A rare cause for delayed renal transplant graft function [Jul 2018]
July 13, 2018GIUS
September 13, 2018Gallbladder Perforation and hepatic abscess formation in Advanced Cholecystitis: CEUS as an Adjunct
Authors
Mr Stephen Moore:Sonographer; Princes Royal University Hospital: King’s College NHS Foundation Trust
s.moore11@nhs.net
Dr Gibran Yusuf;
Consultant Radiologist Princes Royal University Hospital: King’s College NHS Foundation Trust
Gibran.yusuf@nhs.net
Mrs Janine Sawyer:
Sonographer; King’s College Hospital NHS Foundation Trust
janinesawyer@nhs.net
Professor Paul Sidhu;
Professor of Radiology King’s College Hospital NHS Foundation Trust
paulsidhu@nhs.net
Corresponding Author: Stephen Moore s.moore11@nhs.net Postal Address for Authors: King’s College Hospital, Denmark Hill, London, SE5 9RS Princess Royal University hospital, Farnborough Common, Orpington, Kent BR6 8ND
1Abstract
Gallbladder perforation and hepatic abscess formation are rare complications of acute cholecystitis with high mortality rates (1). Ultrasound is the imaging modality of choice for patients presenting with right upper quadrant (RUQ) pain in the acute setting (2,3). However, B-mode ultrasound falls short of confidently diagnosing gallbladder wall defects (3) which are essential for facilitating a diagnosis of gallbladder perforation. We present a case where CEUS unequivocally diagnosed gallbladder wall perforation and hepatic abscess formation
2Keywords
Contrast Enhanced Ultrasound, CEUS, Gallbladder, Perforation, Defect, Acute Cholecystitis, Hepatic, Abscess, Ultrasound, EFSUMB
3Case Report
A 74-year-old male presented in the emergency department with clinical evidence of generalised sepsis. Clinical examination revealed a soft non-tender abdomen with a history of normal bowel movements. A preliminary clinical diagnosis of community acquired pneumonia was made based on CXR appearances of consolidation. Biochemistry demonstrated acute kidney injury (AKI) and severely deranged liver function tests (LFT). An ultrasound of the abdomen was undertaken.
B-mode ultrasound demonstrated complicated gallstones with low level echogenic debris within the gallbladder. The gallbladder wall was thickened and ill-defined anteriorly (Figure 1). Within segment V of the liver, adjacent the anterior gallbladder wall was an ill-defined hypoechoic lesion containing complex fluid components, these findings were suggestive of a hepatic abscess. A second larger hepatic abscess was noted in segments V/VIII (Figure 2).
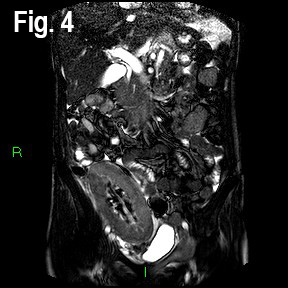
A Bolus of 2.4ml of SonoVue (Bracco, Milan) was administered through a cannula situated in the left antecubital fossa, followed by a 10ml bolus of saline solution. Both abscesses demonstrated peripheral enhancement with no uptake seen in the central fluid components (Figure 3). On further evaluation of the anterior gallbladder wall CEUS demonstrated a well-defined avascular defect providing a communication of the gallbladder contents with the adjacent hepatic abscess (Figure 4). These findings were conclusive of gallbladder wall perforation. A subsequent Computed Tomography confirmed this gallbladder perforation and hepatic abscess formation within segments V and V/VIII of the liver.
B-mode ultrasound demonstrated complicated gallstones with low level echogenic debris within the gallbladder. The gallbladder wall was thickened and ill-defined anteriorly (Figure 1). Within segment V of the liver, adjacent the anterior gallbladder wall was an ill-defined hypoechoic lesion containing complex fluid components, these findings were suggestive of a hepatic abscess. A second larger hepatic abscess was noted in segments V/VIII (Figure 2).
A Bolus of 2.4ml of SonoVue (Bracco, Milan) was administered through a cannula situated in the left antecubital fossa, followed by a 10ml bolus of saline solution. Both abscesses demonstrated peripheral enhancement with no uptake seen in the central fluid components (Figure 3). On further evaluation of the anterior gallbladder wall CEUS demonstrated a well-defined avascular defect providing a communication of the gallbladder contents with the adjacent hepatic abscess (Figure 4). These findings were conclusive of gallbladder wall perforation. A subsequent Computed Tomography confirmed this gallbladder perforation and hepatic abscess formation within segments V and V/VIII of the liver.
4Discussion
Gallbladder perforation and hepatic abscess formation are rare complications of cholecystitis confounded further by non-specific clinical and biochemical presentations (4,5). These dilemmas can cause delays in emergency treatment, resulting in significant mortality rates of up to 70% (1). We present a case where CEUS unequivocally confirmed perforation of the gallbladder wall. CEUS was the preferred initial imaging modality, due to its non-nephrotoxic nature (2,6) in a patient with AKI.
Although ultrasound is the modality of choice when imaging the acutely unwell patient with RUQ pain and deranged LFT (2,3). B-mode ultrasound is known to lack the sensitivity and specificity needed to detect gallbladder wall defects. This is essential to facilitate a diagnosis of gallbladder wall perforation. One study documented the B-mode sensitivity and specificity of gallbladder wall interruption to be 12.8 % and 100% respectively; the addition of micro-bubble contrast agents brought the sensitivity and specificity up to 78% and 85% respectively (3).
CEUS with its purely intravascular nature and exceptionally high spatial and temporal resolution (2,6) is a useful adjunct to B-mode ultrasound in cases of suspected gallbladder perforation (1). The use of contrast allows clear delineation of the avascular defect caused by the discontinuity of the gallbladder wall. Gallbladder wall defects are easily appreciated both on real-time and static imaging.
It is hypothesised that CEUS has the potential to reduce mortality risks by increasing confidence in the ability of ultrasound to diagnose gallbladder perforation despite challenging clinical presentations (1,3). This case demonstrates how CEUS can facilitate a rapid diagnosis in a time critical setting ensuring patient safety.
CEUS is well documented for the characterisation of hepatic abscesses (2,6,7). This case demonstrates classical features in keeping with the evidence-based literature with respect to both the enhancement patterns and delineation of true fluid aspects of abscesses on CEUS (2,6,7)
Although ultrasound is the modality of choice when imaging the acutely unwell patient with RUQ pain and deranged LFT (2,3). B-mode ultrasound is known to lack the sensitivity and specificity needed to detect gallbladder wall defects. This is essential to facilitate a diagnosis of gallbladder wall perforation. One study documented the B-mode sensitivity and specificity of gallbladder wall interruption to be 12.8 % and 100% respectively; the addition of micro-bubble contrast agents brought the sensitivity and specificity up to 78% and 85% respectively (3).
CEUS with its purely intravascular nature and exceptionally high spatial and temporal resolution (2,6) is a useful adjunct to B-mode ultrasound in cases of suspected gallbladder perforation (1). The use of contrast allows clear delineation of the avascular defect caused by the discontinuity of the gallbladder wall. Gallbladder wall defects are easily appreciated both on real-time and static imaging.
It is hypothesised that CEUS has the potential to reduce mortality risks by increasing confidence in the ability of ultrasound to diagnose gallbladder perforation despite challenging clinical presentations (1,3). This case demonstrates how CEUS can facilitate a rapid diagnosis in a time critical setting ensuring patient safety.
CEUS is well documented for the characterisation of hepatic abscesses (2,6,7). This case demonstrates classical features in keeping with the evidence-based literature with respect to both the enhancement patterns and delineation of true fluid aspects of abscesses on CEUS (2,6,7)
5Conclusion
We demonstrate a case of gallbladder wall perforation where the mural defect was only delineated on CEUS. This technique is a quick and useful adjunct to conventional B-mode ultrasound and can be essential to confirming the diagnosis thus expediting appropriate treatment in these clinically challenging cases.
Drug names and Instrument Names: 2.4 ml SonoVue (Bracco, Milan), 10 ml bolus/ flush of 0.9% sodium chloride saline solution.
Drug names and Instrument Names: 2.4 ml SonoVue (Bracco, Milan), 10 ml bolus/ flush of 0.9% sodium chloride saline solution.
6References
(1) Hutchings, S., Punekar, S., Wolstenhulme, S. (2013) ‘Gallbladder perforation: the hole sign’, Ultrasound, 21(1), pp. 144-147 doi: 10.1177/1742271X13489552
(2) Meacock, L M., Sellars, M E., Sidhu, PS. (2010) ‘Contrast-Enhanced Ultrasound Beyond the Liver: Evaluation of Gallbladder and Biliary Duct Disease Processes’, British Journal of Radiology, 83(991), pp. 615-627 doi: 10.1259/bjr/60619911
(3) Ripollé s, T., Martínez-Pérez, MJ., Martin, G., Viuete, J., Martínez-García, R., Diez, J., Martí, C. (2015) ‘Usefulness of contrast-enhanced US in the diagnosis of acute gangrenous cholecystitis: A comparative study with surgical and pathological findings’, European Journal of Radiology, 85(1), pp. 31-38 doi: http://dx.doi.org/10.1016/j.ejrad.2015.10.010
(4) Tang, S., Wang, Y., Wang, Y. (2013) ‘Contrast-enhanced ultrasonography to diagnose gallbladder perforation’, American Journal of Emergency Medicine, 31(1), pp. 1240-1243 doi: http://dx.doi.org/10.1016/j.ajem.2013.04.034
(5) Chowsey, SR., Baghel, H., Sharma, P., Singh, B. (2013) ‘Diagnosis of Gallbladder Perforation- a Puzzle!’, Indian Journal of Surgery, 76(3), pp. 247-250 doi: 10.1007/s12262-013-0826-3
(6) Huang, DY., Yusuf, GT., Daneshi, M., Husainy MA., Ramnarine, R., Sellars, MEK, Sidhu, PS. (2017) ‘Contrast-enhanced US-guided Interventions: Improving Success Rate and Avoiding Complications Using US Contrast Agents’, Radiographics, 37(2), pp 652-664 doi: 10.1148/rg.2017160123
(7) Sidhu, PS., Cantisani, V., Dietrich, CF., Gilja, OH., Saftoiu, A., Bartels, E., Bertolotto, M., Calliada, F., Clevert, DA., Cosgrove, DO., Deganello, A., D’Onofrio, M., Drudi, FM., Freeman, SJ., Harvey, CJ., Jenssen, C., Jung, EM., Klauser, AS., Lassau, N., Meloni, F., Leen, EL., Nicolau, C., Nolse, CP., Piscaglia, F., Prada, F., Prosch, H., Radzina, M., Savelli, L., Weskott, HP., Wijkstra, H. (2018) ‘The EFSUMB guidelines and recommendations for the clinical practice of contrast enhanced ultrasound (CEUS) in non–hepatic applications. Update 2017 (Long version)’, Ultraschall in der Medizine, 39(2), pp e2-e44 doi: 10.1055/a-0586-1107
(2) Meacock, L M., Sellars, M E., Sidhu, PS. (2010) ‘Contrast-Enhanced Ultrasound Beyond the Liver: Evaluation of Gallbladder and Biliary Duct Disease Processes’, British Journal of Radiology, 83(991), pp. 615-627 doi: 10.1259/bjr/60619911
(3) Ripollé s, T., Martínez-Pérez, MJ., Martin, G., Viuete, J., Martínez-García, R., Diez, J., Martí, C. (2015) ‘Usefulness of contrast-enhanced US in the diagnosis of acute gangrenous cholecystitis: A comparative study with surgical and pathological findings’, European Journal of Radiology, 85(1), pp. 31-38 doi: http://dx.doi.org/10.1016/j.ejrad.2015.10.010
(4) Tang, S., Wang, Y., Wang, Y. (2013) ‘Contrast-enhanced ultrasonography to diagnose gallbladder perforation’, American Journal of Emergency Medicine, 31(1), pp. 1240-1243 doi: http://dx.doi.org/10.1016/j.ajem.2013.04.034
(5) Chowsey, SR., Baghel, H., Sharma, P., Singh, B. (2013) ‘Diagnosis of Gallbladder Perforation- a Puzzle!’, Indian Journal of Surgery, 76(3), pp. 247-250 doi: 10.1007/s12262-013-0826-3
(6) Huang, DY., Yusuf, GT., Daneshi, M., Husainy MA., Ramnarine, R., Sellars, MEK, Sidhu, PS. (2017) ‘Contrast-enhanced US-guided Interventions: Improving Success Rate and Avoiding Complications Using US Contrast Agents’, Radiographics, 37(2), pp 652-664 doi: 10.1148/rg.2017160123
(7) Sidhu, PS., Cantisani, V., Dietrich, CF., Gilja, OH., Saftoiu, A., Bartels, E., Bertolotto, M., Calliada, F., Clevert, DA., Cosgrove, DO., Deganello, A., D’Onofrio, M., Drudi, FM., Freeman, SJ., Harvey, CJ., Jenssen, C., Jung, EM., Klauser, AS., Lassau, N., Meloni, F., Leen, EL., Nicolau, C., Nolse, CP., Piscaglia, F., Prada, F., Prosch, H., Radzina, M., Savelli, L., Weskott, HP., Wijkstra, H. (2018) ‘The EFSUMB guidelines and recommendations for the clinical practice of contrast enhanced ultrasound (CEUS) in non–hepatic applications. Update 2017 (Long version)’, Ultraschall in der Medizine, 39(2), pp e2-e44 doi: 10.1055/a-0586-1107



![Gallbladder Perforation and hepatic abscess formation in Advanced Cholecystitis: CEUS as an Adjunct </br> [Aug 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_auggg002-2018.jpg)
![Gallbladder Perforation and hepatic abscess formation in Advanced Cholecystitis: CEUS as an Adjunct </br> [Aug 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_auggg003-2018.jpg)
![Gallbladder Perforation and hepatic abscess formation in Advanced Cholecystitis: CEUS as an Adjunct </br> [Aug 2018]](https://efsumb.org/wp-content/uploads/2020/11/cotm_auggg004-2018.jpg)
