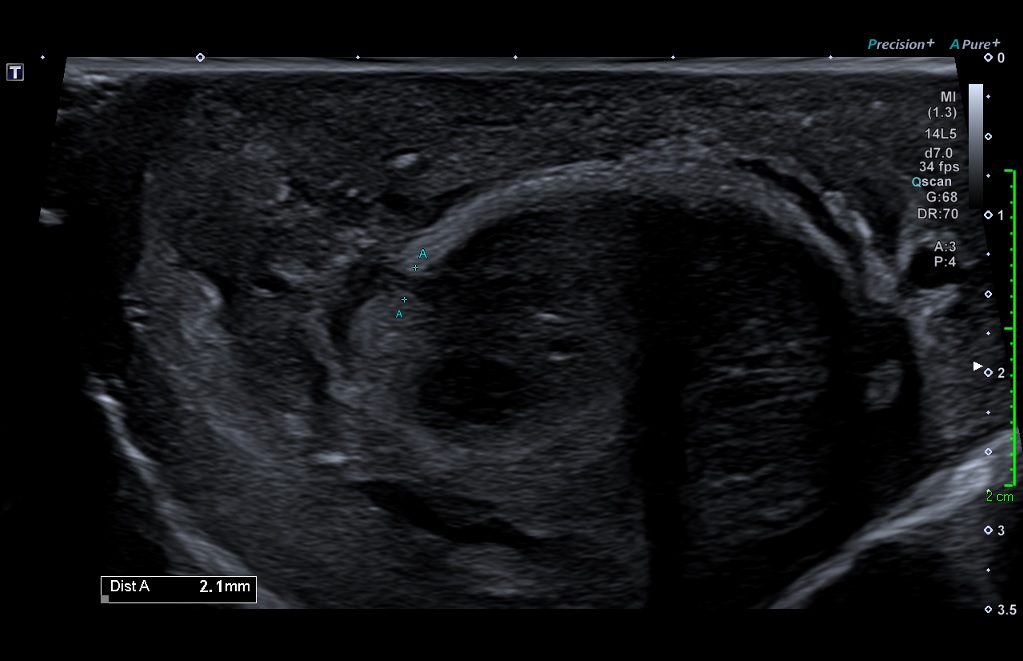
An unusual penile swelling [July 2021]
June 30, 2021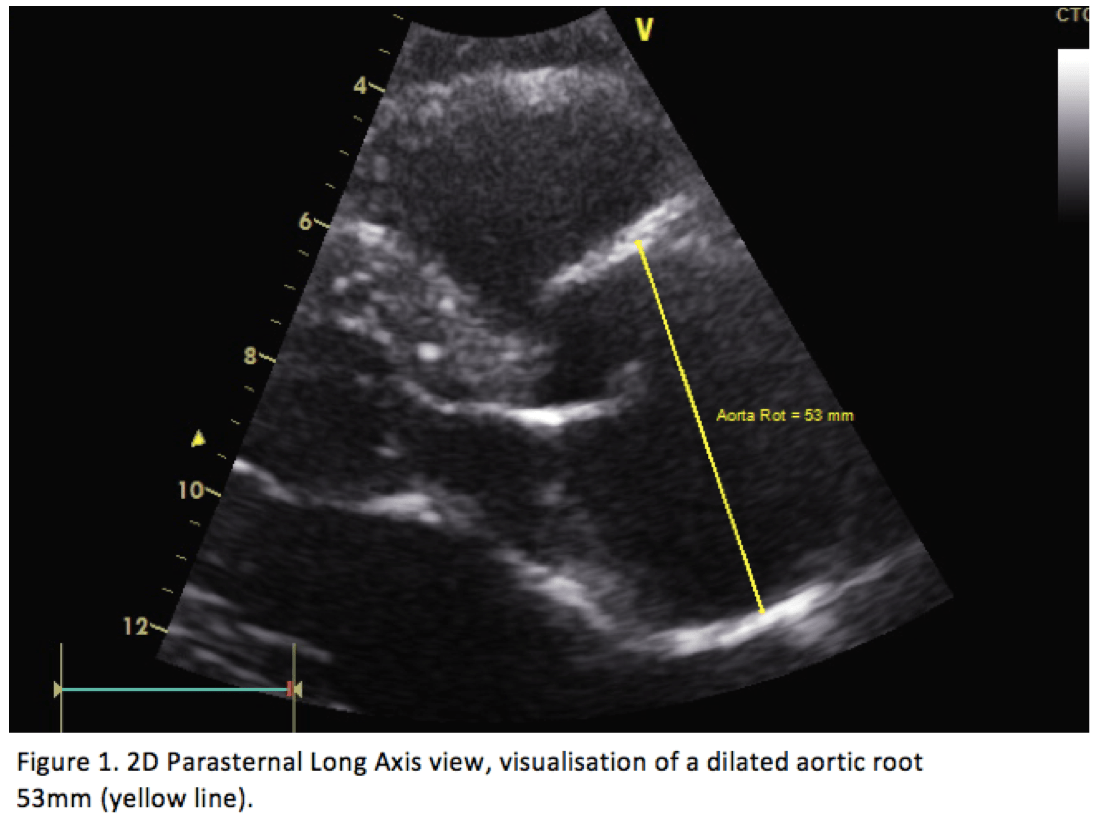
Diagnosing Thoracic Aortic Dissection using Bedside Ultrasound in an Emergency Department in a Norwegian University Teaching Hospital [September 2021]
September 6, 2021Ultrasound findings in Sars-Cov2-Infection of the lung
AUTHORS
Jonas B H Koch (1)
Christoph F Dietrich (2)
(1) Kliniken Hirslanden Beau Site, Salem und Permanence, Bern, Switzerland, jonas.koch@hirslanden.ch (2) Kliniken Hirslanden Beau Site, Salem und Permanence, Bern, Switzerland, ChristophFrank.Dietrich@hirslanden.ch
Jonas B H Koch (1)
Christoph F Dietrich (2)
(1) Kliniken Hirslanden Beau Site, Salem und Permanence, Bern, Switzerland, jonas.koch@hirslanden.ch (2) Kliniken Hirslanden Beau Site, Salem und Permanence, Bern, Switzerland, ChristophFrank.Dietrich@hirslanden.ch
Correspondence:
Prof. Dr. med. Christoph F. Dietrich
Department of General Internal Medicine DAIM, Kliniken Hirslanden Beau Site, Salem und Permanence, Bern, Switzerland
ChristophFrank.Dietrich@hirslanden.ch
Tel +41764408150
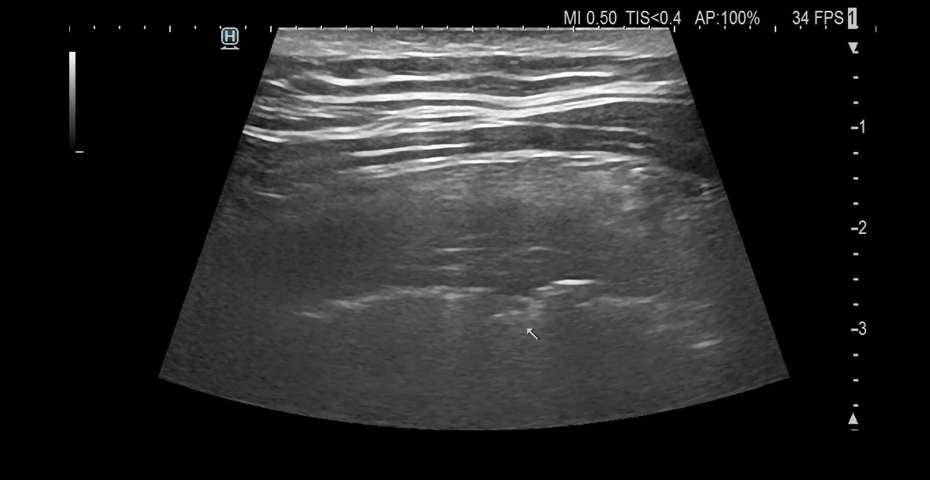
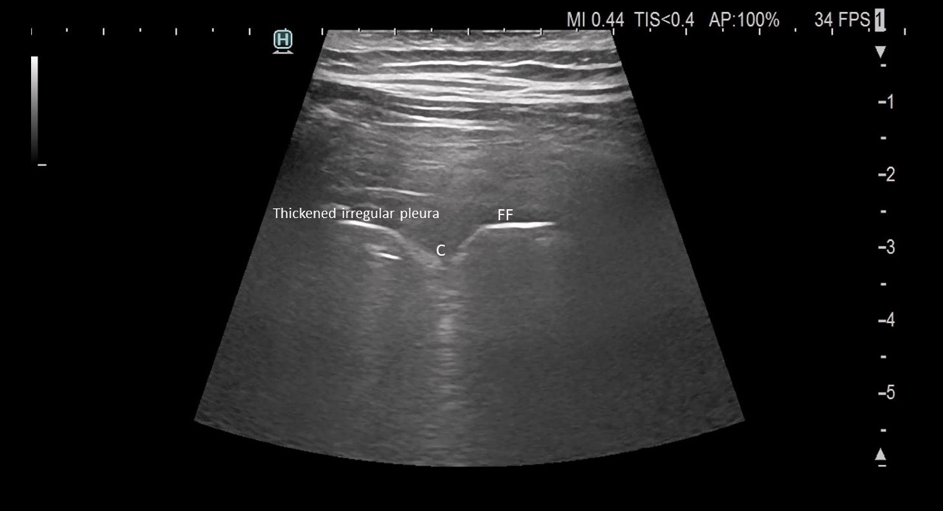
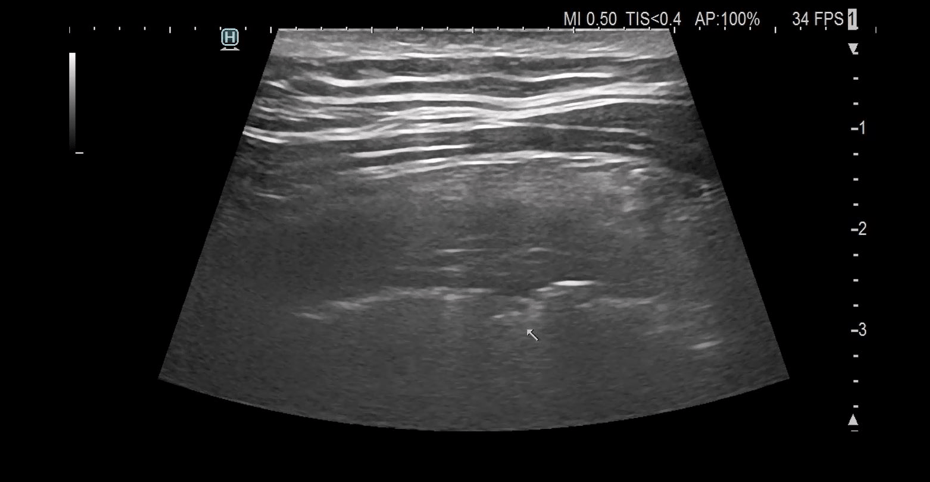
Video: Multiple consolidations in the right lung are shown in video 1 (same region as shown in figures a-d).
1Clinical history
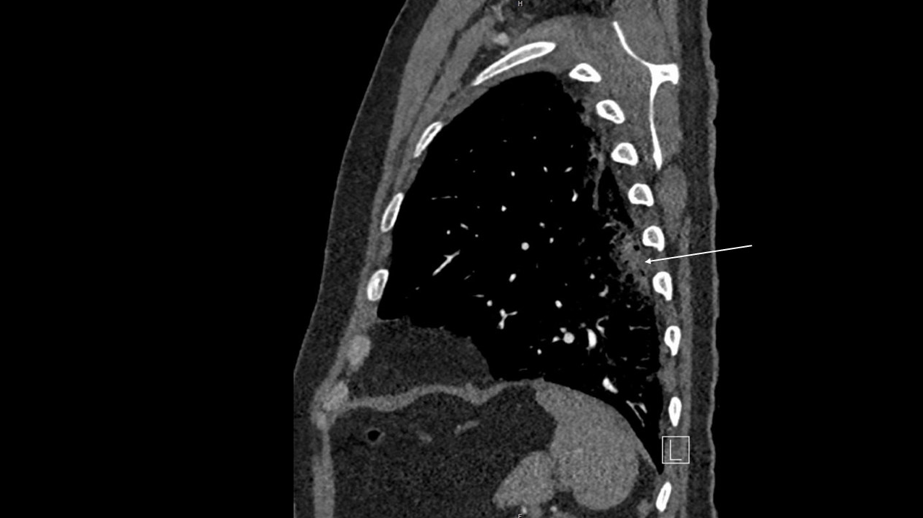
60 year old male tested positive for Sars-CoV2- after having symptoms of upper airway infection for two days. On the day he became increasingly dyspneic and tachypneic with increased thoracic pressure, he was hospitalized. Owing to the rapid increasing oxygen requirements, he was intubated and admitted to the ICU for 9 days. On the first day back on the ward, he was asymptomatic and only needed 3l oxygen. Ultrasound imaging was performed at this time point.
2Discussion
COVID-19 infection is primarily a respiratory disease, therefore, lung imaging is essential for diagnosis (1,2). The typical sonographic signs using lung US (LUS) identified in the course of COVID-19 infections include features of the pleura and pleural space (1), findings of interstitial pneumonia (2) and artefacts (3) (1,3-5). The signs are specific when there is a very high “pretest” probability of patients with cough and dyspnea (1). There is often initial posterior-basal lung involvement, which may become extensive and involve the entire lung. In the later stages, mixed and much less specific image patterns can be observed including bacterial pneumonia superinfection and the so-called white lung. US also allows detection of complications including pneumothorax and pulmonary embolism (5).
3Ultrasound signs and differential diagnosis
Pleura
• Thickened, irregular (coarse) and fragmented pleural line.
• Small(est) superficially located pleural fluid (sign of severity). More extensive pleural effusion is not typical.
Lung
• Consolidation, multiple areas. Initially, often posterobasal with very small consolidative foci developing later, in various distribution and may involve the entire lung.
• Aero-alveolo-broncho-gram as typical sign of pneumonia beyond interstitial pneumonia.
Artefacts
• B-line artefacts (BLA, initially discrete, later multifocal and confluent).
• Respiratory dependent lung sliding in combination with A-line artefacts, combined with BLA (heterogeneous involvement of the lungs with mixing A and B patterns nearby, in a different manner from cardiac pulmonary edema, which shows homogeneous increase in B lines).
Differential diagnosis and complications
• Chronic heart insufficiency (BLA, larger pleura effusion than in CoViD).
• Bacterial pneumonia (typically larger consolidations than in CoViD).
• Lunge emboli.
• Pneumothorax.
• Thickened, irregular (coarse) and fragmented pleural line.
• Small(est) superficially located pleural fluid (sign of severity). More extensive pleural effusion is not typical.
Lung
• Consolidation, multiple areas. Initially, often posterobasal with very small consolidative foci developing later, in various distribution and may involve the entire lung.
• Aero-alveolo-broncho-gram as typical sign of pneumonia beyond interstitial pneumonia.
Artefacts
• B-line artefacts (BLA, initially discrete, later multifocal and confluent).
• Respiratory dependent lung sliding in combination with A-line artefacts, combined with BLA (heterogeneous involvement of the lungs with mixing A and B patterns nearby, in a different manner from cardiac pulmonary edema, which shows homogeneous increase in B lines).
Differential diagnosis and complications
• Chronic heart insufficiency (BLA, larger pleura effusion than in CoViD).
• Bacterial pneumonia (typically larger consolidations than in CoViD).
• Lunge emboli.
• Pneumothorax.
4Conflicts of Interest:
“The authors declare no conflict of interest.”
5References
1. Piscaglia F, Stefanini F, Cantisani V, Sidhu PS, Barr R, Berzigotti A, Chammas MC, et al. Benefits, Open questions and Challenges of the use of Ultrasound in the COVID-19 pandemic era. The views of a panel of worldwide international experts. Ultraschall Med 2020;41:228-236.
2. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med 2020;382:727-733.
3. Dietrich CF, Mathis G, Cui XW, Ignee A, Hocke M, Hirche TO. Ultrasound of the pleurae and lungs. Ultrasound Med Biol 2015;41:351-365.
4. Dietrich CF, Mathis G, Blaivas M, Volpicelli G, Seibel A, Atkinson NS, Cui XW, et al. Lung artefacts and their use. Med Ultrason 2016;18:488-499.
5. Dietrich CF, Mathis G, Blaivas M, Volpicelli G, Seibel A, Wastl D, Atkinson NS, et al. Lung B-line artefacts and their use. J Thorac Dis 2016;8:1356-1365.
2. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med 2020;382:727-733.
3. Dietrich CF, Mathis G, Cui XW, Ignee A, Hocke M, Hirche TO. Ultrasound of the pleurae and lungs. Ultrasound Med Biol 2015;41:351-365.
4. Dietrich CF, Mathis G, Blaivas M, Volpicelli G, Seibel A, Atkinson NS, Cui XW, et al. Lung artefacts and their use. Med Ultrason 2016;18:488-499.
5. Dietrich CF, Mathis G, Blaivas M, Volpicelli G, Seibel A, Wastl D, Atkinson NS, et al. Lung B-line artefacts and their use. J Thorac Dis 2016;8:1356-1365.