A rare case of a co-located pigmented naevus and dermal cyst: The utility of very high frequency Ultrasound and Videodermoscopy for differentiation [Nov 2018]
November 18, 2018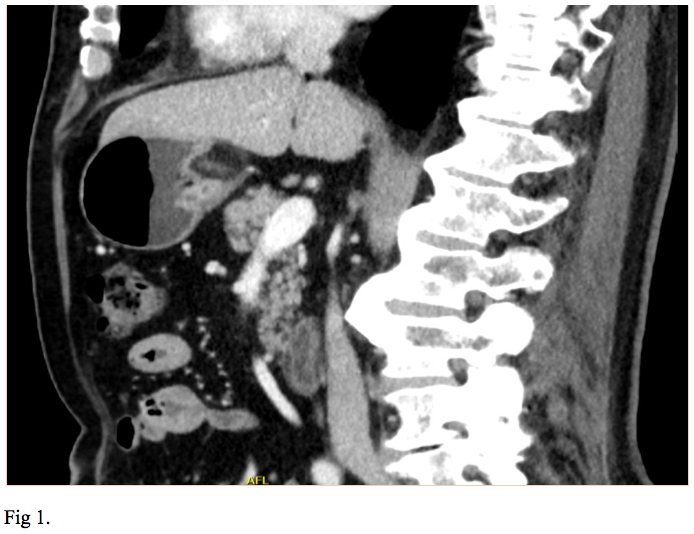
Looks can be deceiving in gastric submucosal lesions [Jan 2019]
January 23, 2019Don’t forget about the intramuscular metastasis!
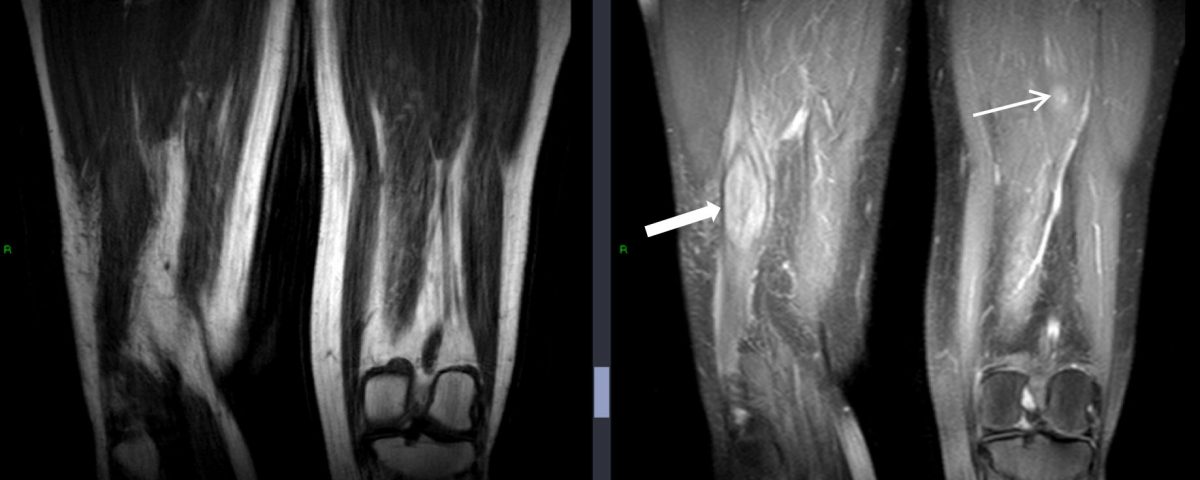
Figure 2 – initial external MR - confirms larger mass within right distal biceps femoris muscle (solid arrow) and demonstrates further, smaller mass between fat plans of left posterior thigh muscles (line arrow) - T1w and PDW DRI images (Fig 2a) - T1W FS Gadolinium enhanced MR – demonstrates enhancing intramuscular lesions with peripheral oedema (arrows) (Fig 2b)
Figure 2 – initial external MR - confirms larger mass within right distal biceps femoris muscle (solid arrow) and demonstrates further, smaller mass between fat plans of left posterior thigh muscles (line arrow) - T1w and PDW DRI images (Fig 2a) - T1W FS Gadolinium enhanced MR – demonstrates enhancing intramuscular lesions with peripheral oedema (arrows) (Fig 2b)
Figure 3 – PETCT images demonstrate avid lesions in both thighs (a) and further avid lesion in posterior mediastinum (b) - PET CT images of both legs demonstrate avid FDG take up in right and left lesions (Fig 3a) - ET CT showing Mediastinal primary tumour which also demonstrates FDG avidity (Fig 3b)
Figure 3 – PETCT images demonstrate avid lesions in both thighs (a) and further avid lesion in posterior mediastinum (b) - PET CT images of both legs demonstrate avid FDG take up in right and left lesions (Fig 3a) - ET CT showing Mediastinal primary tumour which also demonstrates FDG avidity (Fig 3b)
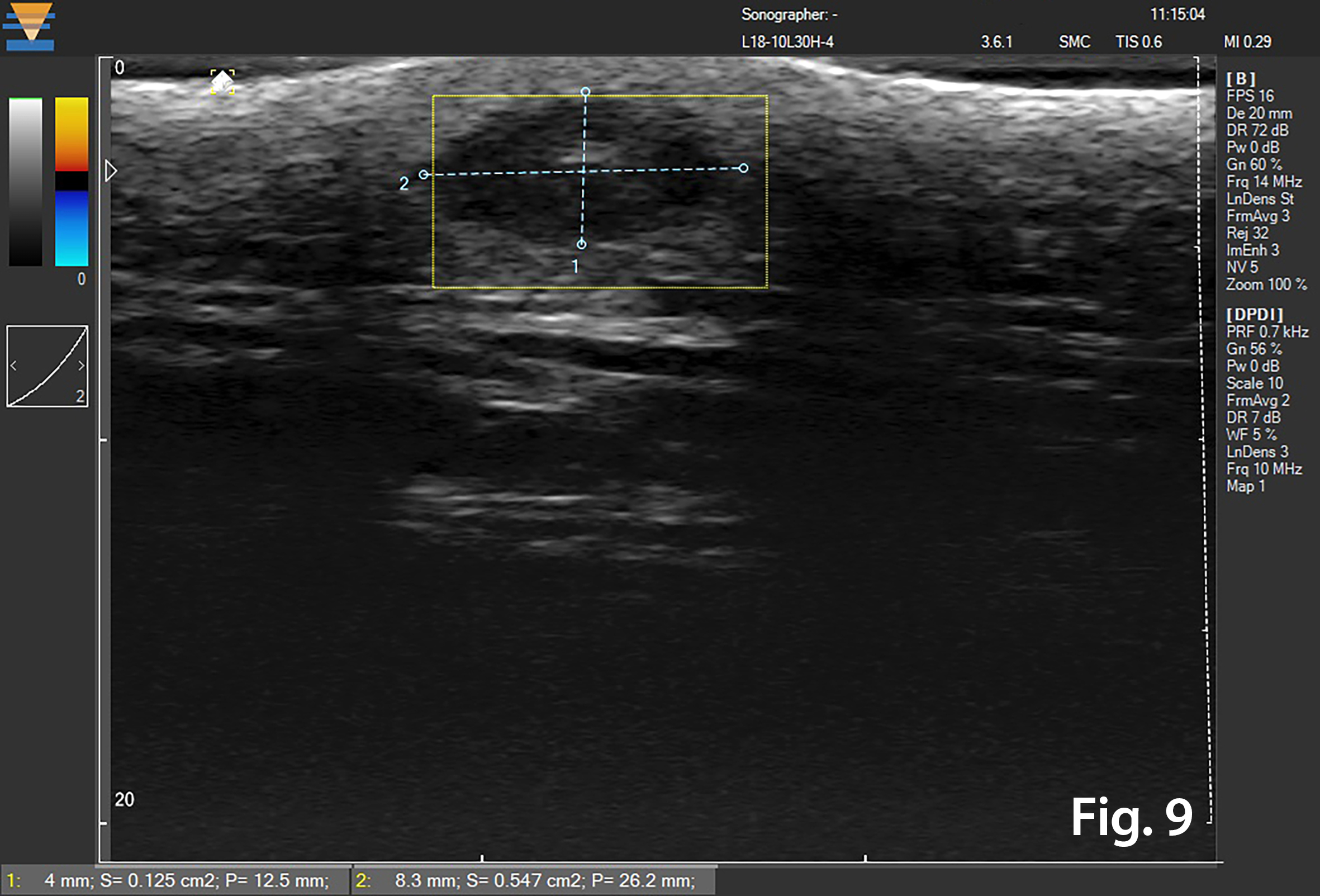
Figure 5 – New presentation of left calf pain with clinical suspicion of a deep venous thrombosis(DVT) – US demonstrated a well-defined hypoechoic mass lesion (a)with moderate vascularity (b) in left gastrocnemius. - Hypoechoic lesion in L gastrocnemius (Fig 5a) - Vascularity demonstrated on Microflow Imaging. (Fig 5b)
Figure 5 – New presentation of left calf pain with clinical suspicion of a deep venous thrombosis(DVT) – US demonstrated a well-defined hypoechoic mass lesion (a)with moderate vascularity (b) in left gastrocnemius. - Hypoechoic lesion in L gastrocnemius (Fig 5a) - Vascularity demonstrated on Microflow Imaging. (Fig 5b)
A subsequent PET-CT showed further lesions in the proximal thigh and anterior superior iliac spine as well as a 5cm posterior mediastinal mass. The overall findings were in keeping with a metastatic germ cell tumour with soft tissue metastases to the right and left thigh. The patient was treated with therapeutic radiotherapy followed by chemotherapy and initially deemed to have a good response with no measurable disease elsewhere apart from the mediastinal mass. She then re-presented in 2018 for an US Doppler of the leg owing to “calf pain” and the possibility of a deep vein thrombosis (DVT). The ultrasound findings unfortunately demonstrated a mass at the site of tenderness and was subsequently biopsied.
- Ultrasound 2016 (Figure 1)
- There was an abnormal soft tissue mass in the distal posterior thigh, related to the biceps femoris.
- MRI 2016 (Figure 2)
- Elliptical mass like lesion measuring 7.2 x 2.7cm on T1 weighted imaging which was isointense to normal muscle but demonstrates patchy, peripheral enhancement following gadolinium injection. The mass was within the short head of biceps femoris muscle.
- Another smaller similar lesion was noted within left thigh, measuring 2.9cm lying in the fat plane between posterior thigh muscles.
- PET/CT Sep 2016 (Figure 3)
- FDG acid lesions seen in both thighs and within posterior mediastinum
- MRI 2017- post chemotherapy (Figure 4)
- Both muscle lesions showed a significant reduction in size
- Recent Ultrasound 2018 (Figure 5)
- There was an irregular mass in the left gastrocnemius at the site of tenderness. It was moderately vascular and was subsequently biopsied to reveal a new metastatic deposit similar to the previous lesions and thus disease progression.
The expression of tumour markers determines the characterisation of these tumours – either seminoma, teratoma (mature and immature) and non-seminomatous germ cell tumours (NSGCTs), with the prognosis of NSGCTs being associated with the poorest outcome [3]. Specifically, a mediastinal primary is classed as a further indicator of poor prognosis by the International Germ cell consensus classification[4]. For NSGCTs, the common therapeutic strategy is chemotherapy followed by surgery to resect the residual mediastinal tumour. Metastatic spread from NSGCTs is seen to the lung in around 10% of patients with mediastinal disease [1], with the next most common sites being liver and CNS. A number of case reports have described muscular metastases from testicular GCTs [5,6], however, there is very little in the literature describing muscular metastases from mediastinal NSGCTs at primary presentation.
[2] Tumors of the Lung, Pleura, and Mediastinum - Kenneth E. Rosenzweig MD, Lee M. Krug MD, in Leibel and Phillips Textbook of Radiation Oncology (Third Edition), 2010, Saunders
[3] C. R. Nichols, “Mediastinal germ cell tumours: clinical features and biologic correlates,” Chest, vol. 99, no. 2, pp. 472–479, 1991.
[4] International Germ Cell Consensus Classification: a prognostic factor-based staging system for metastatic germ cell cancers. International Germ Cell Cancer Collaborative Group. Mead, G.M et al. J Clin Oncol. 1997 Feb; 15(2):594-603.
[5] Mixed Germ Cell Testicular Cancer with Left Ventricular Metastasis Presenting with Embolic Stroke and Small Bowel Tumor Seeding. Sundararajan S, Braunhut B, Ahmann F, Agarwal A. Case Rep Oncol Med. Vol 2014; 5 pages, article ID 250531.
[6] Metastatic Germ-Cell Cancer. Jan Menke, M.D., and Eckhardt Grabbe, M.D. July 26, 2007 N Engl J Med 2007; 357:391 DOI: 10.1056/NEJMicm060694


![Don’t forget about the intramuscular metastasis! </br> [Dec 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotmDec2018_fig1a.jpg)
![Don’t forget about the intramuscular metastasis! </br> [Dec 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotmDec2018_fig1b.jpg)
![Don’t forget about the intramuscular metastasis! </br> [Dec 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotmDec2018_fig2a.jpg)
![Don’t forget about the intramuscular metastasis! </br> [Dec 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotmDec2018_fig2b.jpg)
![Don’t forget about the intramuscular metastasis! </br> [Dec 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotmDec2018_fig3a.jpg)
![Don’t forget about the intramuscular metastasis! </br> [Dec 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotmDec2018_fig3b.jpg)
![Don’t forget about the intramuscular metastasis! </br> [Dec 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotmDec2018_fig4a.jpg)
![Don’t forget about the intramuscular metastasis! </br> [Dec 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotmDec2018_4b.jpg)
![Don’t forget about the intramuscular metastasis! </br> [Dec 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotmDec2018_fig5a.jpg)
![Don’t forget about the intramuscular metastasis! </br> [Dec 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotmDec2018_fig5b.jpg)
