Non-inflamed Stump Appendix within the Cecum [November 2021]
November 1, 2021
Typical ultrasound features in open spina bifida [January 2022]
January 26, 2022Primary liver lymphoma developed in a patient with chronic hepatitis C
AUTHOR
1 Pompilia Radu, 2 Zeno Sparchez
1 University Clinic for Visceral Surgery and Medicine, Inselspital Bern, Switzerland
2 Institute for Gastroenterology and Hepatology, Cluj Napoca, Romania
zsparchez@gmail.com
1 Pompilia Radu, 2 Zeno Sparchez
1 University Clinic for Visceral Surgery and Medicine, Inselspital Bern, Switzerland
2 Institute for Gastroenterology and Hepatology, Cluj Napoca, Romania
zsparchez@gmail.com
1Clinical History
62 years old man with chronic hepatitis C on antiviral treament with Pegylated Interferon and Ribavirin. During the 10th month of the antiviral treatment the patient was complaining of epigastric pain and vomiting. An upper digestive endoscopy was performed which revealed only a mild gastritis.
2Image findings
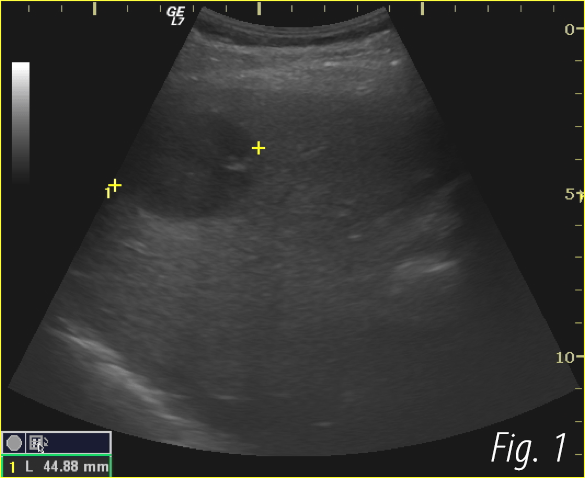
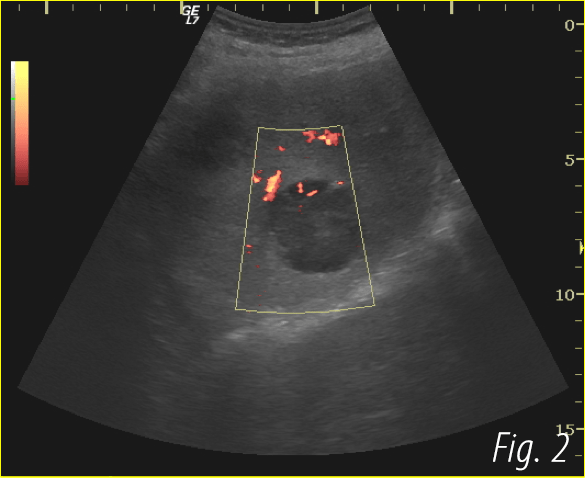
On ultrasound examination 2 hypoechoic tumors (40 and 32 mm in size) were detected in the right liver lobe (Fig.1,2). CEUS showed hypervascularity in arterial phase ( enhancecentripetal web like emhancement) followed by a rapid wash-out in the late arterial phase ( Movie 1-3).
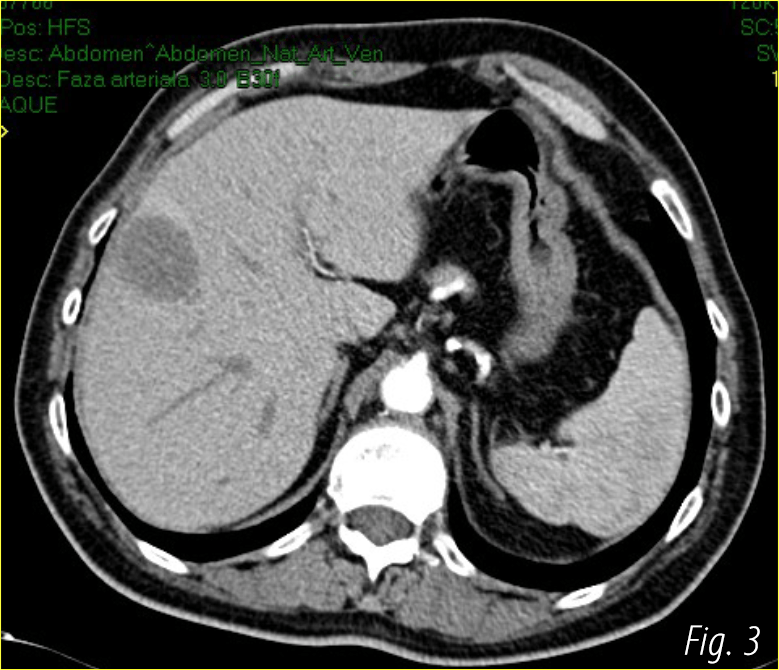
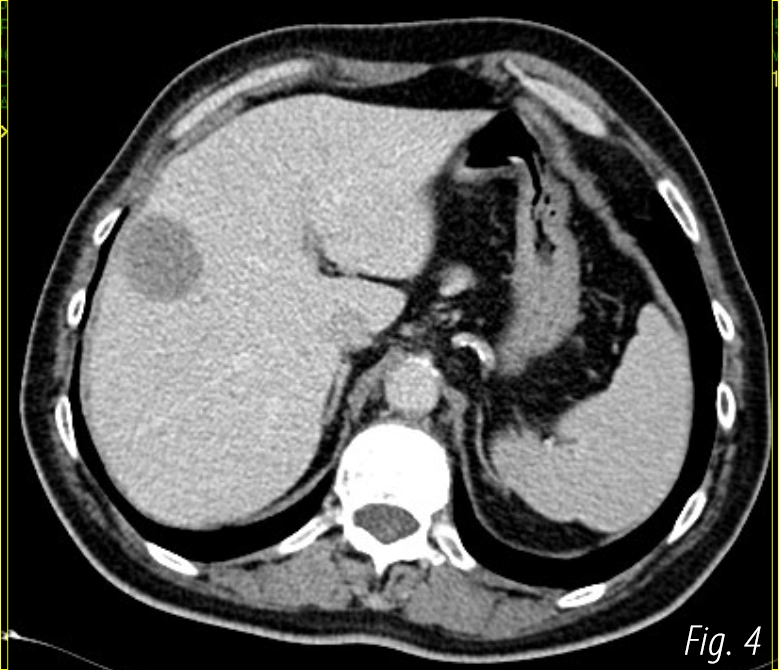
3Computed Tomography
The lesions were hypodense in the pre-contrast phase and with a thick wall enhancement in the arterial phase. Hypervasular hepatic metastases were suspicioned. AFP and other gastrointestinal tumoral markers were normal.
4Diagnosis
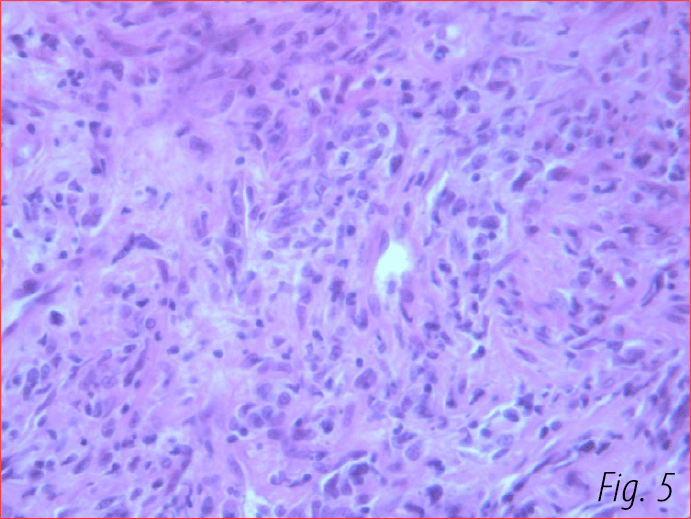
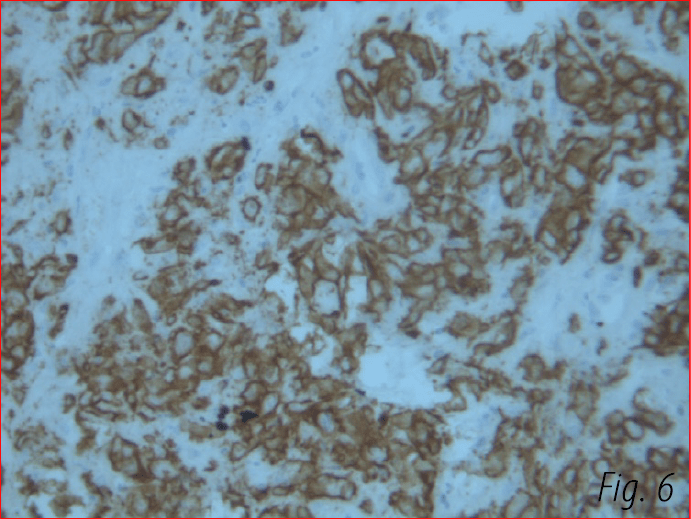
Percutaneous liver biopsy was performed and a proliferation of lymphocites were depicted at histology. The specimen was not sufficient for IHC so another biopsy were performed. The final diagnosis was B cell Nonhodgkin lymphoma ( Fig.5,6). The patient was then sent to the Hematological Clinic for treatment.
5Discussion
Primary liver lymphoma is defined as an extranodal lymphoma of the liver without involvement of any other organ (lymph node, bone marrow, spleen, etc.(1). The primary non-Hodgkin lymphoma of the liver is a rare condition that represents less than 1 % of all extra nodal lymphomas (1,2).<
The exact cause of PHL is unknown, but it seems that there is a strong association between hepatitis C or B virus (HCV) . The majority of PHL patients are middle-aged men who usually present nonspecific symptoms. On imaging the liver involvement may be nodular ( solitary 63% of cases or multiple 37% ) or diffuse (2). In B mode ultrasonography the lesions are almost 100% hypoechoic , some with important color Doppler signals (2,3). Some lesions have ill defined margins and do not invade or deviate hepatic vessels.
CEUS shows various contrast enhancement in arterial phase followed by wash out ( in 100% of cases in all studies). Most of the studies showed hyperenhancement in 100% of cases with except of one showing isoenhancement as the most frequent pattern ( 44%) followed by hypo (31%) and hyperenhancement (25%)(3,4). In our patient the lesions were hyperenhancing in arterial phase (web-like centripetal enhancement) followed by a quick wash- out. On abdominal CT scan the masses are hypo-attenuating. After contrast administration 50% of lesions do not enhance, 33% have a patchy enhancement, and 16% show a peripheral ring of enhancement (1,5) .
Diagnosis of PHL requires a liver biopsy compatible with lymphoma and the absence of lympho-proliferative disease outside the liver. Percutaneous liver biopsy is a reliable and useful tool to diagnose hepatic lymphoma.
The exact cause of PHL is unknown, but it seems that there is a strong association between hepatitis C or B virus (HCV) . The majority of PHL patients are middle-aged men who usually present nonspecific symptoms. On imaging the liver involvement may be nodular ( solitary 63% of cases or multiple 37% ) or diffuse (2). In B mode ultrasonography the lesions are almost 100% hypoechoic , some with important color Doppler signals (2,3). Some lesions have ill defined margins and do not invade or deviate hepatic vessels.
CEUS shows various contrast enhancement in arterial phase followed by wash out ( in 100% of cases in all studies). Most of the studies showed hyperenhancement in 100% of cases with except of one showing isoenhancement as the most frequent pattern ( 44%) followed by hypo (31%) and hyperenhancement (25%)(3,4). In our patient the lesions were hyperenhancing in arterial phase (web-like centripetal enhancement) followed by a quick wash- out. On abdominal CT scan the masses are hypo-attenuating. After contrast administration 50% of lesions do not enhance, 33% have a patchy enhancement, and 16% show a peripheral ring of enhancement (1,5) .
Diagnosis of PHL requires a liver biopsy compatible with lymphoma and the absence of lympho-proliferative disease outside the liver. Percutaneous liver biopsy is a reliable and useful tool to diagnose hepatic lymphoma.
6Teaching Points
PLL should be included in the differential diagnosis of hepatic tumors in patients who are hepatitis C virus-positive, and who have atypical imaging and no known malignancy or elevated tumor marker levels.
The CEUS characteristics may be not different from those of hepatocellular carcinoma but a very quick wash out may raise the suspicion of non HCC malignant lesion and warrant a liver biopsy.
The CEUS characteristics may be not different from those of hepatocellular carcinoma but a very quick wash out may raise the suspicion of non HCC malignant lesion and warrant a liver biopsy.
7References
1. Zentar A, Tarchouli M, Elkaoui H, Belhamidi MS, Ratbi MB, Bouchentouf SM, Ali AA, Bounaim A, Sair K. Primary hepatic lymphoma. J Gastrointest Cancer. 2014;45(3):380-382.
2. Lu Q, Zhang H, Wang WP, Jin YJ, Ji ZB. Primary non-Hodgkin's lymphoma of the liver: sonographic and CT findings. Hepatobiliary Pancreat Dis Int. 2015 ;14(1):75-81.
3. Foschi FG, Dall'Aglio AC, Marano G, et al. Role of contrast-enhanced ultrasonography in primary hepatic lymphoma. J Ultrasound Med. 2010;29(9):1353-6.
4. Trenker C, Kunsch S, Michl P, Wissniowski TT, Goerg K, Goerg C. Contrast-enhanced ultrasound (CEUS) in hepatic lymphoma: retrospective evaluation in 38 cases. Ultraschall Med. 2014 Apr;35(2):142-8.
5. Ippolito D, Porta M, Maino C, et al. Diagnostic approach in hepatic lymphoma: radiological imaging findings and literature review. J Cancer Res Clin Oncol. 2020;146(6):1545-1558
2. Lu Q, Zhang H, Wang WP, Jin YJ, Ji ZB. Primary non-Hodgkin's lymphoma of the liver: sonographic and CT findings. Hepatobiliary Pancreat Dis Int. 2015 ;14(1):75-81.
3. Foschi FG, Dall'Aglio AC, Marano G, et al. Role of contrast-enhanced ultrasonography in primary hepatic lymphoma. J Ultrasound Med. 2010;29(9):1353-6.
4. Trenker C, Kunsch S, Michl P, Wissniowski TT, Goerg K, Goerg C. Contrast-enhanced ultrasound (CEUS) in hepatic lymphoma: retrospective evaluation in 38 cases. Ultraschall Med. 2014 Apr;35(2):142-8.
5. Ippolito D, Porta M, Maino C, et al. Diagnostic approach in hepatic lymphoma: radiological imaging findings and literature review. J Cancer Res Clin Oncol. 2020;146(6):1545-1558