high lipid content of hepatocytes. Intratumoral hemorrhage can also result in increased echogenicity and heterogeneity whereas recent hemorrhages appear as hypoechoic areas . On CEUS, HCA display arterial hyperenhancement, usually at the periphery initially with subsequent very quick centripetal filling, in direct contrast to focal nodular hyperplasia (FNH). However, this arterial enhancement pattern may also be seen in HCC and hyperenhancing metastases and is not pathognomonic of HCA Percutaneous liver biopsy or fine-needle aspiration is usually not indicated since adenomas have a tendency to bleed following biopsy and also particularly because the amount of tissue obtained is often insufficient to confirm a diagnosis. However, when a lesion is suspicious of malignant transformation, biopsy can confirm the diagnosis before surgical resection .
- Rosenberg L. The risk of liver neoplasia in relation to combined oral contraceptive use. Contraception 1991; 43(6): 643-652.
- Martin NM, Abu Dayyeh BK, Chung RT. Anabolic steroid abuse causing recurrent hepatic adenomas and hemorrhage. World J. Gastroenterol 2008; 14(28): 4573-75.
- Labrune P, Trioche P, Duvaltier I, et al. Hepatocellular adenomas in glycogen storage disease type I and III: a series of 43 patients and review of the literature. J Ped Gastroenterol Nutr 1997; 24(3): 276-279.
- Stoot JH, Coelen RJ, De Jong MC, Dejong CH: Malignant transformation of hepatocellular adenomas into hepatocellular carcinomas: a systematic review including more than 1600 adenoma cases. HPB (Oxford) 2010;12:509–522.
- Bioulac-Sage P, Rebouissou S, Thomas C, Blanc JF, Saric J, Sa Cunha A, Rullier A, Cubel G, Couchy G, Imbeaud S, Balabaud C, Zucman-Rossi J. Hepatocellular adenoma subtype classification using molecular markers and immunohistochemistry. Hepatology 2007; 46: 740-748.
- Kohene de gonzalez AK, Salomao MA, Lagana SM. Current conceps in the immunohistochemical evaluation of liver tumors. World J Hepatol 2015; 7(10):1403-11.
- Garre Sánchez MC, Gómez Rodriguez RA and Zaragosi Esparza A. Lesiones Focales hepáticas. En: Tratado de ultrasonografia abdominal. Madrid. Ed Diaz de Santos. 71-107.
- Claudon M, Dietrich C F, Choi B I, et al. Guidelines and Good Clinical Practice Recommendations for Contrast Enhanced Ultrasound (CEUS) in the Liver – Update 2012. Ultraschall in Med 2013; 34: 11–29.
- Baheti AD, Yeh MM, O’Malley R, Lalwani N. Malignant transformation of hepatic adenoma in glycogen storage disease type -1a: report of an exceptional case diagnosed by surveillance imaging. J Clin Imaging Sci 2015; 5:47.
Figure 2:Contrast-enhanced ultrasound (CEUS) in the arterial (a) and late (b) phase. CEUS showed early hyperenhancing features in the arterial phase of the lesion and clear wash out in the small nodule-in-nodule appearance without wash out in the rest of the lesion.


![Hepatic adenoma with focal hepatocellular carcinoma</br> [Aug 2016]](https://efsumb.org/wp-content/uploads/2020/11/cotm_august2016_fig02a.jpg)
![Hepatic adenoma with focal hepatocellular carcinoma</br> [Aug 2016]](https://efsumb.org/wp-content/uploads/2020/11/cotm_august2016_fig02b.jpg)
