- European Federation of Societies for Ultrasound in Medicine and Biology ~ Educating all for competence to practice ultrasound safely

Ultrasound diagnosis of bladder endometriosis [Dec 2022]
February 20, 2023
Subclavian Steal Syndrome [Feb 2023]
May 25, 2023SUBMIT YOUR CASE
EFSUMB invites submission of interesting cases for the website section 'Case of the Month'. All CoM submissions are eligible for selection for free registration at the next Euroson congress. Two cases that receive the most 'likes' in a year will receive free registration for the next EUROSON congress and the third most liked liked case will receive a cash prize of 100 EUR.
2022 Winners were:
Top rated is Sonographic Diagnosis of a Pott’s Puffy Tumor in a 5-year-old-girl - [Jul 2022]
M Brandt Department of Otorhinolaryngology, Head and Neck Surgery, University Hospital of Regensburg, Germany
Second is Ischemic Colitis as Complication of SARS-CoV-2 Infection - [June 2022]
Federica Lepore Department of Internal Medicine, San Matteo Hospital Foundation, University of Pavia, Italy
Both winners received free registration at EUROSON2023.
View Submission Template
An Eye for an Eye
Dr Jędrzej Krawczyk, Ms Theresa Richardson, Professor Adrian Lim
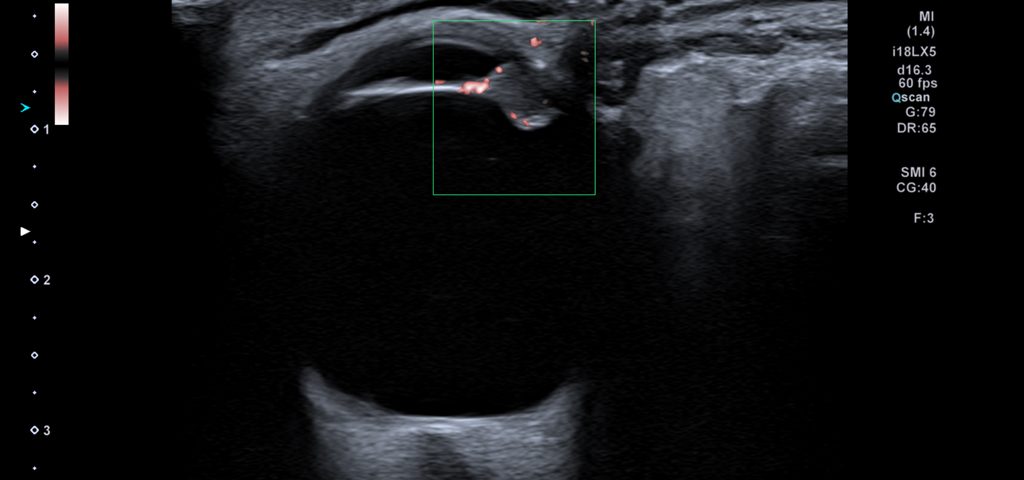
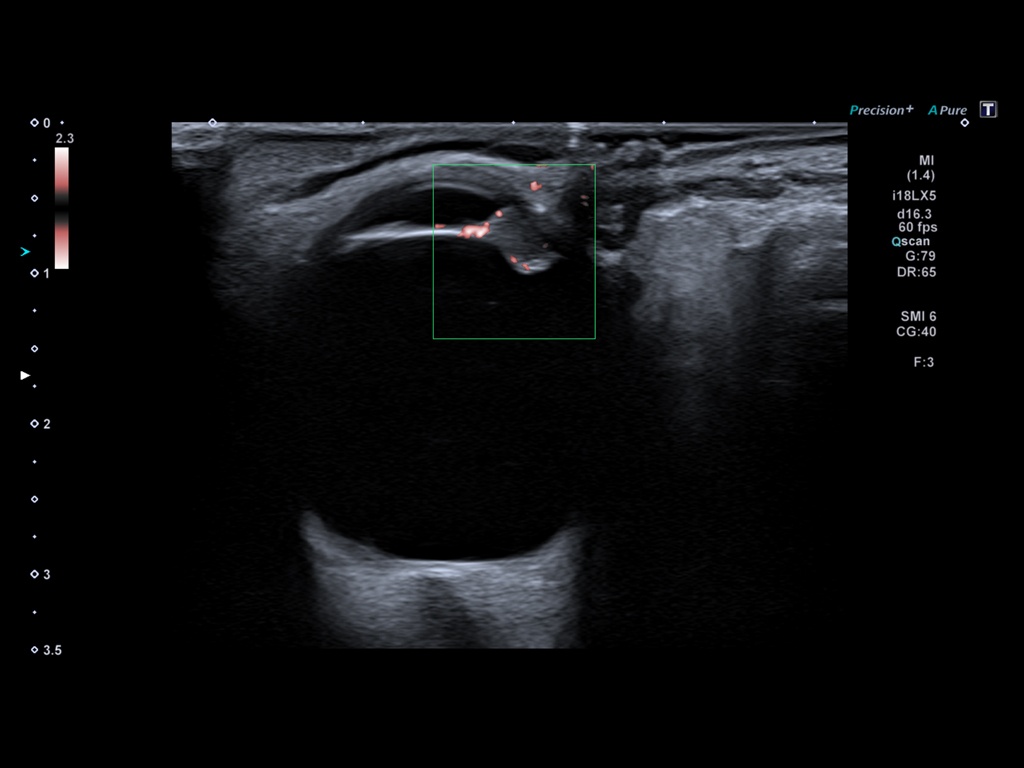
Video 1
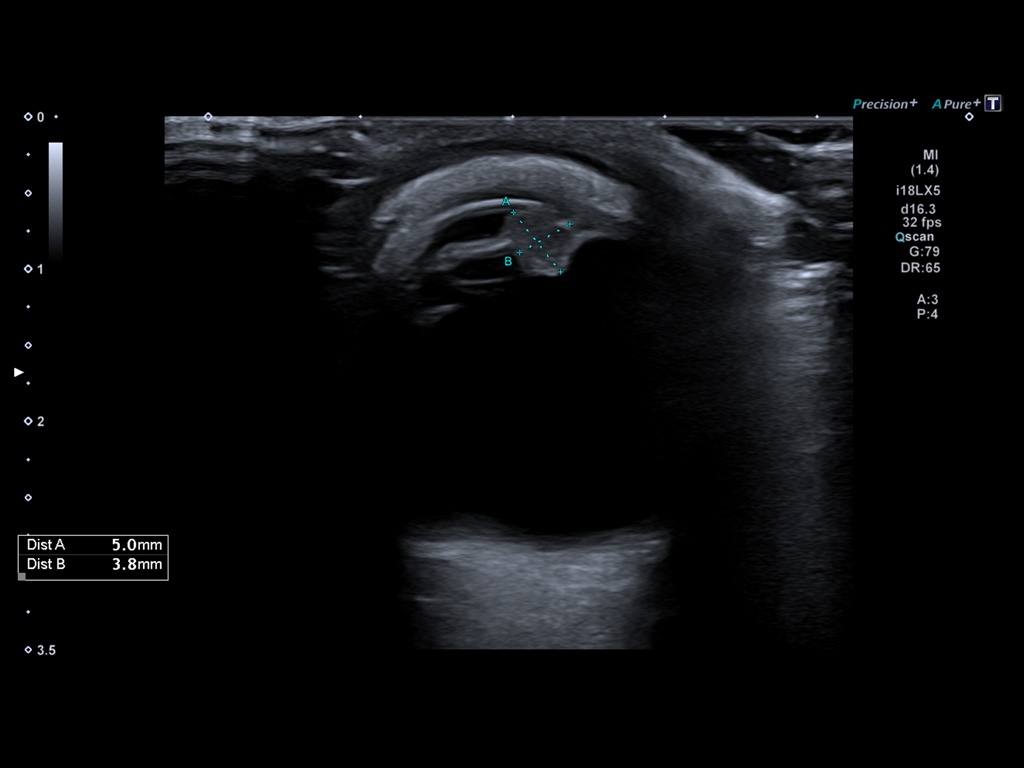
Video clip of the left orbit ultrasound scan, demonstrating a 5 mm mass of the iris extending antero-laterally and protruding both into the anterior and posterior chambers.
The patient himself had noticed it relatively long before that, but as he had not experienced any other symptoms, he only became concerned when the lesion increased in size.
Incidentally, the patient had had a computed tomography (CT) scan of the head (owing to unrelated, neurological symptoms) a few months prior to his presentation to the Ophthalmologist. In retrospect, the left globe lesion was just visible, but CT provided an inferior level of detail which was not diagnostic, in contradistinction to the superior anatomical detail delineated on ultrasound (Fig. 4).
Uveal melanoma (UM), being the most common primary intraocular tumour in adults, is an important pathology that needs to be considered when undertaking ultrasound examination of the orbit.
CLINICAL PERSPECTIVE:
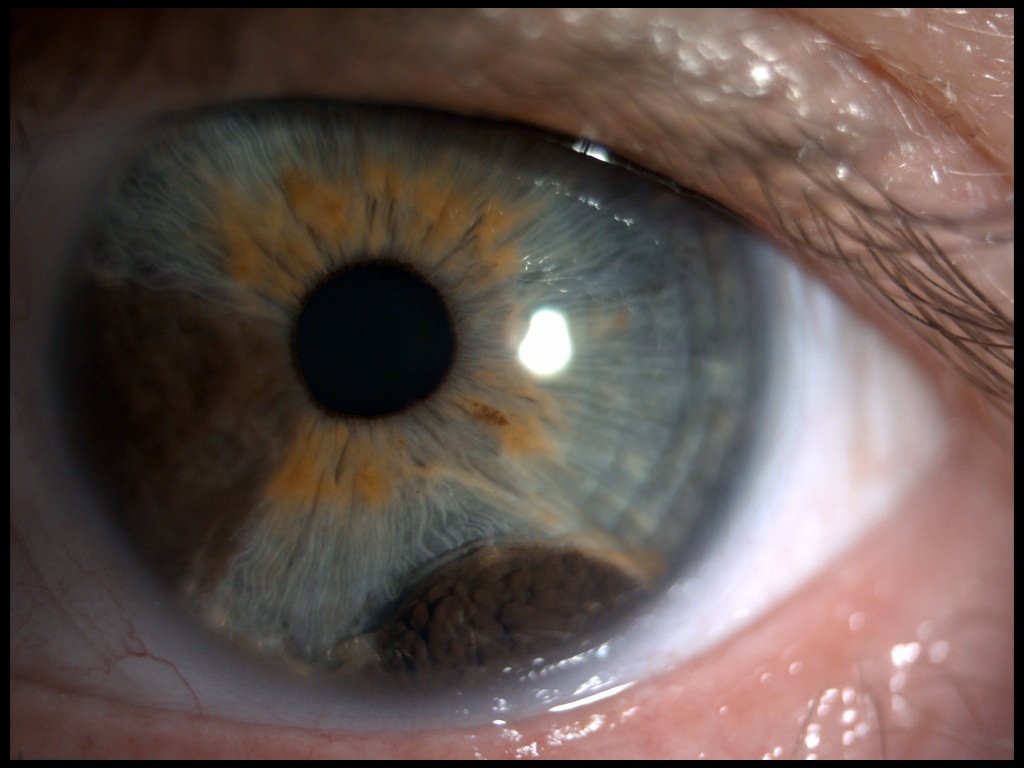
Sonographic assessment of UM has been well-established, and it is classically described as hyperechoic, dome-shaped lesion demonstrating acoustic hollowness and unlike benign lesion typically has some vascular flow. Subretinal fluid may also be present.
Certain imaging features that can be easily evaluated on ultrasound play central role in primary tumour (T) classification (e.g. thickness, largest basal diameter, involvement of ciliary body or extrascleral extension)(1).
Another notable contribution of ultrasound to the multimodal ocular oncology assessment is the ability to help distinguish UM from its most important differential: a choroidal nevus (benign pigmented lesion). As established by CL. Shields et al. on a retrospective review of 3806 consecutive choroidal nevi imaging cases, multimodal imaging can capture risk factors for malignant transformation of the nevus (2). These include lesion thickness >2mm and melanoma hollowness (low internal reflectivity), which is best evaluated on US.
There are other strengths that are unique for US among other diagnostic imaging modalities in the evaluation of intraocular tumours. These include superb spatial resolution, which allows for precise visualisation of fine intraocular structures. In addition, the latest advances in microflow imaging enable detection of small vessels and detailed characterisation of the tumour. As seen in our case, US can provide much more diagnostic information than CT and in some instances even MRI.
THERAPY PLANNING:
With the advent of novel, eye-conserving treatment options and individualised therapeutic modalities, the information ultrasound provides on tumour morphology is of great value to the Ophthalmologist.
It is worth noting that the value of US in patients suffering from UM is not limited to the primary tumour, which metastasizes most commonly to the liver. While older literature suggested that hepatic ultrasound had poor sensitivity in detecting liver metastases in UM, more recent studies found its high value in surveillance of the patients affected by this malignancy (3). MM. Choudhary et al. concluded that surveillance based on serial hepatic US scans and confirmatory imaging as needed offers high likelihood of detecting asymptomatic liver metastases in UM patients.
This highlights the importance of sonography, not only in the primary tumour evaluation, but also in the follow-up phase.
OUTCOME & PROGNOSIS:
Unfortunately, owing to the extent of tumour invasion it was decided that radical surgery would be the best treatment option and thus our patient underwent complete enucleation of the left globe.
Despite the aforementioned advances in treatment options, around half of the patients with uveal melanoma develop metastatic disease 10-15 years after initial diagnosis, which often leads to a fatal outcome.
- In certain instances, it can provide more diagnostic value than other cross-sectional imaging and it remains useful in the surveillance of UM patients.
2) Shields CL, Dalvin LA, Ancona-Lezama D, et al. Choroidal nevus imaging features in 3,806 cases and risk factors for transformation into melanoma in 2,355 cases: The 2020 Taylor R. Smith and Victor T. Curtin lecture. Retina. 2019;39(10):1840-1851.
3) Choudhary MM, Gupta A, Bena J, Emch T, Singh AD. Hepatic ultrasonography for surveillance in patients with uveal melanoma. JAMA Ophthalmol. 2016;134(2):174-180.