- European Federation of Societies for Ultrasound in Medicine and Biology ~ Educating all for competence to practice ultrasound safely
Liver Elastography
September 7, 2017
Multimodal endoscopic ultrasound of a woman with multiple pancreatic lesions [Oct 2017]
October 12, 2017Splenosis mimicking peritoneal metastasis
1 Medizinische Klinik 2, Caritas-Krankenhaus Bad Mergentheim 2 Department of Radiology, Caritas-Krankenhaus Bad Mergentheim
We present a case of a 69-year-old male patient, who was admitted with pneumonia. The initial abdominal ultrasound performed in the admission room demonstrated presence of an oval structure in the left epigastrium, the nature and origin of which was difficult to define. Apart from a postsurgical scar in the left upper abdominal quadrant, physical examination of the patient demonstrated no abnormal findings. The patient had no family history or related diseases. He had a history of splenectomy following abdominal trauma 40 years ago. Laboratory testing including tumor markers demonstrated no abnormalities apart from raised C-reactive protein (CRP) as a sign of inflammation secondary to the pneumonia.
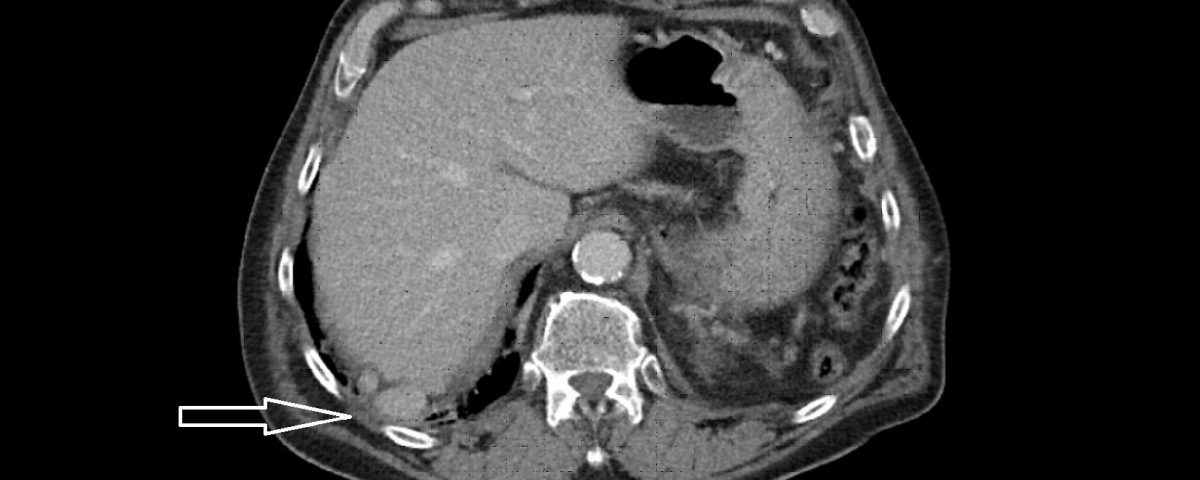
Computed tomography of the abdomen demonstrated no spleen and numerous small nodules of up to 28 mm between intestinal loops and between the liver and diaphragm suggesting a disseminated neoplastic process, thought to be most probably, peritoneal carcinomatosis. The arrow on the scan illustrates the lesion that was biopsied which excluded neoplasia and demonstrated splenic tissue.
Computed tomography of the chest revealed pneumonic infiltration but was otherwise normal. The endoscopic examination of the upper and lower gastrointestinal tract was normal. Contrast enhanced ultrasound (CEUS) showed arterial and late phase enhancement lasting more than 5 minutes in all examined nodules. After Biopsy the ultrasound examination was performed showing multiple almost echofree but also echogenic round and oval shaped focal peritoneal masses with a size of up to 46 mm [Figure 2-4].
Splenosis is a rare disease caused by autotransplantation of splenic cells [1]. The first description of splenosis was described by H. Albrecht in 1886 [2]. The term ‘splenosis’ was used for the first time by Buchbinder and Lipkoff in 1939 [3]. The majority of cases of splenosis are reported after traumatic splenectomies and only few after elective splenectomies performed in the course of hematological diseases [1]. Incidentally discovered splenosis may occur in any location of the abdominal cavity. In rare circumstances and depending on the location, splenosis may trigger various symptoms. The most frequent symptoms of abdominal splenosis include abdominal pain, gastrointestinal bleeding [4] and intestinal obstruction [5]. Thoracic splenosis has been reported to cause hemoptysis. Other rare locations of splenosis reported include subcutaneous tissue [6] and the occipital lobe [7]. Imaging findings including CT and magnetic resonance imaging (MRI) may be misleading not taking into account the various locations of splenotic nodules.
Contrast enhanced ultrasound (CEUS) was performed late in the diagnostic process but showed indicative signs of splenic tissue. The CEUS features that are suggestive of splenic tissue are heterogenous arterial enhancement (zebra phenomenon) and long lasting enhancement without wash out lasting for more than four minutes. The findings are in accordance with the guidelines of the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) [8] excluding metastates with typical early washout [9].
- 1. Ksiadzyna D., Peña A. S. Abdominal splenosis. Revista Espanola de Enfermedades Digestivas. 2011;103(8):421–426.
- 2. Albrecht H. Ein Fall von Zahlreichen, uber ganze Peritoneum versprungtent Nebenmilzer. Beitr Path Anat 1896; 20: 513.
- 3. Buchbinder J. H., Lipkoff C. J. Splenosis: multiple peritoneal splenic implants following abdominal injury. Surgery. 1939;6(6):927–934.
- 4. Arroja B, Almeida N, Macedo CR, Moreira AP, Oliveira P, Tomé L. et al. Gastric splenosis: a rare cause of digestive bleeding. Rev Esp Enferm Dig. 2011;103:377-8
- 5. Gincu V, Kornprat P, Thimary F, Jahn S, Mischinger HJ. Intestinal obstruction caused by splenosis at the rectosigmoid junction, mimicking malignant pelvic tumor. Endoscopy. 2011;43(Suppl 2):E260
- 6. Yeh CJ, Chuang WY, Kuo TT. Case report: unusual subcutaneous splenosis occurring in a gunshot wound scar: pathology and immunohistochemical identification. Pathol Int 2006; 56: 336-9.
- 7. Rickert CH, Maasjosthusmann U, Probst-Cousin S, et al. A unique case of cerebral spleen. Am J Surg Pathol 1998; 22: 894-6.
- 8. Piscaglia F, Nolsøe C, Dietrich CF, et al. The EFSUMB guidelines and recommendations on the clinical practice of contrast enhanced ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med 2012; 33: 33–59.
- 9. Asha Omar, Simon Freeman, Contrast-enhanced ultrasound of the spleen, Ultrasound. 2016 Feb; 24(1): 41–49. Published online 2016 Jan 14.
Figure 2: B-mode ultrasound of the abdominal lesion(s). The largest and almost echofree lesion (46 mm) was identified.
Figure 3: The same lesion as shown in Figure 2. Contrast enhanced ultrasound revealed arterial (a) and late phase enhancement lasting > 4 minutes (b).
Figure 4: At different abdominal locations more echogenic round oval lesions upt to 30 mm were identified by ultrasound. The lesions were best depicted during the late phase enhancement behind the accessory spleen next to the lesion shown in figure 2 (a) and elsewhere in the abdomen (b). The Figure 3c represents the CT finding shown in figure 1.
Med. Klinik 2, Caritas-Krankenhaus Bad Mergentheim
Uhlandstr. 7, D-97980 Bad Mergentheim, Germany
Tel: 49 (0)7931 - 58 - 2201 / 2200
Fax: 49 (0)7931 - 58 - 2290
Christoph.dietrich@ckbm.de


![Splenosis mimicking peritoneal metastasis</br> [Sep 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_sept2017_fig1a.jpg)
![Splenosis mimicking peritoneal metastasis</br> [Sep 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_sept2017_fig1b.jpg)
![Splenosis mimicking peritoneal metastasis</br> [Sep 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_sept2017_fig2.jpg)
![Splenosis mimicking peritoneal metastasis</br> [Sep 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_sept2017_fig3a.jpg)
![Splenosis mimicking peritoneal metastasis</br> [Sep 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_sept2017_fig3b.jpg)
![Splenosis mimicking peritoneal metastasis</br> [Sep 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_sept2017_fig4a.jpg)
![Splenosis mimicking peritoneal metastasis</br> [Sep 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_sept2017_fig4b.jpg)
![Splenosis mimicking peritoneal metastasis</br> [Sep 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm_sept2017_fig4c.jpg)
