Student Image Challenge 92
May 21, 2021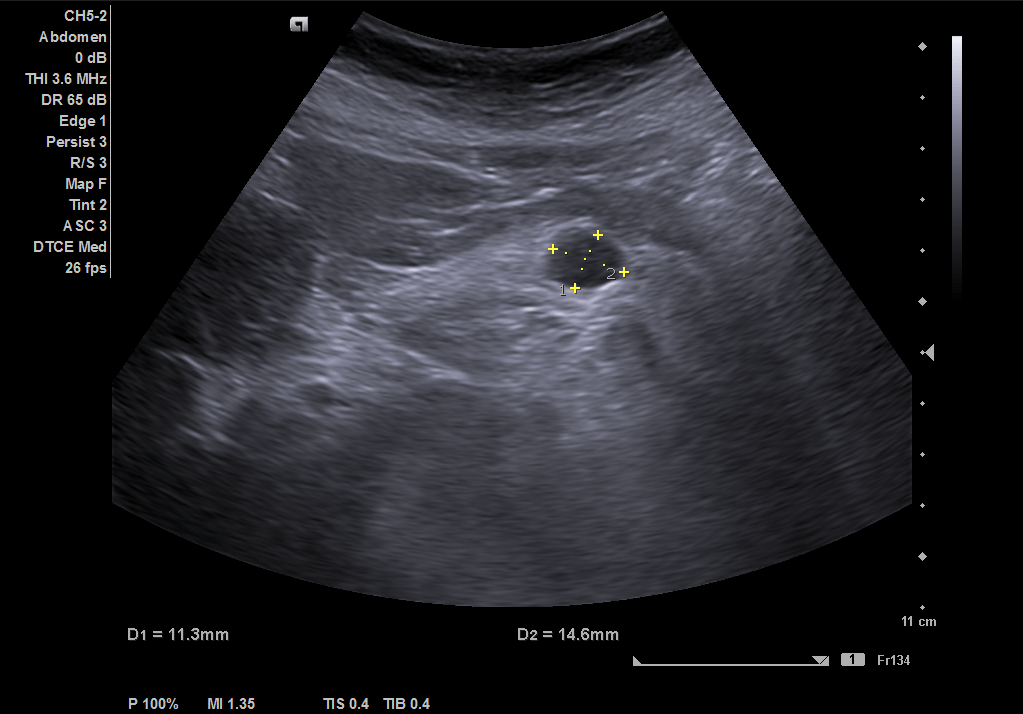
Student Image Challenge 93
June 7, 2021Ultrasound of an ileocecal intussusception in a 12-month-old boy [June 2021]
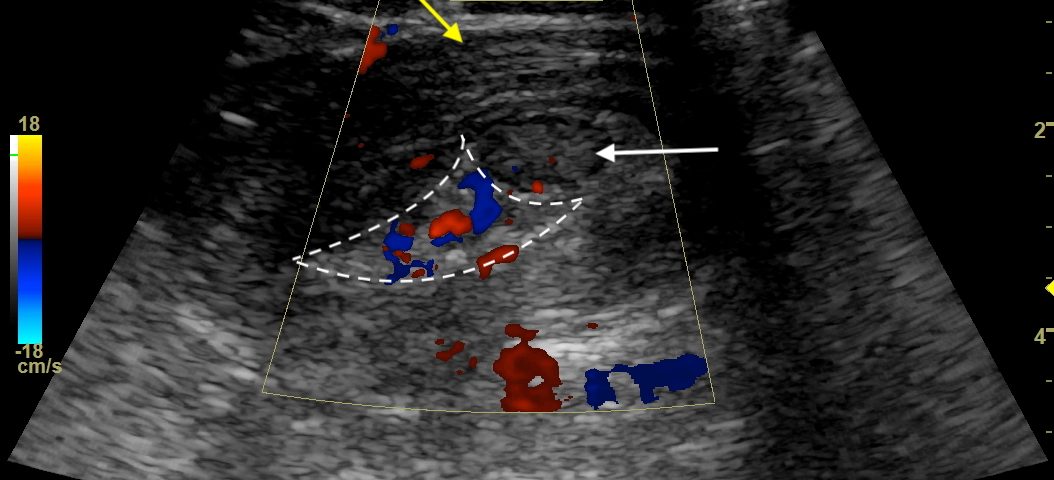
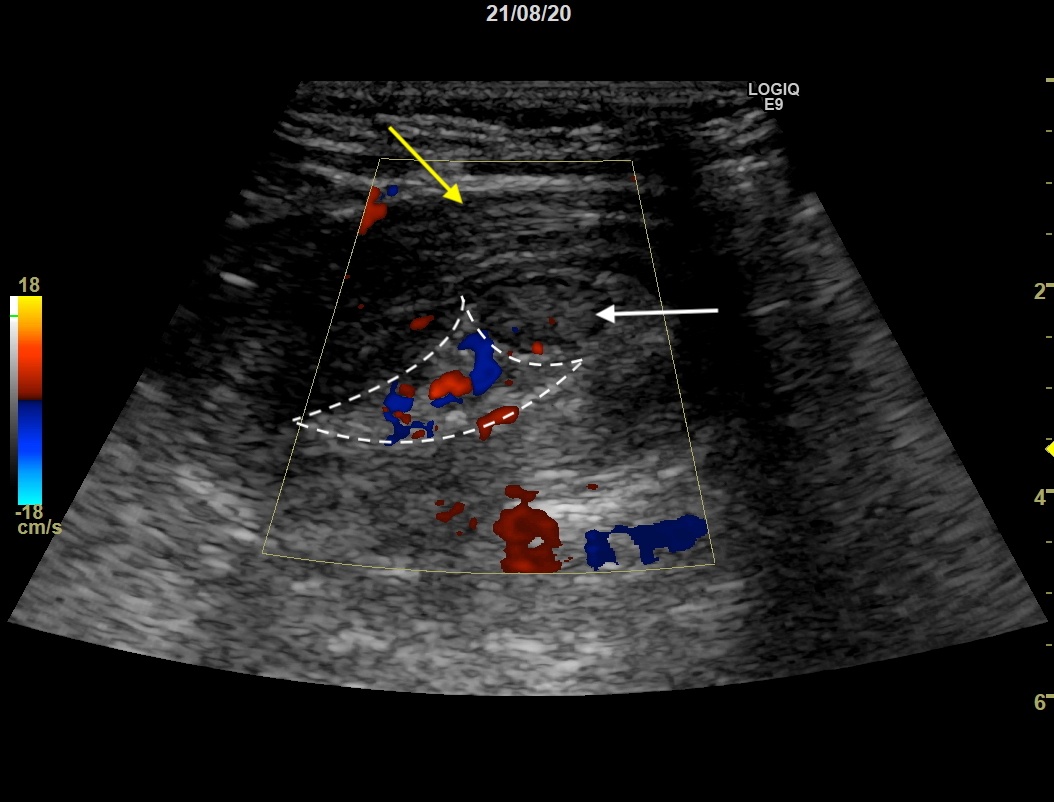
Figure 2: Color Doppler showed vascularization of the bowel walls in the intussusception. Yellow arrow: The outer layers representing the intussuspiens bowel wall (colon) and lumen. White arrow: The inner layers representing the intussusceptum/telescoping bowel (ileum). Dashed white line: Mesenteric fat.
Ultrasound of an ileocecal intussusception in a 12-month-old boy
Sair Ahmad Nissar Anjum and Maryam Mozaffari
Department of Radiology
Copenhagen University Hospital
Denmark
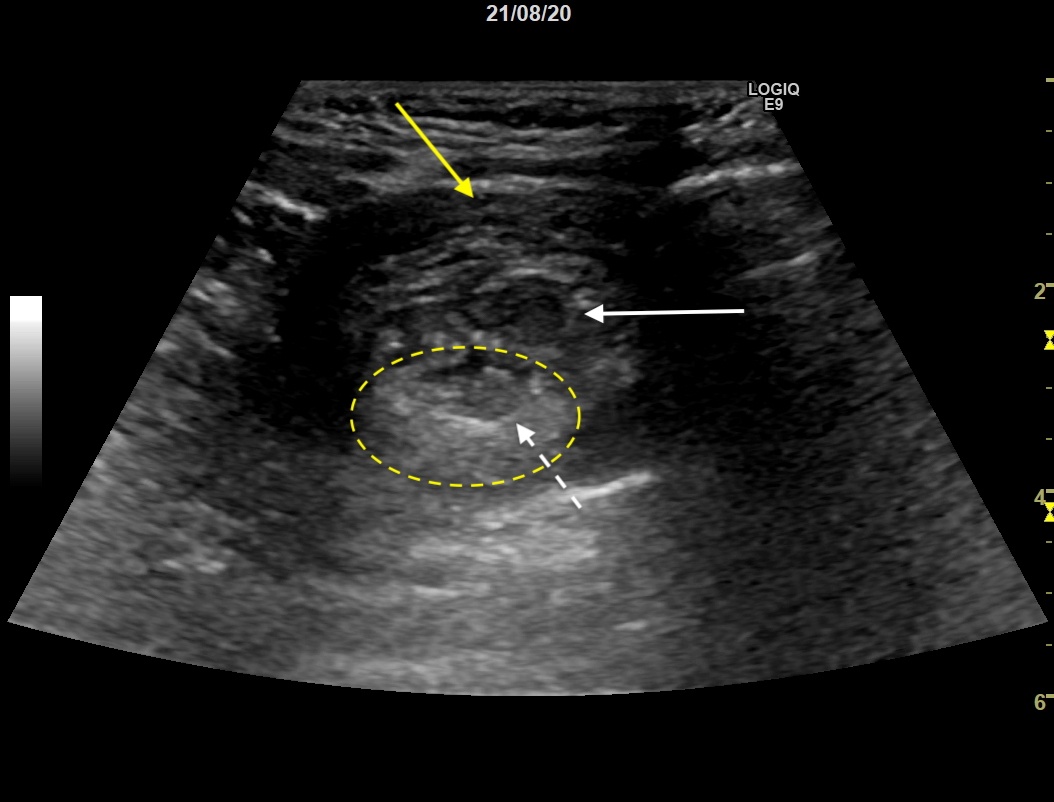
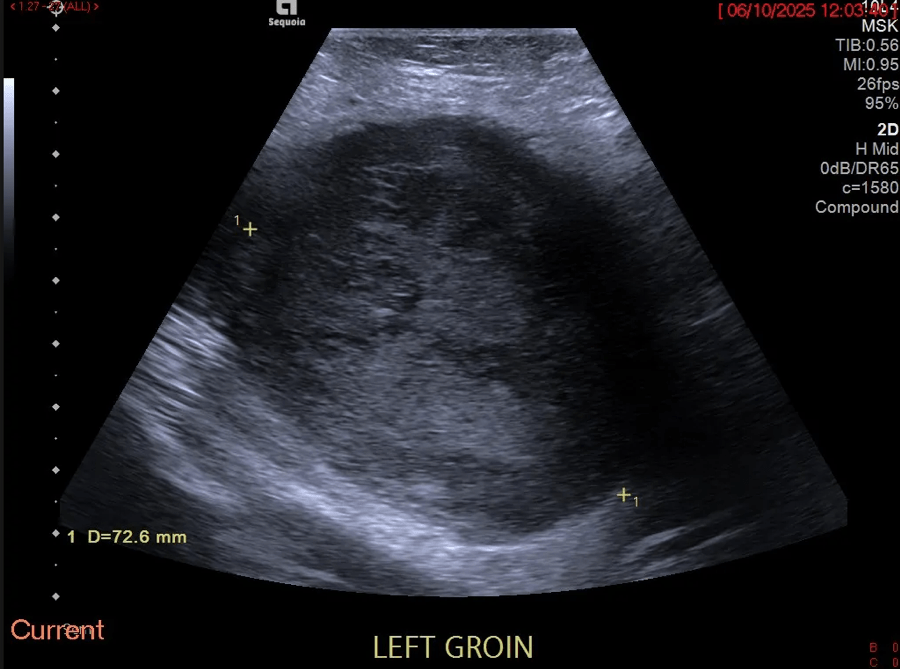
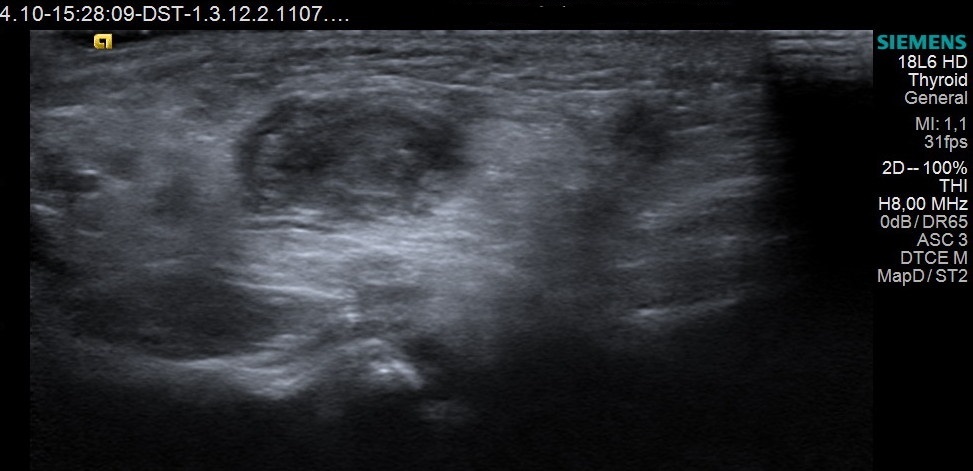
Figure 1: Transverse image showing the doughnut sign. Yellow arrow: The outer layers representing the intussuspiens bowel wall (colon) and lumen. White arrow: The inner layers representing the intussusceptum/telescoping bowel (ileum). Dashed yellow line: Mesenteric fat. Dashed white arrow: Lymph node within mesenteric fat.
Figure 2: Color Doppler showed vascularization of the bowel walls in the intussusception. Yellow arrow: The outer layers representing the intussuspiens bowel wall (colon) and lumen. White arrow: The inner layers representing the intussusceptum/telescoping bowel (ileum). Dashed white line: Mesenteric fat.
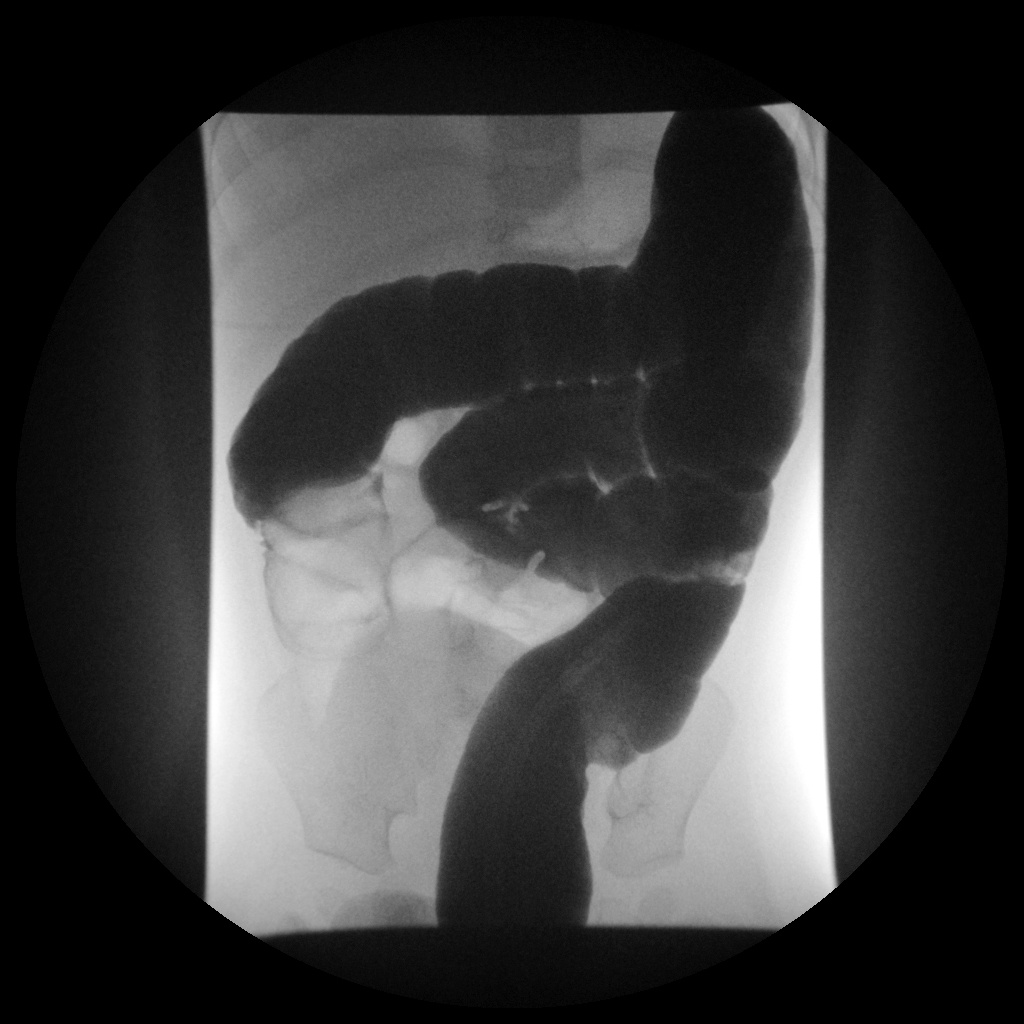
Eventually, laparoscopy was performed and the remaining intussusceptum, consisting of cecum, appendix and approximately 5 cm of the terminal ileum was reduced without any complications. The patient was discharged 2 days later in good health.
It is the most common cause of intestinal obstruction in children between 3 months and 3 years, second only to appendicitis as the most common cause of an acute abdominal emergency in children (3). Approximately 60% of children with intussusception are younger than 1-year-old and 80–90% are younger than 2 years. Approximately 10 percent of cases occur in children older than 5 years. 3–4% occur in those older than 10 years, and 1% in infants younger than 3 months (5).
In infants the most common type of intussusception is ileocolic accounting for 90% (2, 6). This is often an idiopathic condition presumably caused by lymphoid hyperplasia following a viral or other enteric infection (1). Intussusception occurring before and after the typical age range is likely to be associated with a pathologic lead point and has been reported to occur in approximately 5–6% of intussusceptions. These are due to either focal masses or diffuse abnormality in the bowel wall. The most common focal pathological lead points are Meckel’s diverticulum, duplication cyst, polyp and lymphoma. Diffuse abnormalities causing intussusception are often cystic fibrosis or Henoch–Schönlein Purpura (1).
The classic symptoms are acute colicky abdominal pain, red currant jelly stool, vomiting, and a palpable abdominal mass or emesis. Especially infants may initially only present with lethargy and irritability. The variability of the presenting symptoms can make the diagnosis challenging (4). A delay in diagnosis can result in bowel ischemia, perforation, and increased need for surgical intervention.
Ultrasound is considered the modality of choice for the diagnosis of pediatric intussusception due to its accuracy and lack of ionizing radiation. The accuracy of ultrasound to rule out intussusception is close to 100% (1). A doughnut, pseudokidney, or target sign is a diagnostic finding representing layers of the intestine within the intestine (1, 7). The crescent in a donut sign is also seen and represents the echogenic mesenteric fat that wraps around the mesenteric border of the intussuscepted intestine, forming the crescent. Occasionally, reactive lymphadenopathy can be identified within the involved mesentery (8).
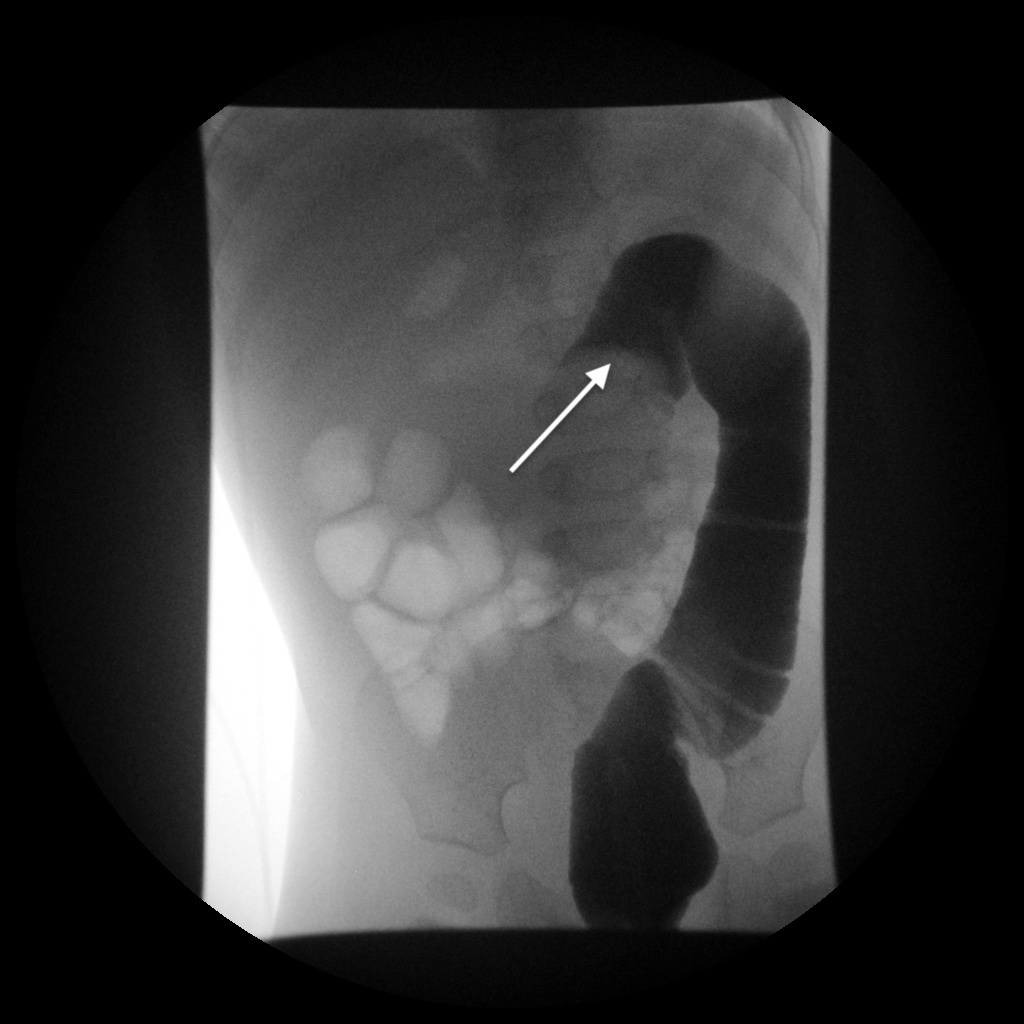
In stable children without signs of peritonitis, the preferred treatment is intravenous fluid resuscitation followed by a reduction enema, which can be done with either water-soluble contrast agent or air. The average reduction rate is 74% (1). Prior to that, every child should undergo a surgical consultation to assess for peritonitis or perforation, which precludes enema. Children with evidence of shock, sepsis or free air on abdominal radiographs are not candidates for enema either.
In cases where the enema is unsuccessful surgery is performed to prevent bowel ischemia and possible perforation.
• The most common type of intussusception is ileocolic and predominantly occurs in children younger than 2 years old.
• The classic symptoms can be acute colicky abdominal pain, red currant jelly stool, vomiting, a palpable abdominal mass, emesis, lethargia or irritability.
• Ultrasound has a high diagnostic accuracy for intussusception and should be the method of choice.
2. Mandeville K, Chien M, Willyerd FA, Mandell G, Hostetler MA, Bulloch B. Intussusception: clinical presentations and imaging characteristics. Pediatr Emerg Care. 2012;28(9):842-4.
3. Waseem M, Rosenberg HK. Intussusception. Pediatr Emerg Care. 2008;24(11):793-800.
4. Lin-Martore M, Kornblith AE, Kohn MA, Gottlieb M. Diagnostic Accuracy of Point-of-Care Ultrasound for Intussusception in Children Presenting to the Emergency Department: A Systematic Review and Meta-analysis. West J Emerg Med. 2020;21(4):1008-16.
5. Thomas T Sato NV. Intussusception in children Uptodate2020 [cited 2020 20.september 2020]. Available from: https://www.uptodate.com/contents/intussusception-in-children?search=intussusception in children&source=search_result&selectedTitle=1~115&usage_type=default&display_rank=1 - H4154394222.
6. Bartocci M, Fabrizi G, Valente I, Manzoni C, Speca S, Bonomo L. Intussusception in childhood: role of sonography on diagnosis and treatment. J Ultrasound. 2015;18(3):205-11.
7. Hryhorczuk AL, Strouse PJ. Validation of US as a first-line diagnostic test for assessment of pediatric ileocolic intussusception. Pediatr Radiol. 2009;39(10):1075-9.
8. Yu ML, Lee KH, Li YL. The crescent-in-doughnut sign in intussusception. Abdom Radiol (NY). 2018;43(5):1266-7.