Don’t forget about the intramuscular metastasis! [Dec 2018]
December 18, 2018Basic Obstetric Scanning
January 25, 2019Looks can be deceiving in gastric submucosal lesions
Authors:
Alina Constantin, Adrian Săftoiu, Cătălin Copăescu Ponderas Academic Hospital, Bucharest
Alina Constantin, Adrian Săftoiu, Cătălin Copăescu Ponderas Academic Hospital, Bucharest
1Abstract
Subepithelial lesions (SELs) are tumors that appear as a bulge or mass on endoscopy with normal appearing overlying mucosa and originate from the muscularis mucosa, submucosa, or muscularis propria (1). Initial management of SELs centers on proper diagnosis and determination of any malignant potential of the lesion. Endoscopic evaluation alone is insufficient for diagnosing the etiology of a subepithelial lesion. Endoscopic ultrasound (EUS) is the most accurate imaging test for evaluation of SELs of the gastrointestinal (GI) tract (2). We present a case where an ulcerated gastric SELs presenting as GI bleeding was classified as a gastrointestinal stromal tumor (GIST), based on the endoscopic appearance and location. EUS showed well-defined hyperechoic lesion arising from the submucosal layer, characteristic for lipoma, with no need for tissue sampling.
Keywords: Subepithelial lesions (SELs), EUS-FNA, EUS-FNB, Lipoma, GIST
Keywords: Subepithelial lesions (SELs), EUS-FNA, EUS-FNB, Lipoma, GIST
2Case Report
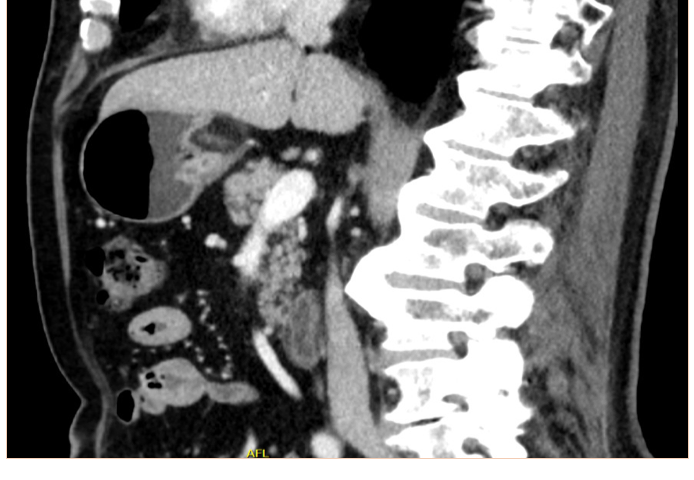
We report the case of a 66-year-old gentleman, known to suffer from high blood pressure, diabetes mellitus type 2, dyslipidemia, cervical and lumbar spondylosis, who presented to the emergency department with asthenia, pallor, melena. On physical examination, the patient was tachycardic with a heart rate of 120, and had a blood pressure of 100/60. He was pale but conscious and orientated. Cardiovascular and respiratory examinations were normal. His abdomen was soft, non-distended, bowel sounds were present and no palpable masses were felt. His laboratory investigations showed a mild normochromic, normocytic anaemia, low haematocrit, hyperglycemia, hypercholesterolemia. The patient was initially resuscitated and stabilized with intravenous fluids and proton pump inhibitors were initiated (iv 80 mg bolus and continuous infusion 8 mg/h). A naso-gastric tube was inserted which produced 300 ml of fresh blood. The patient underwent an urgent upper GI endoscopy which revealed an antral submucosal tumour with an ulcer over the mass. No active bleeding was seen during the procedure. A CT scan of the abdomen and pelvis highlighted a 30/20/18 mm oval shaped soft tissue lesion of fat density arising from the posterior wall of the stomach, with no associated lymphadenopathy. The liver, spleen, and pancreas all appeared normal (Fig 1,2). EUS has been performed and revealed a 30/18 mm intensely hyperechoic lesion continuous with the submucosal layer of the GI tract wall. The lesion was also soft on elastography, and as all the features were suggestive of a benign lesion, tissue sampling was not performed at that stage (Fig 3,4). The patient’s case was discussed at the Tumor Board meeting. The joint decision was to proceed with an exploratory laparoscopy and resect the benign mass. Histopathological examination confirmed the diagnosis of lipoma (Fig 5,6).
3Discussion
SELs of the GI tract are tumors that originate from the muscularis mucosa, submucosa, or muscularis propria. They usually are identified during routine upper and lower endoscopy as bulge or mass with normal overlying mucosa. The majority are small (<2 cm in diameter) and found incidentally; however, SELs can present with bleeding, obstruction, or metastases, depending on tumor size, location, and histopathology (3). Appropriate evaluation and management of subepithelial masses is essential since these lesions can potentially be malignant. Endoscopic evaluation alone is insufficient for diagnosing the etiology of a subepithelial lesion, thus another imaging modality is needed. Although CT scan offers information about both the gastric wall and the extragastric extent of the disease, the most accurate imaging test for the evaluation of GI SELs remains EUS due to his ability to delineate individual histologic layers. Furthermore, it can accurately distinguish between extrinsic compression of the GI tract and an intramural growth. In addition, it can evaluate the lesion size and the presence of associated lymphadenopathy for further staging. Finally, EUS-guided FNA (EUS-FNA) and fine-needle biopsy (FNB) allow tissue diagnosis to guide further management (4).
Regarding our case, based on the endoscopic appearance and location of the SELs, gastrointestinal stromal tumor (GIST), a neoplastic lesion with malignant potential was the most likely diagnosis. Differential diagnosis included surely benign lesions such as a lipoma, leiomyoma or schwannoma. The diagnosis of lipoma was suspected on abdominal CT scan and was confirmed by EUS. The joint decision to proceed with an exploratory laparoscopy and resect the benign mass was made based on the latest recommendation of the American Society for Gastrointestinal Endoscopy (ASGE). The suggestion of ASGE was that symptomatic GI lipoma should be resected or followed up.
Regarding our case, based on the endoscopic appearance and location of the SELs, gastrointestinal stromal tumor (GIST), a neoplastic lesion with malignant potential was the most likely diagnosis. Differential diagnosis included surely benign lesions such as a lipoma, leiomyoma or schwannoma. The diagnosis of lipoma was suspected on abdominal CT scan and was confirmed by EUS. The joint decision to proceed with an exploratory laparoscopy and resect the benign mass was made based on the latest recommendation of the American Society for Gastrointestinal Endoscopy (ASGE). The suggestion of ASGE was that symptomatic GI lipoma should be resected or followed up.
4Conclusion
Initial management of SELs centers on proper diagnosis and determination of any malignant potential of the lesion. EUS is the most accurate imaging test for evaluation of SELs of the GI tract. Lipoma is a well-defined hyperechoic lesion arising from the submucosal layer and does not require follow up or therapy unless is symptomatic.
5References
[1] Humphris JL, Jones DB. Subepithelial mass lesions in the upper gastrointestinal tract. J Gastroenterol Hepatol 2008;23:556-66.
[2] Hwang JH, Saunders MD, Rulyak SJ, et al. A prospective study comparing endoscopy and EUS in the evaluation of GI subepithelial masses. Gastrointest Endosc 2005;62:202-8.
[3] Hwang JH, Rulyak SD, Kimmey MB. American Gastroenterological Association Institute technical review on the management of gastric subepithelial masses. Gastroenterology 2006;130:2217-2228.
[4] A. Faulx, S. Kothari et al, The role of endoscopy in subepithelial lesions of the GI tract, Gastrointestinal Endoscopy , Volume 85, No. 6 : 2017
[5] S. Termos, O. Reslan et al, Giant gastric lipoma presenting as GI bleed: Enucleation or Resection?, International Journal of Surgery Case Reports 41 (2017) 39–42
[2] Hwang JH, Saunders MD, Rulyak SJ, et al. A prospective study comparing endoscopy and EUS in the evaluation of GI subepithelial masses. Gastrointest Endosc 2005;62:202-8.
[3] Hwang JH, Rulyak SD, Kimmey MB. American Gastroenterological Association Institute technical review on the management of gastric subepithelial masses. Gastroenterology 2006;130:2217-2228.
[4] A. Faulx, S. Kothari et al, The role of endoscopy in subepithelial lesions of the GI tract, Gastrointestinal Endoscopy , Volume 85, No. 6 : 2017
[5] S. Termos, O. Reslan et al, Giant gastric lipoma presenting as GI bleed: Enucleation or Resection?, International Journal of Surgery Case Reports 41 (2017) 39–42


![Looks can be deceiving in gastric submucosal lesions </br> [Jan 2019]](https://efsumb.org/wp-content/uploads/2020/11/jan2019-fig01.png)
![Looks can be deceiving in gastric submucosal lesions </br> [Jan 2019]](https://efsumb.org/wp-content/uploads/2020/11/jan2019-fig02.png)
![Looks can be deceiving in gastric submucosal lesions </br> [Jan 2019]](https://efsumb.org/wp-content/uploads/2020/11/jan2019-fig03.png)
![Looks can be deceiving in gastric submucosal lesions </br> [Jan 2019]](https://efsumb.org/wp-content/uploads/2020/11/jan2019-fig04.png)
![Looks can be deceiving in gastric submucosal lesions </br> [Jan 2019]](https://efsumb.org/wp-content/uploads/2020/11/jan2019-fig05.png)
![Looks can be deceiving in gastric submucosal lesions </br> [Jan 2019]](https://efsumb.org/wp-content/uploads/2020/11/jan2019-fig06.png)
