MALT Lymphoma developed on a Sjogren Syndrome [Aug 2022]
October 31, 2022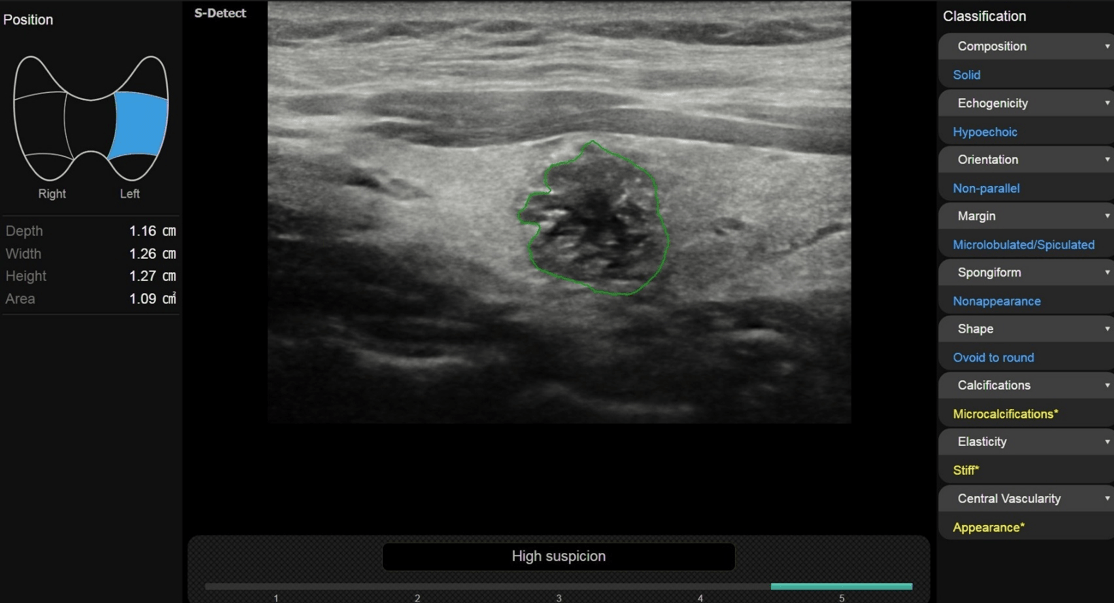
Multiparametric ultrasound and AI of Papillary Carcinoma [Oct 2022]
December 30, 2022Pilomatricoma: A Case Report with Pathological Confirmation
AUTHORS
Hakan Doğan[1],
Evren Uzer[1],
Gizem Timocin Yıgman[1],
Adnan Kabaalioglu[1] [1] Department of Radiology, Koç University Hospital, Istanbul, Turkey
*Corresponding author:
Hakan Doğan
Koç University School of Medicine, Department of Radiology, 34010, Istanbul, Turkey
Tel: +90 212 250 82 50, Fax: +90 850 250 82 50
E-mail: hakandoganmd@gmail.com
Hakan Doğan[1],
Evren Uzer[1],
Gizem Timocin Yıgman[1],
Adnan Kabaalioglu[1] [1] Department of Radiology, Koç University Hospital, Istanbul, Turkey
*Corresponding author:
Hakan Doğan
Koç University School of Medicine, Department of Radiology, 34010, Istanbul, Turkey
Tel: +90 212 250 82 50, Fax: +90 850 250 82 50
E-mail: hakandoganmd@gmail.com
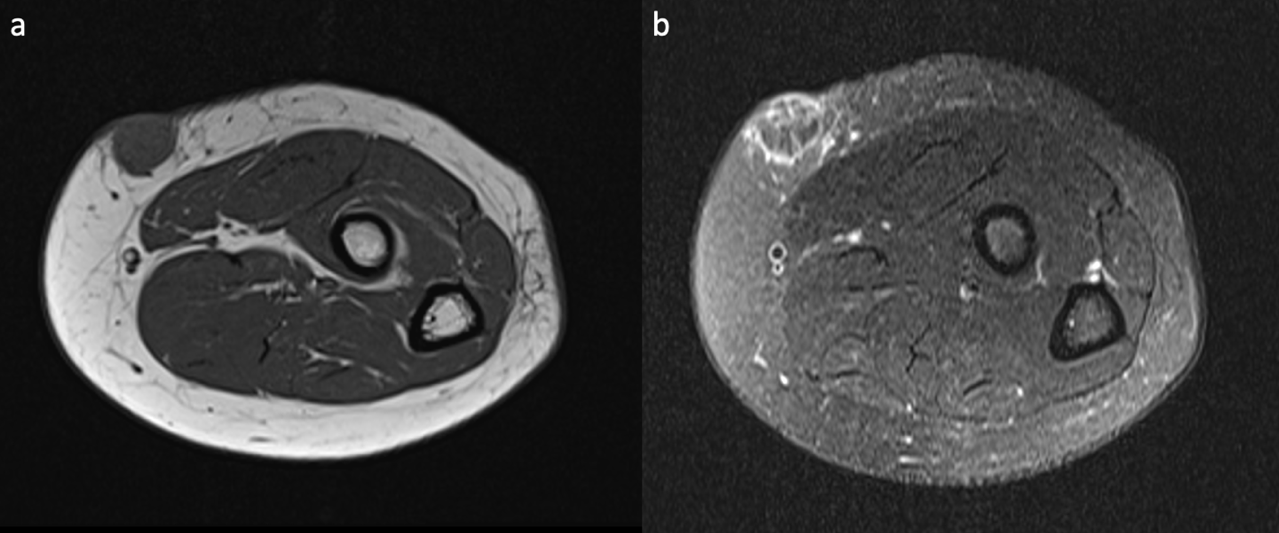
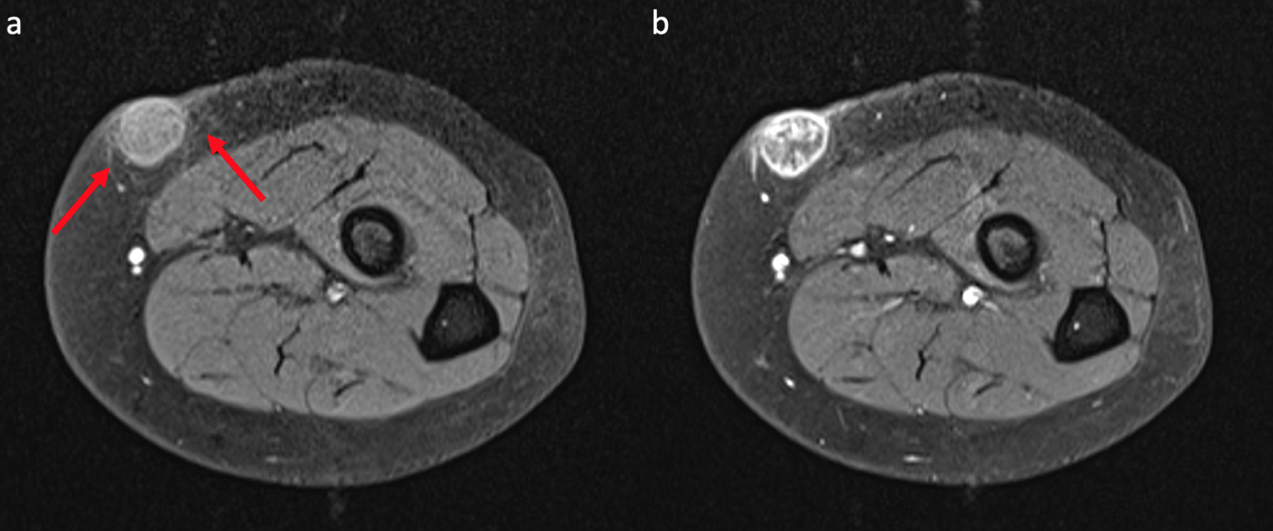
Figure 4. Pre- and post-contrast fat-saturated T1-weighted images of the lesion. After intravenous contrast administration, the lesion depicts internal reticular and peripheral ring-like enhancement (b). Perilesional fat stranding (red arrows) is also seen on pre-contrast fat-saturated T1-weighted image (a).
1Clinical History
A 23-year-old female patient was admitted to our orthopedics and traumatology clinic with a six month history of slowly enlarging mass in the left forearm. She denied any previous trauma to the area.
Physical examination showed a firm, mobile, superficial, nodular mass with mild tenderness and erythema in the extensor surface of the proximal left forearm.
Physical examination showed a firm, mobile, superficial, nodular mass with mild tenderness and erythema in the extensor surface of the proximal left forearm.
2Image findings
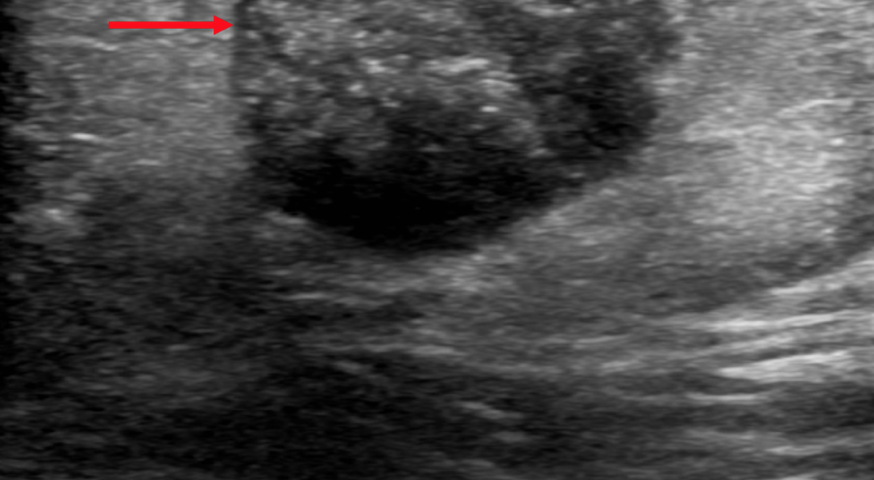
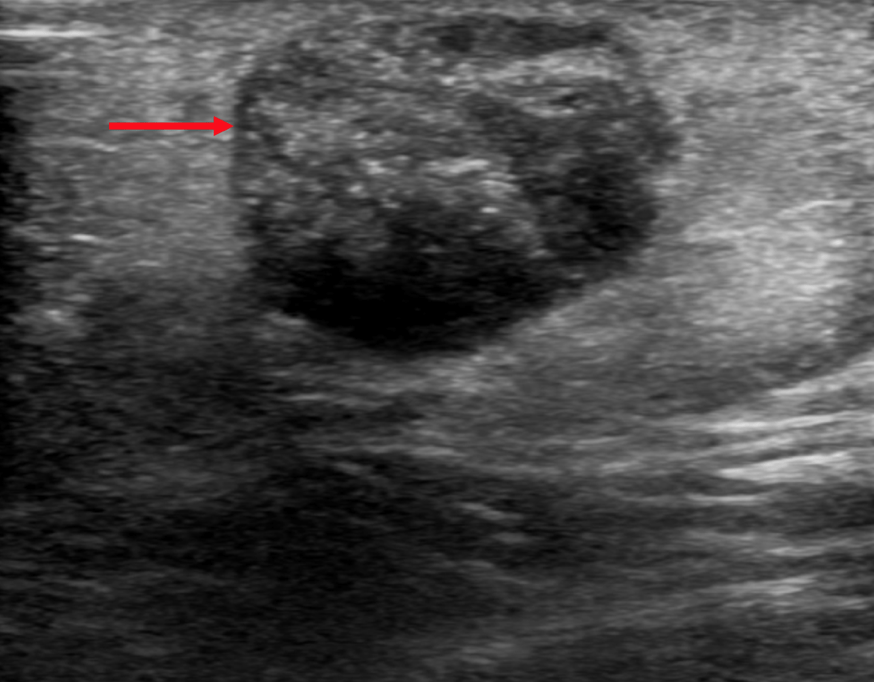
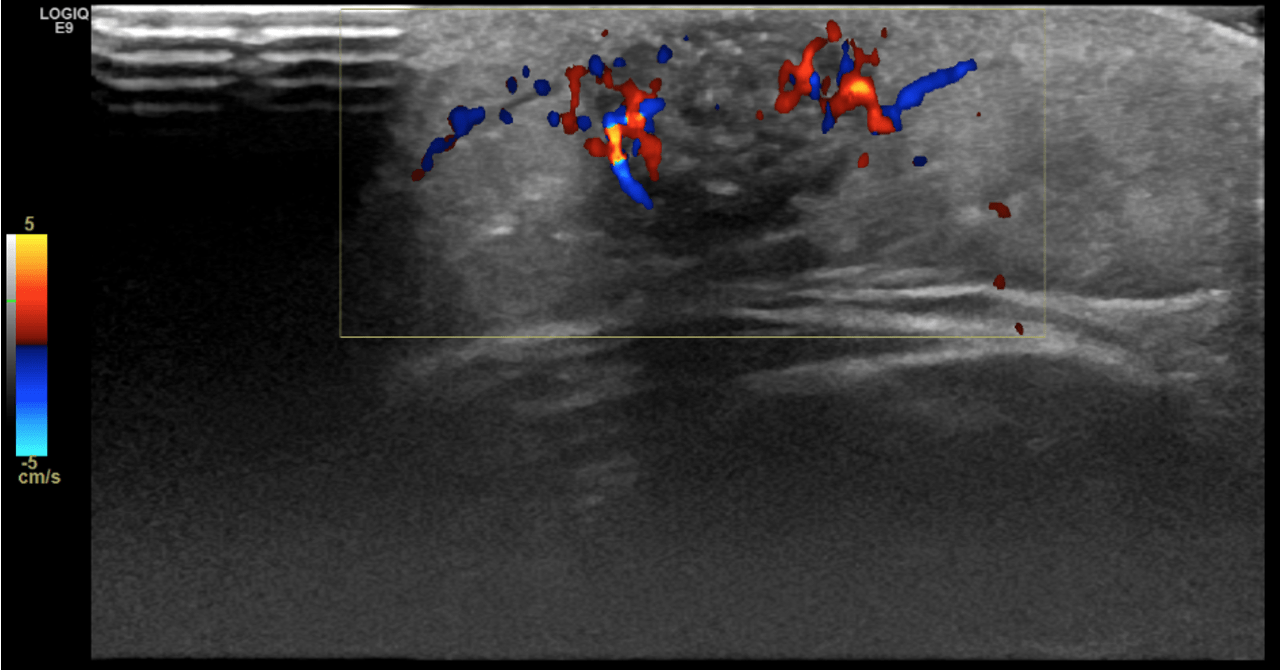
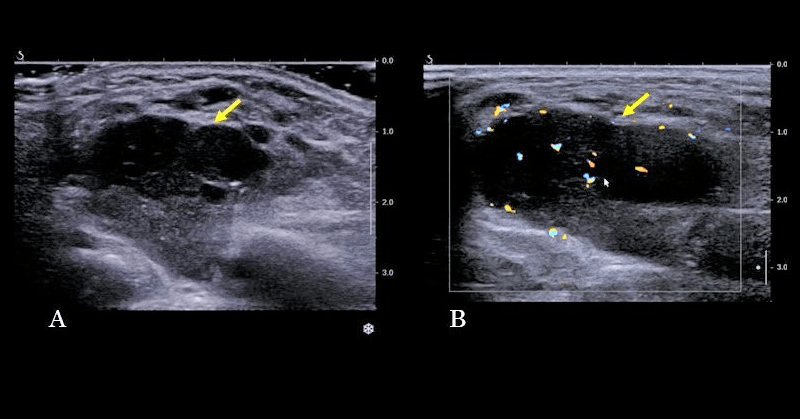
Gray scale ultrasound (US) examination revealed a 14x10 mm, subcutaneous, well-defined, oval-shaped mass. The lesion was heterogeneously hypoechoic with peripheral hypoechoic rim and internal, scattered hyperechoic foci with mild acoustic shadowing. Perilesional hyperechogenicity was also noted (Figure 1). On color Doppler US, the lesion had internal and peripheral vascularity (Figure 2).
On magnetic resonance imaging (MRI), the lesion was homogenously hypointense on T1-weighted images (T1-WI) and heterogeneous with internal and ring-like hyperintensities on fat-suppressed T2-weighted images (T2WI). After intravenous contrast administration, peripheral ring-like and internal reticular enhancement was observed. Perilesional fat stranding was also seen.
On magnetic resonance imaging (MRI), the lesion was homogenously hypointense on T1-weighted images (T1-WI) and heterogeneous with internal and ring-like hyperintensities on fat-suppressed T2-weighted images (T2WI). After intravenous contrast administration, peripheral ring-like and internal reticular enhancement was observed. Perilesional fat stranding was also seen.
3Diagnosis
Excisional biopsy was performed and the histopathological examination was consistent with pilomatricoma.
4Discussion
BACKGROUND
Pilomatricoma is a deep dermal or subcutaneous tumor originating from the hair cortex cells. It was first described by Malharbe and Chenantais in 1880, and was formerly known as “calcifying epithelioma of Malherbe”. Pilomatricomas constitute 0.12% of all skin tumors and are usually benign. Malignant transformation is possible, although very rare (1).
Pilomatricomas are usually located in the head and neck region but they can also be found in the trunk and the upper and lower extremities. They are usually solitary, but in patients with some autosomal dominant diseases or syndromes, such as myotonic muscular dystrophy and Gardner syndrome, multiple pilomatricomas can be seen (1).
Pilomatricomas often develop in the first two decades of life and mostly affect children and adolescents. There is also a slight female predominance (1).
CLINICAL PERSPECTIVE
Pilomatricomas usually manifest as firm, slow-growing, superficial masses with reddish-blue discoloration. They can range in size from 0.5 to 3 cm in diameter (1).
THERAPY PLANNING:
Pilomatricomas do not regress spontaneously and surgical excision is the preferred treatment choice (2).
OUTCOME & PROGNOSIS:
Pilomatricomas have excellent prognosis after complete surgical resection. Recurrences can occur in case of incomplete excision (3).
Pilomatricoma is a deep dermal or subcutaneous tumor originating from the hair cortex cells. It was first described by Malharbe and Chenantais in 1880, and was formerly known as “calcifying epithelioma of Malherbe”. Pilomatricomas constitute 0.12% of all skin tumors and are usually benign. Malignant transformation is possible, although very rare (1).
Pilomatricomas are usually located in the head and neck region but they can also be found in the trunk and the upper and lower extremities. They are usually solitary, but in patients with some autosomal dominant diseases or syndromes, such as myotonic muscular dystrophy and Gardner syndrome, multiple pilomatricomas can be seen (1).
Pilomatricomas often develop in the first two decades of life and mostly affect children and adolescents. There is also a slight female predominance (1).
CLINICAL PERSPECTIVE
Pilomatricomas usually manifest as firm, slow-growing, superficial masses with reddish-blue discoloration. They can range in size from 0.5 to 3 cm in diameter (1).
THERAPY PLANNING:
Pilomatricomas do not regress spontaneously and surgical excision is the preferred treatment choice (2).
OUTCOME & PROGNOSIS:
Pilomatricomas have excellent prognosis after complete surgical resection. Recurrences can occur in case of incomplete excision (3).
5Teaching Points
On ultrasound, if a heterogeneous, well-defined, oval-shaped mass with a peripheral hypoechoic rim, perilesional hyperechogenicity, vascularity, and internal hyperechoic foci which show acoustic shadowing is found in the subcutaneous layer, a diagnosis of pilomatricoma should be taken into consideration.
6Conflicts of Interest
The authors have no competing interests to declare that are relevant to the content of this case report.
7References
1. Kato H, Kanematsu M, Watanabe H, et al. MR imaging findings of pilomatricomas: a radiological-pathological correlation. Acta Radiol. 2016;57(6):726-732.
2. Choo HJ, Lee SJ, Lee YH, et al. Pilomatricomas: the diagnostic value of ultrasound. Skeletal Radiol. 2010;39(3):243-250.
3. Hwang JY, Lee SW, Lee SM. The common ultrasonographic features of pilomatricoma. J Ultrasound Med. 2005;24(10):1397-1402.
2. Choo HJ, Lee SJ, Lee YH, et al. Pilomatricomas: the diagnostic value of ultrasound. Skeletal Radiol. 2010;39(3):243-250.
3. Hwang JY, Lee SW, Lee SM. The common ultrasonographic features of pilomatricoma. J Ultrasound Med. 2005;24(10):1397-1402.