Multimodal endoscopic ultrasound of a woman with multiple pancreatic lesions [Oct 2017]
October 12, 2017Update on CEUS Non Liver Guidelines
December 8, 2017Ultrasonographic approach to dysphagia
A female patient in her early thirties suffers from long standing dysphagia, started at the age of 18 years. The symptoms became more intense, accompanied by shortness of breath. Furthermore, the patient developed an anxiety disorder requiring regular psychiatric support.
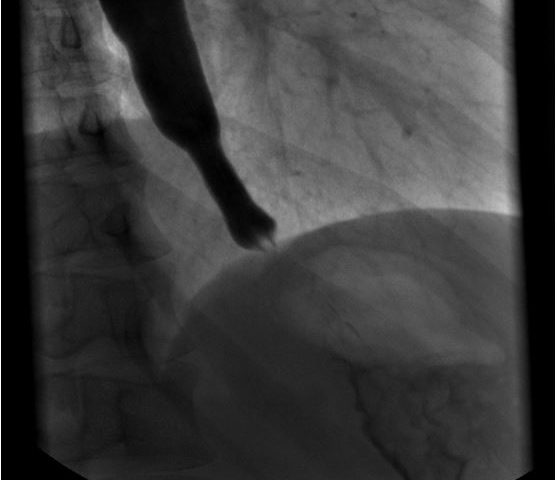
The clinical examination showed a patient in good general health condition with a BMI of 20 (kg/m2). The inspection of the throat and the oral cavity has not shown any pathologic findings. The most frequent triggers of dysphagia in the age group of 20-49 years [2,3] are due to mechanical obstruction (median neck cyst, nasopharyngeal carcinoma, disorders of the thyroid gland, etc.), autoimmune/inflammatory diseases (eosinophilic esophagitis, inflammatory myopathy, Sjögren’s syndrome, throat infection, etc.), esophageal dysmotility (achalasia, nutcracker esophagus, multiple sclerosis, etc.) and others (gastro esophageal reflux, anxiety disorder, heterotopic gastric mucosa, etc.).The first diagnostic procedure performed was an esophagogastroduodenoscopy with no major pathological findings, except for candida infection. The patient then proceeded to an esophageal passage with a barium swallow that showed an enlargement of the distal esophagus up to 3 cm (Figure 1). For various reasons no further diagnostic steps were performed with the diagnosis being made that this was psycho-functional. As the dysphagia was deteriorating, the patient attended our clinic to get an ultrasound examination of her neck which showed an impressive dilatation in the left lower neck area during the swallowing act, consistent with a dilatation of the lower esophagus (Figure 2, video-clip). This finding was confirmed by the subsequent esophageal manometry that was consistent with a congenital achalasia of type 2 according to the Chicago classification (figure 3).
Since then, repeated endoscopic pneumatic dilatations of the lower esophageal sphincter have been successful, maintaining the relief of long lasting symptoms.
The symptoms of achalasia may be misdiagnosed for years due to complex background patterns.
2. Pandolfino JE, Gawron AJ: Achalasia: a systematic review. JAMA 2015; 313: 1841–1852.
3. Roden DF, Altman KW: Causes of dysphagia among different age groups: a systematic review of the literature. Otolaryngol Clin North Am 2013; 46: 965–987.
Figure 2: Ultrasound (linear 9 MHz probe): during swallowing shows a 3 cm, sickle-shaped and hyperreflective structure consistent with a dilatation of the lower esophagus.
Figure 3: Esophageal manometry: consistent with pressure ratios typical for achalasia type 2 according to the Chicago- Classification, with missing slackening of the lower esophageal sphincter and aperistaltic contractions


![Ultrasonographic approach to dysphagia</br> [Nov 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm2017-november-fig1.jpg)
![Ultrasonographic approach to dysphagia</br> [Nov 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm2017-november-fig2.jpg)
![Ultrasonographic approach to dysphagia</br> [Nov 2017]](https://efsumb.org/wp-content/uploads/2020/11/cotm2017-november-fig3.jpg)
