The role of ultrasound in detection and characterisation of incidental Renal Cell Carcinomas [October 2021]
September 30, 2021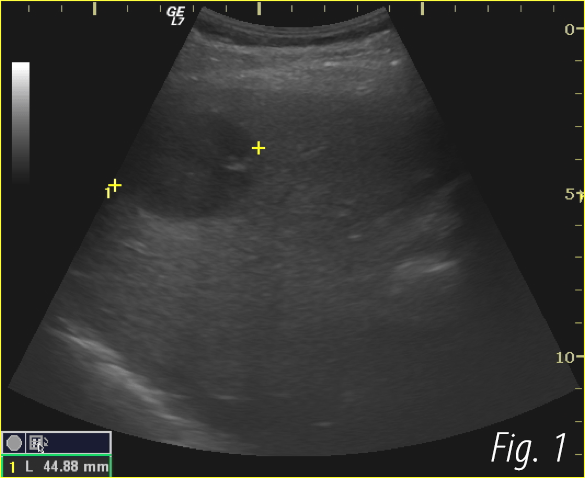
Primary liver lymphoma developed in a patient with chronic hepatitis C [December 2021]
December 9, 2021Non-inflamed stump appendix within the cecum
AUTHOR
Maksym Zhayvoronok
Diagnostic Ultrasound Unit, DP Medbud, Kyiv, Ukraine
Maksym Zhayvoronok
Diagnostic Ultrasound Unit, DP Medbud, Kyiv, Ukraine
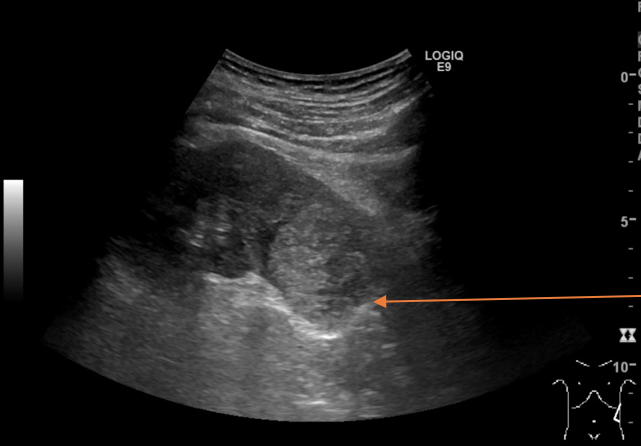
Video1. However, there were no signs of intestinal inflammation. The study showed no increase in vascular blood flow with color Doppler, and there was no free fluid in the abdomen.
1Clinical History
A 40-year-old female presented to our clinic for a routine ultrasound study.
An appendicectomy scar was noted medially. The appendectomy was performed 5 years ago. The patient had not sought medical advice previously.
2Image findings
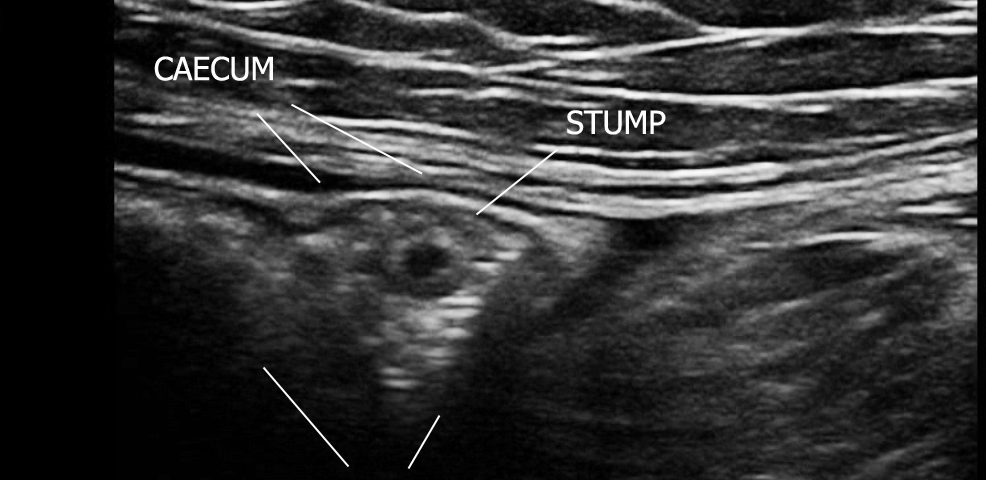
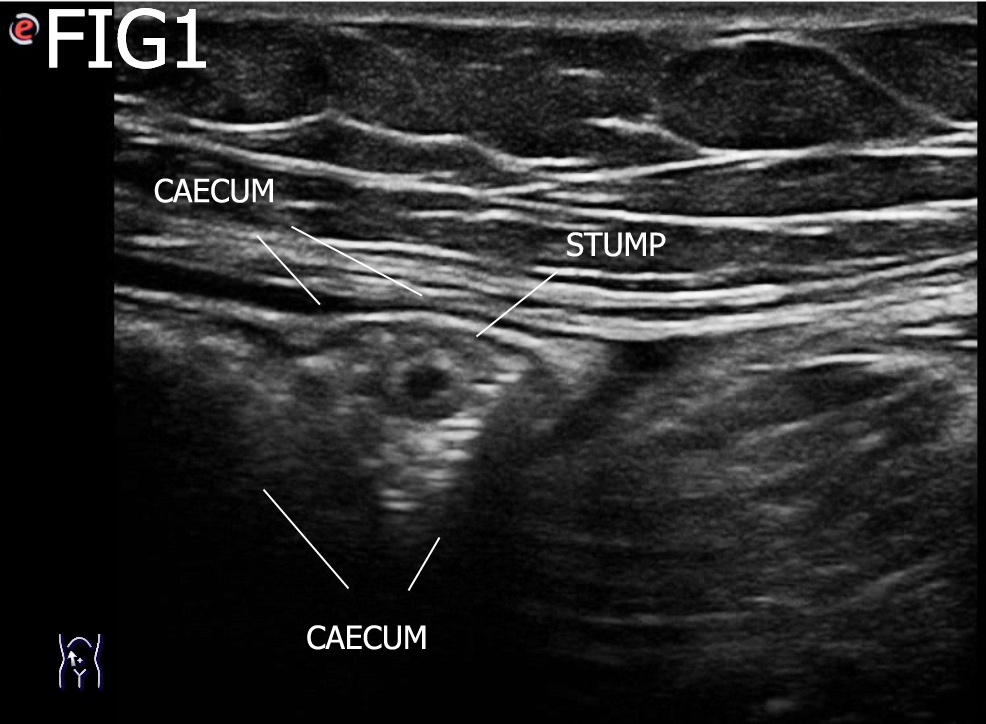
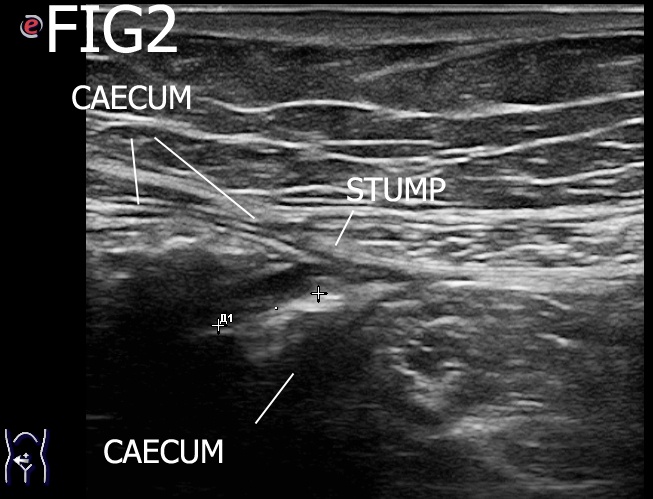
An ultrasound examination of the abdomen was performed using an Esaote MyLabSeven system with a linear array transducer and centre frequency of 13 MHz. The patient was examined in the supine position. The examination revealed a short blind ending tubular structure resembling an appendix but given the history, it was taken to represent a non-inflamed appendix stump. Unusually, this was located inside the lumen of the cecum. The stump was 6 x 8 mm in size and had a characteristic layered structure. There was no soreness or ultrasound signs of inflammation.
3Diagnosis
The findings were consistent with a non-inflamed stump appendix within the cecum.
4Discussion
The finding of a stump appendix is important to note as stump appendicitis (SA) can be a rare long-term complication of appendectomy. It is defined as the interval development of inflammation of the remaining appendix after an appendectomy. The signs and symptoms are the same as an acute appendicitis and can be difficult to diagnose on imaging. Prior knowledge of a stump appendix would thus aid the diagnosis and help clarify the imaging findings which can sometimes be confusing.
Often, there is a delayed or missed diagnosis that can cause morbidity. The perforation rate of SA reportedly ranges from 40 to 70%. SA was first described by Rose in 1945, with a reported incidence of 1 in 50,000 cases. However, the exact prevalence is not known and likely underreported as it may imply inadequate surgical technique. Buttrick et al. conducted a 5-year case review of 3252 appendectomies at our institution, which revealed only two cases of SA yielding a prevalence of approximately 0.06%. In a 60-year review by Subramanian and Liang, patients presented a mean of 108 ± 20 months after initial appendectomy. It was unclear if there werespecific high-risk features for the development of SA.
However, they noted in their review that SA occurred after both open and laparoscopic appendectomies. Additionally, they noted that the mean length of the residual stump was 3.3 cm (range 0.5–6.5 cm) with no patient reported to have SA with residual stump < 0.5 cm. The most common presenting symptom was abdominal pain (93%) with 77% of patients having right lower quadrant pain. Fifty-seven percent of patients presented with gastrointestinal symptoms, including nausea and vomiting.
Often, there is a delayed or missed diagnosis that can cause morbidity. The perforation rate of SA reportedly ranges from 40 to 70%. SA was first described by Rose in 1945, with a reported incidence of 1 in 50,000 cases. However, the exact prevalence is not known and likely underreported as it may imply inadequate surgical technique. Buttrick et al. conducted a 5-year case review of 3252 appendectomies at our institution, which revealed only two cases of SA yielding a prevalence of approximately 0.06%. In a 60-year review by Subramanian and Liang, patients presented a mean of 108 ± 20 months after initial appendectomy. It was unclear if there werespecific high-risk features for the development of SA.
However, they noted in their review that SA occurred after both open and laparoscopic appendectomies. Additionally, they noted that the mean length of the residual stump was 3.3 cm (range 0.5–6.5 cm) with no patient reported to have SA with residual stump < 0.5 cm. The most common presenting symptom was abdominal pain (93%) with 77% of patients having right lower quadrant pain. Fifty-seven percent of patients presented with gastrointestinal symptoms, including nausea and vomiting.
5References
1. Subramanian A, Liang MK. A 60-year literature review of stump appendicitis: The need for a critical view. Am J Surg 2012; 203: 503–7.
2. Martínez Chamorro E, Merina Castilla A, Muñoz Fraile B, Koren Fernández L, Borruel NS. Stump appendicitis: Preoperative imaging findings in four cases. Abdom Imaging 2013; 38: 1214–9.
3. Leff DR, Sait MR, Hanief M, Salakianathan S, Darzi AW, Vashisht R. Inflammation of the residual appendix stump: A systematic review. Colorectal Dis 2012; 14: 282–93.
2. Martínez Chamorro E, Merina Castilla A, Muñoz Fraile B, Koren Fernández L, Borruel NS. Stump appendicitis: Preoperative imaging findings in four cases. Abdom Imaging 2013; 38: 1214–9.
3. Leff DR, Sait MR, Hanief M, Salakianathan S, Darzi AW, Vashisht R. Inflammation of the residual appendix stump: A systematic review. Colorectal Dis 2012; 14: 282–93.