- European Federation of Societies for Ultrasound in Medicine and Biology ~ Educating all for competence to practice ultrasound safely

Abdominal (retroperitoneal) lymphadenopathy [Oct 2016]
October 11, 2016
Supersonic Shear Imaging ShearWave Elastography [Dec 2016]
December 11, 2016One-stop differential diagnosis of Mllerian anomalies using 3D ultrasound: complete uterine septum
Assistant Professor of Obstetrics and Gynecology
Aristotle University of Thessaloniki, Greece
The human fallopian tubes, uterus, cervix and the upper two thirds of the vagina develop from the two Müllerian (paramesonephric) ducts through a three-stage process, i.e. organogenesis, fusion and septal resorption (1). The lateral fusion of the Müllerian ducts occurs between the seventh and ninth weeks, when their lower segments fuse. At this stage a midline septum is present in the uterine cavity, which usually regresses at around 20 weeks (2).
Failure of the Müllerian ducts to fuse results in a bicornuate or didelphys uterus, whereas failure of the septum to resorb results in arcuate or septate uterus (complete or partial). When two cervical orifices are identified at speculum examination, differential diagnosis must be made between didelphys and completely septate uterus, as the two conditions differ in their embryological origin, clinical associations and surgical repair.
Hysterosalpingography has traditionally been the mainstay in the diagnostic workup of Müllerian abnormalities of the uterus, but it cannot depict the external contour of the uterus. The development of three-dimensional (3D) ultrasound has been recently proven a cost-effective means for the diagnosis and differential diagnosis of Müllerian duct abnormalities, having equal or better performance than MRI (1).
In this case, a young (21-year old) G0P0 woman visited her Obstetrician for her first check-up after the commencement of intercourse. On speculum examination, two separate cervical ossa were seen; 2D ultrasound demonstrated two separate endometrial echogenicities, indicating the presence of two endometrial cavities. The patient was referred for 3D transvaginal scan (TVS) with the tentative diagnosis of didelphys uterus.
The patient was scanned on a GE E6 Voluson Expert machine (GE Healthcare, Milwaukee, WI), using a RIC5-9-D vaginal 4D probe. The uterus was originally scanned in a longitudinal plane and a 3D volume was taken. The reconstruction of the uterus on the coronal plane was done using the OmniView / Polyline modality and render modality with GYNSurfaceHD surface setting.
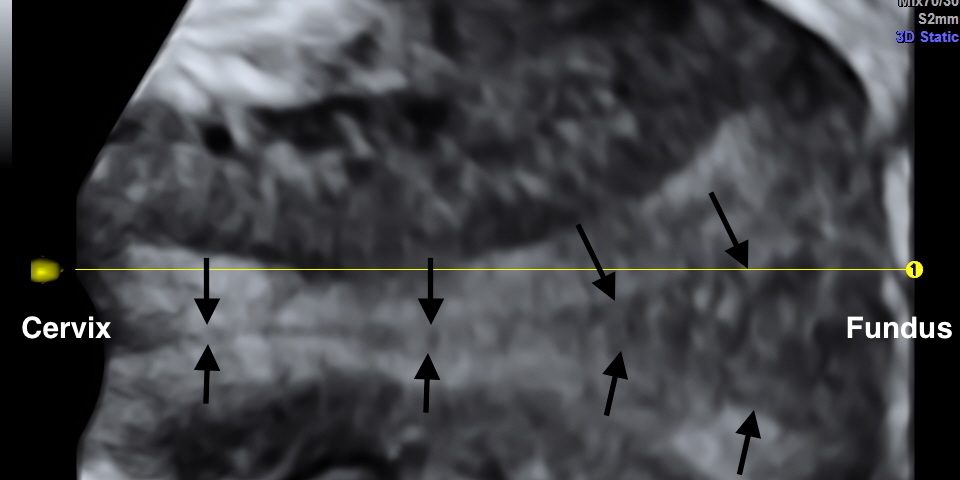
Three-dimensional reconstruction showed a midline septum running throughout the uterine cavity and the cervix, with normal contour of the uterine fundus. Therefore the diagnosis of a complete uterine septum as per the American Fertility Society, or a Class U2bC1 anomaly (complete uterine septum with septate cervix) as per the European Society of Human Reproduction and Embryology / European Society of Gynecologic Endoscopy (ESHRE/ESGE) new guidelines (3) was made (Figures 1 and 2).
The prevalence of Müllerian abnormalities is approximately 5.5% in the general population, increases to 8.8% among women with infertility and reaches a staggering 24.5% in women with recurrent miscarriages and infertility (4). Among these conditions, canalization abnormalities, i.e. subseptate or septate uterus, are found in 2.3% of the general population, in 5.3% of women with recurrent miscarriage and in 15.4% of those with recurrent miscarriage and infertility (4). Septate uterus has been associated with increased risk for infertility, first-trimester miscarriage (relative risk 2.89) and preterm birth (relative risk 2.14) (5). Recently a series of 24 pregnant women was reported, in whom a septate uterus was incidentally diagnosed at early pregnancy scan; only 33.3% progressed beyond the second trimester (6). Complete uterine septum with cervical duplication is an uncommon variant of septate uterus, however there are currently more than 40 cases published in the literature (7-9).
Traditionally, a history of reproductive complications was the trigger for investigating the patient using transvaginal sonography, hysterosalpingography and, commonly, laparoscopy. With the advent of MRI, it became the imaging method of choice, due to its lack of radiation and its ability to clearly delineate both the internal and external uterine anatomy (1). Recently, 3D transvaginal ultrasound has emerged as a comparably reliable, easier and cheaper alternative to MRI. 3D ultrasound creates a “volume” of image data, in which the operator can navigate either at the time of examination or later in a stored volume (offline).
The optimal method for diagnosing Mullerian anomalies was the subject of a recent ESHRE consensus committee, which examined the advantages and disadvantages of each of the methods used. Gynecological examination and standard 2-dimensional ultrasound was deemed as the method of choice in asymptomatic women, based on its wide availability and minimal cost. Whenever a woman is at high risk, or a suspicion ensues, 3-D ultrasound (transvaginal or transabdominal or transperineal, according to the circumstances) is the preferred means for the extended investigation, complemented by other methods (e.g. MRI and/or hysteroscopy and/or laparoscopy) if necessary (10).
In the case of complete septate uterus, 3D reconstruction of the endometrial cavity and the fundal contour in a coronal plane allowed the differentiation from uterus didelphys, which is the most common differential diagnosis when a double cervical os is encountered at speculum examination.
The most common presenting complaint in cases of septate uterus is pregnancy loss in parous women and dyspareunia in nulligravid patients (11). Although hysteroscopic resection of the septum is the therapeutic mainstay for these cases, its effectiveness has never been tested in randomized controlled trials (12). However, retrospective data indicate that the pregnancy outcome in these patients is significantly improved after surgery (13), and septectomy is an intuitive symptomatic treatment for dyspareunia in women with a vaginal septum.
In conclusion, this case of an uncommon anomaly illustrates how the recent addition of 3D ultrasound in the diagnostic toolbox can facilitate fast, safe, reliable and low-cost differentiation of a Müllerian anomaly at an outpatient setting, which would otherwise require hysteroscopy and/or hysterosalpingography plus laparoscopy, or, at best MRI, in a separate appointment.
- Chandler TM, Machan LS, Cooperberg PL, Harris AC, Chang SD. Mullerian duct anomalies: from diagnosis to intervention. Br J Radiol. 2009 Dec;82(984):1034-42.
- Healey A. Embryology of the female reproductive tract. In: Mann GS, Blair JC, Garden AS (Eds.) Imaging of Gynecological Disorders in Infants and Children. Springer, 2012:21-30
- Grimbizis GF, Gordts S, Di Spiezio Sardo A, Brucker S, De Angelis C, Gergolet M, Li TC, Tanos V, Brölmann H, Gianaroli L, Campo R. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum Reprod. 2013 Aug;28(8):2032-44
- Chan YY, Jayaprakasan K, Zamora J, Thornton JG, Raine-Fenning N, Coomarasamy A. The prevalence of congenital uterine anomalies in unselected and high-risk populations: a systematic review. Hum Reprod Update. 2011 Nov-Dec;17(6):761-71
- Chan YY, Jayaprakasan K, Tan A, Thornton JG, Coomarasamy A, Raine-Fenning NJ. Reproductive outcomes in women with congenital uterine anomalies: a systematic review. Ultrasound Obstet Gynecol. 2011 Oct;38(4):371-82.
- Ghi T, De Musso F, Maroni E, Youssef A, Savelli L, Farina A, Casadio P, Filicori M, Pilu G, Rizzo N. The pregnancy outcome in women with incidental diagnosis of septate uterus at first trimester scan. Hum Reprod. 2012 Sep;27(9):2671-5
- Saygili-Yilmaz ES, Erman-Akar M, Bayar D, Yuksel B, Yilmaz Z. Septate uterus with a double cervix and longitudinal vaginal septum. J Reprod Med. 2004 Oct;49(10):833-6.
- Ribeiro SC, Yamakami LY, Tormena RA, Pinheiro Wda S, Almeida JA, Baracat EC. Septate uterus with cervical duplication and longitudinal vaginal septum. Rev Assoc Med Bras. 2010 Mar-Apr;56(2):254-6.
- Chen SQ, Deng N, Jiang HY, Li JB, Lu S, Yao SZ. Management and reproductive outcome of complete septate uterus with duplicated cervix and vaginal septum: review of 21 cases. Arch Gynecol Obstet. 2013 Apr;287(4):709-14.
- Grimbizis GF, Di Spiezio Sardo A, Saravelos SH, Gordts S, Exacoustos C, Van Schoubroeck D, Bermejo C, Amso NN, Nargund G, Timmerman D, Athanasiadis A, Brucker S, De Angelis C, Gergolet M, Li TC, Tanos V, Tarlatzis B, Farquharson R, Gianaroli L, Campo R. The Thessaloniki ESHRE/ESGE consensus on diagnosis of female genital anomalies†. Hum Reprod. 2016;31(1):2-7
- Patton PE, Novy MJ, Lee DM, Hickok LR. The diagnosis and reproductive outcome after surgical treatment of the complete septate uterus, duplicated cervix and vaginal septum. Am J Obstet Gynecol. 2004 Jun;190(6):1669-75
- Kowalik CR, Goddijn M, Emanuel MH, Bongers MY, Spinder T, de Kruif JH, Mol BW, Heineman MJ. Metroplasty versus expectant management for women with recurrent miscarriage and a septate uterus. Cochrane Database Syst Rev. 2011 Jun 15;(6):CD008576
- Homer HA, Li TC, Cooke ID. The septate uterus: a review of management and reproductive outcome. Fertil Steril. 2000 Jan;73(1):1-14
Figure 2: Reconstruction as before using the render modality with GYNSurfaceHD surface setting.


![One-stop differential diagnosis of Mllerian anomalies using 3D ultrasound: complete uterine septum</br> [Nov 2016]](https://efsumb.org/wp-content/uploads/2020/11/cotm_november2016-fig01.jpg)
![One-stop differential diagnosis of Mllerian anomalies using 3D ultrasound: complete uterine septum</br> [Nov 2016]](https://efsumb.org/wp-content/uploads/2020/11/cotm_november2016-fig02.jpg)
