
ALBANIA – AUA
September 21, 2020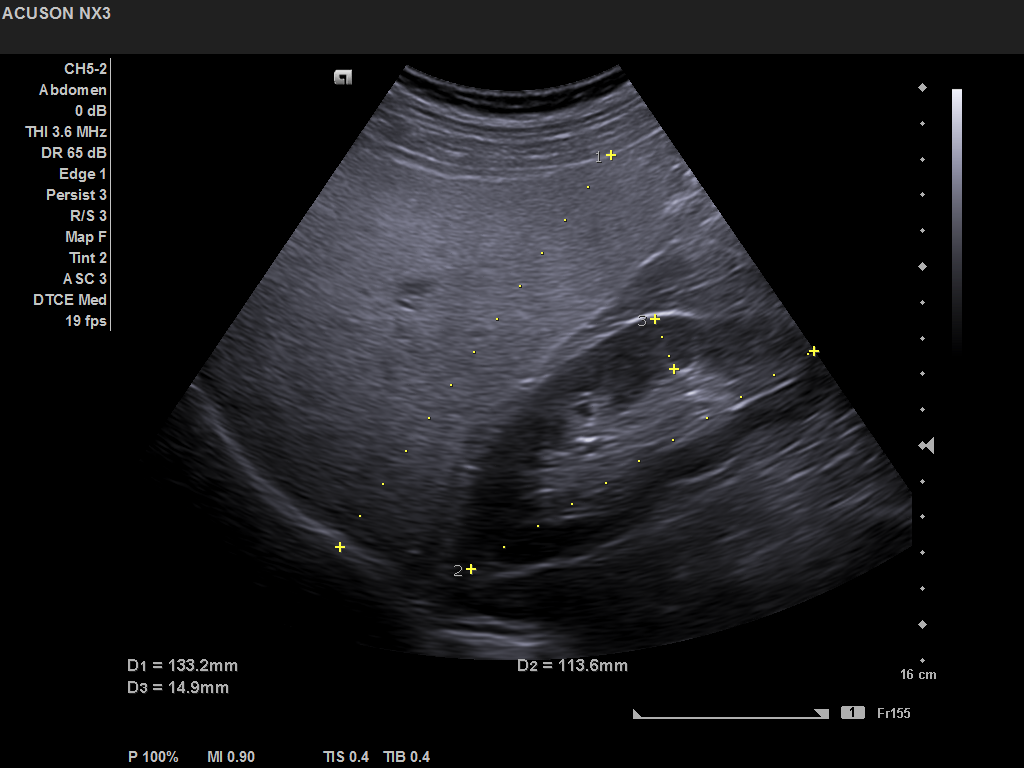
Student Image Challenge 68
October 8, 2020Ultrasound findings in Actinomyces infection of the neck
Anja Brosig, Christopher Bohr, Julian Künzel
Department of Otorhinolaryngology, University Hospital of Regensburg, Germany
Franz-Josef-Strauß-Allee 11
93053 Regensburg
Germany
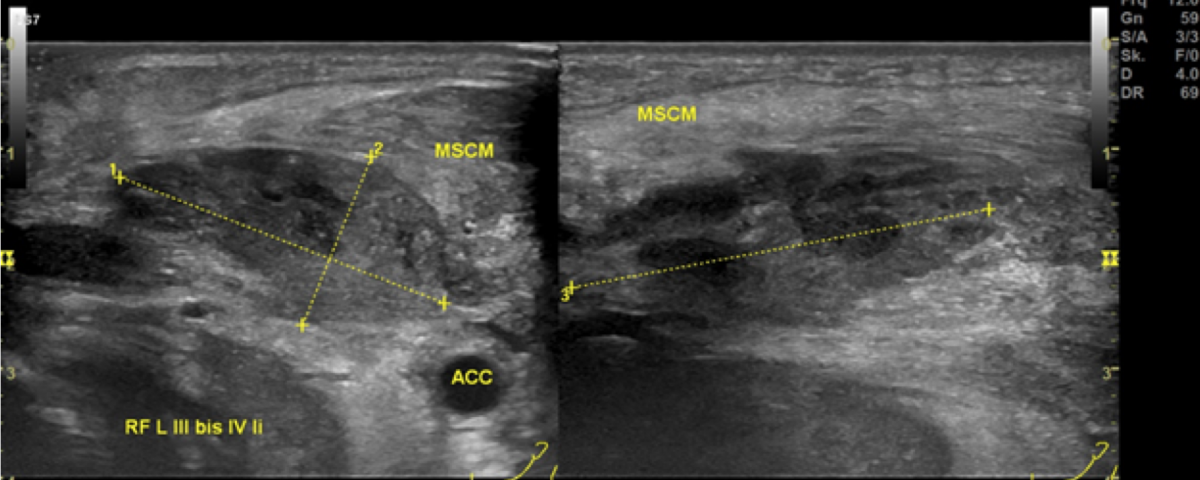
Preoperative ultrasonographic findings showed an oval hypoechoic inhomogeneous mass, approximately 4 x 3 x 1.5 cm in levels III to IV of the left side of the neck below the sternocleidomastoid muscle. (Fig. 1) The mass was partly indistinct to the adjacent tissue and demonstrated peripheral perfusion with no central vascularity. (Fig. 2) The surrounding soft tissues appeared oedematous and thickened. (Fig. 1 – 2)
Figure 1. Hypoechoic inhomogeneous mass partly indistinct from the adjacent tissue in Levels III to IV of the left neck; ACC = Common carotid artery; MSCM = sternocleidomastoid muscle.
Sonographic check 2.5 weeks after start of treatment
Figure 7. Status after 2,5 weeks of i.v. antibiotic therapy and drainage. The fluid formation in the left thyroid lobe (sd li) has resolved. The infrahyoid muscle (ihm) and the sternocleidomastoid muscle (mscm) are still mildly thickened. The drain is still in place (lasche in situ). acc = Common carotid artery.
An incision of the lymph node collection was carried out on the day of admission and a drain inserted. Histopathologically there was a purulent abscess and chronic-granular inflammation with evidence of actinomycete glands.
Microbiological tests showed no evidence of tuberculosis, toxoplasmosis, Bartonella or MOTT. Although there was no microbiological detection of actinomycetes, an actinomycete infection was assumed.
The patient received intravenous antibiotic therapy with amoxicillin /clavulonic acid for 3 weeks. During the course, a MRI of the neck was performed, which showed residual fluid in the former abscess cavity and another fluid collection in the left thyroid lobe, which appeared to be in contact. (Fig. 5) A sonographic check showed an echo-poor area around the left thyroid lobe corresponding to the MRI findings (Fig. 6). Owing to these findings and continued secretions from the wound area, revision surgery with wound drainage was carried out. Healing and improvement was confirmed on a subsequent sonographic check. (Fig. 7)
The antibiotic therapy was then oralized and the patient was discharged after three weeks in hospital. The total duration of antibiotic treatment was 8 weeks.
A distinction is made between acute, subacute and chronic forms of actinomycosis. While acute actinomycetes infection usually result in soft tissue swelling or abscess formation, patients with a long history of illness usually develop painless, coarse masses that can also form fistulas with drainage channels to the skin. (4)
2. Schaal K.P., Lee H.J. Actinomycete infections in humans--a review. Gene. 1992;115:201–211.
3. Moghimi M., Salentijn E., Debets-Ossenkop Y., Karagozoglu K.H., Forouzanfar T. Treatment of cervicofacial actinomycosis: A report of 19 cases and review of literature. Med. Oral Patol. Oral Cir. Bucal. 2013;18:e627–e632.
4. Heo SH, Shin SS, Kim JW, et al. Imaging of actinomycosis in various organs: a comprehensive review. Radiographics 2014;34:19-33.
5. Lancella A., Abbate G., Foscolo A.M., Dosdegani R. Two unusual presentations of cervicofacial actinomycosis and review of the literature. Acta Otorhinolaryngol. Ital. 2008;28:89–93.
6. Park JK, Lee HK, Ha HK, Choi HY, Choi CG. Cervicofacial actinomycosis: CT and MR imaging findings in seven patients. AJNR Am J Neuroradiol 2003;24:331-5.
7. Stájer A, Ibrahim B, Gajdács M, Urbán E, Baráth Z. Diagnosis and Management of Cervicofacial Actinomycosis: Lessons from Two Distinct Clinical Cases. Antibiotics (Basel). 2020 Mar 25;9(4).


![Ultrasound findings in Actinomyces infection of the neck </br> [Aug/Sep 2020]](https://efsumb.org/wp-content/uploads/2020/11/cotmaug2020-fig01.png)
![Ultrasound findings in Actinomyces infection of the neck </br> [Aug/Sep 2020]](https://efsumb.org/wp-content/uploads/2020/11/cotmaug2020-fig02.png)
![Ultrasound findings in Actinomyces infection of the neck </br> [Aug/Sep 2020]](https://efsumb.org/wp-content/uploads/2020/11/cotmaug2020-fig03.png)
![Ultrasound findings in Actinomyces infection of the neck </br> [Aug/Sep 2020]](https://efsumb.org/wp-content/uploads/2020/11/cotmaug2020-fig04.png)
![Ultrasound findings in Actinomyces infection of the neck </br> [Aug/Sep 2020]](https://efsumb.org/wp-content/uploads/2020/11/cotmaug2020-fig05.png)
![Ultrasound findings in Actinomyces infection of the neck </br> [Aug/Sep 2020]](https://efsumb.org/wp-content/uploads/2020/11/cotmaug2020-fig06.png)
![Ultrasound findings in Actinomyces infection of the neck </br> [Aug/Sep 2020]](https://efsumb.org/wp-content/uploads/2020/11/cotmaug2020-fig07.png)
